Backstory
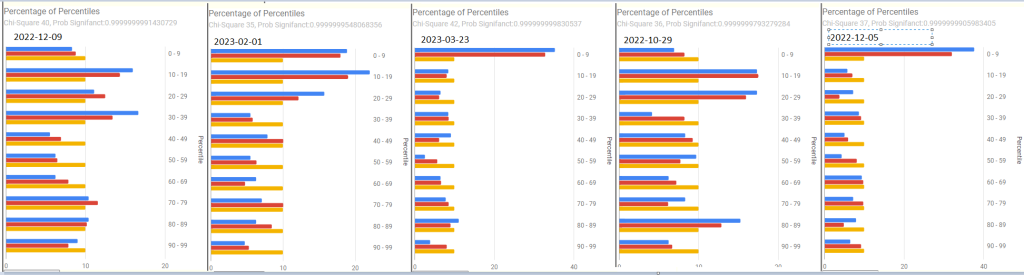
A sample result dated 29/10/2023 it’s for 19month old son born via C section and having lots of ongoing tummy pain since birth.
Fully breastfed for well over 12 months but the microbiome doesn’t appear that way.
Analysis
This is a very much “flying by the seats of my pants” analysis. Why? From birth for the next 10-20 years the microbiome has dramatic natural changes. The Fuzzy Logic Expert System on Microbiome Prescription is tuned for adults and not these age ranges. If you are dealing with a child, the approach below is suggested.
I am going to use ChatGPT selectively to make analysis easier, checking that it’s answers agree with my memories from reading studies..
So, first some literature to frame this analysis in. There are 400+ studies on C Sections and Infant microbiome.
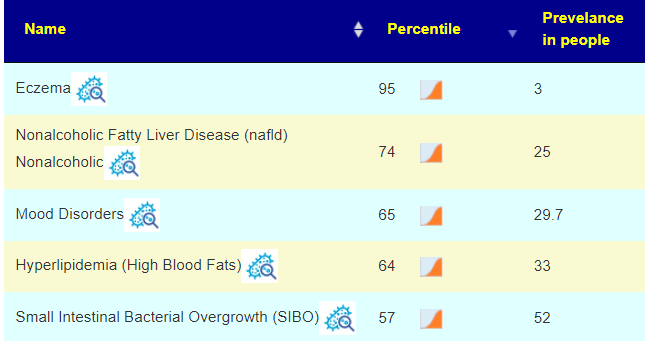
- “There is certainly a transient difference in the gut microbiota of infants born by Cesarean delivery compared to their VD counterparts. While this difference appears to be corrected after weaning, it may have lifelong impacts on the development of the immune system. ” [2018]
- “When comparing the gut microbiota composition of CSD babies with vaginally delivered (VD) babies, the former show a microbiome that closely resembles that found in the environment and the mother’s skin, while VD babies show a microbiome more similar to the vaginal microbiome. Although these alterations of normal gut microbiota establishment tend to disappear during the first months of life, they still affect host health in the mid–long term since CSD has been correlated with a higher risk of early life infections and non-transmissible diseases, such as inflammatory diseases, allergies, and metabolic diseases.” [2021]
- Too late, but important for any future babies “Lab analysis showed that the microbiota of the C-section babies swabbed with their mother’s vaginal fluids was close to that of vaginally born babies” [2021]
Bifidobacteria and Firmicutes Dominance: In healthy infants and toddlers, the gut microbiome often shows dominance of beneficial bacteria like Bifidobacteria and Firmicutes. These bacteria play crucial roles in digestion, immune system development, and protection against pathogens.
From ChatGpt
Generally, Bifidobacterium can comprise anywhere from 10% to 40% or more of the total gut microbial population in toddlers.
In healthy toddlers, Firmicutes can typically constitute a substantial portion of the gut microbiota, often ranging from around 30% to 60% or more of the total bacterial population
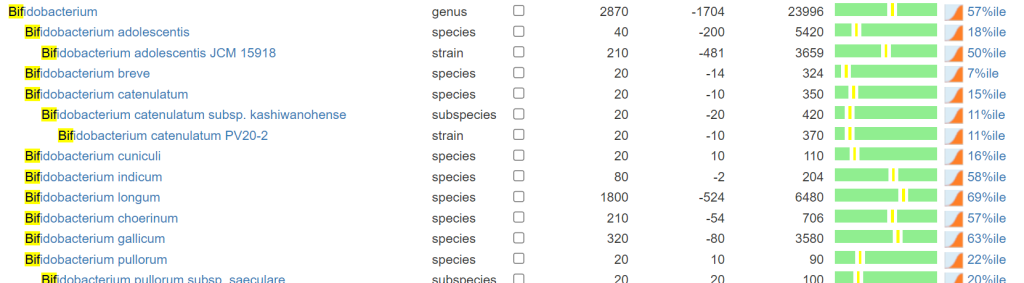
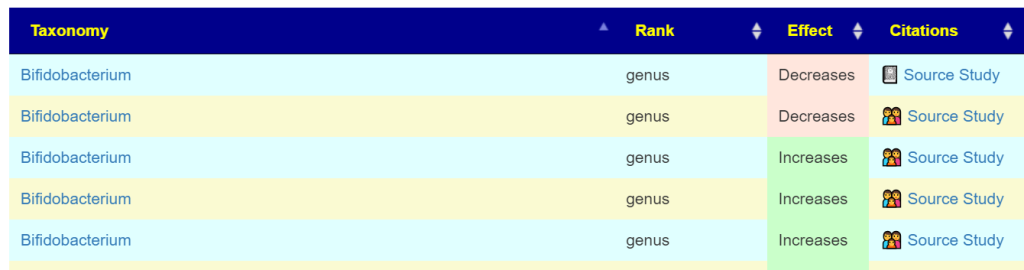
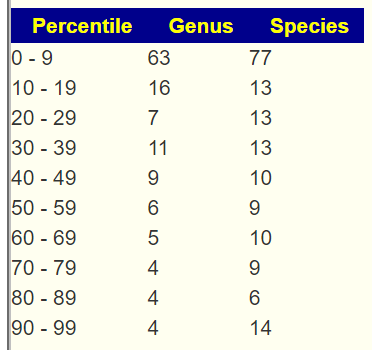
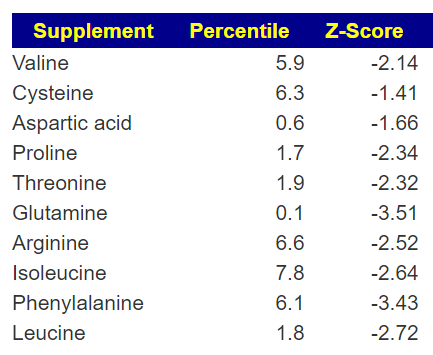
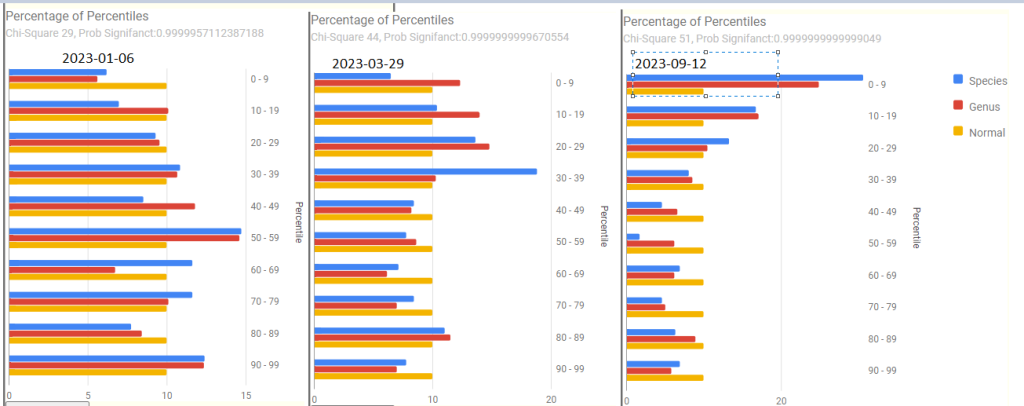
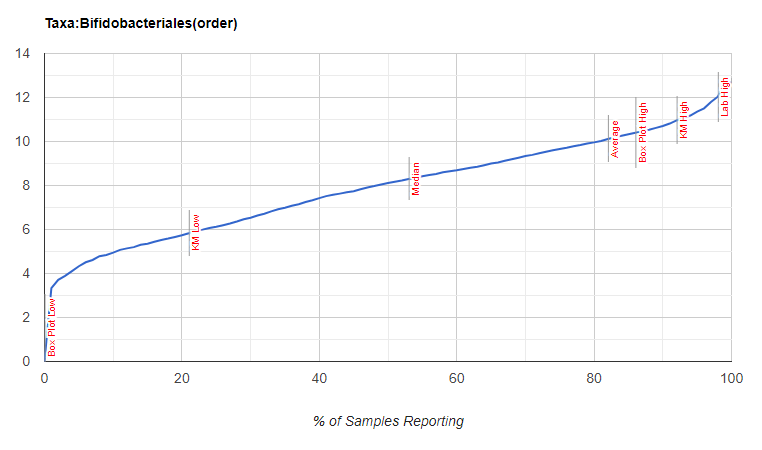
Looking at Bifidobacterium, the numbers are lower (57%ile) than expected for a child of this age but with a rich diversity of species. Bifidobacterium is 2.4%, well below the expected 10-40%. Bacillota (formerly known as Firmicutes at 83%ile) is 79.4%, well above expected 30-60%.
Switch to consequence, ChatGpt reports:
“Some of the health implications of low Bifidobacterium levels in toddlers may include:
- Digestive Issues: Bifidobacterium species contribute to the breakdown of complex carbohydrates, aiding in the digestion of certain fibers and sugars. Low levels of these bacteria may result in digestive problems such as constipation, diarrhea, or irregular bowel movements.
- Weakened Immune Function: Bifidobacterium species are involved in regulating and supporting the immune system. Insufficient levels of these beneficial bacteria may compromise the immune response, making toddlers more susceptible to infections and illnesses.
- Increased Risk of Allergies and Asthma: Some research suggests that alterations in the gut microbiota, including low levels of Bifidobacterium, might be associated with a higher risk of developing allergies and asthma in children.
- Potential Weight and Metabolic Effects: The gut microbiome, including Bifidobacterium, can influence metabolism and energy regulation. Low levels of these beneficial bacteria in toddlers’ gut microbiota might potentially be linked to metabolic issues or an increased risk of obesity later in life, although this connection is still an area of ongoing research.
- Impact on Neurodevelopment: Emerging studies suggest a possible link between the gut microbiota and brain development. Some evidence indicates that alterations in gut bacteria, including Bifidobacterium, might influence cognitive development and behavior in children.
- Susceptibility to Infections and Antibiotics: A decrease in beneficial bacteria like Bifidobacterium can leave the gut more vulnerable to colonization by harmful bacteria. Moreover, toddlers with low levels of these beneficial bacteria may face a higher risk of complications after antibiotic treatments, as antibiotics can further disrupt the delicate balance of the gut microbiota.
- Digestive Imbalances: In some cases, an overabundance of certain Firmicutes strains might affect the balance of gut microbiota and contribute to digestive problems, including irregular bowel movements, bloating, or discomfort.”
At this point, using the Fuzzy-Logic Expert System on Microbiome Prescription is not a good choice to get suggestions. It is tuned for adults and not toddlers. All of the values are in the normal range for an adult, but definitely out of range for a toddler.
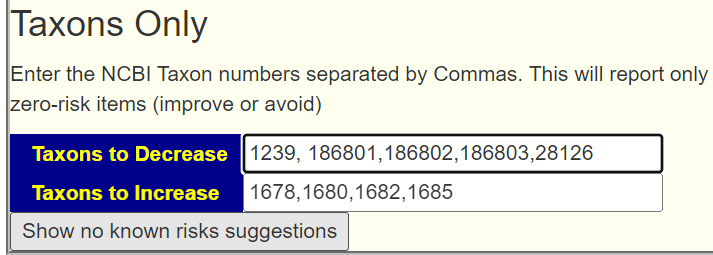
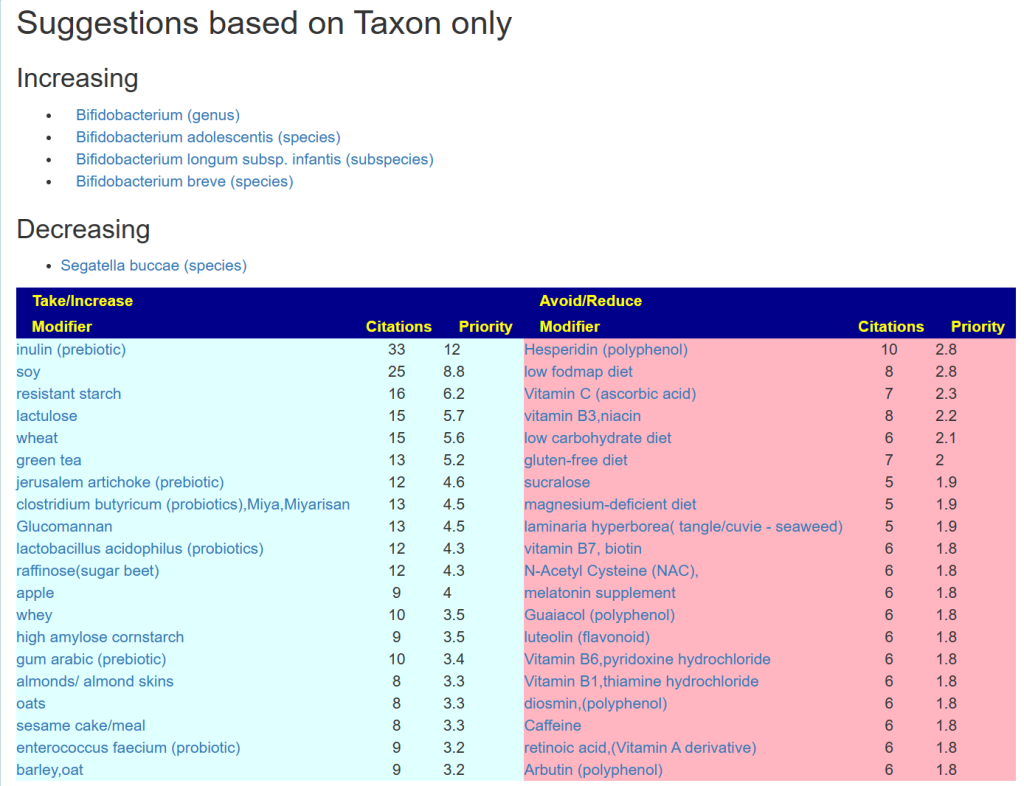
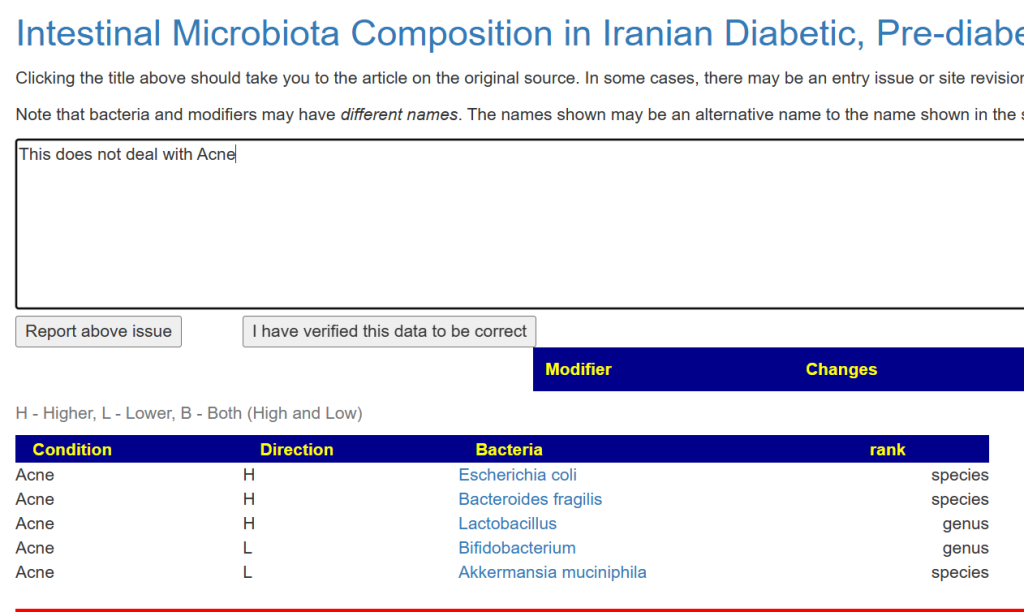
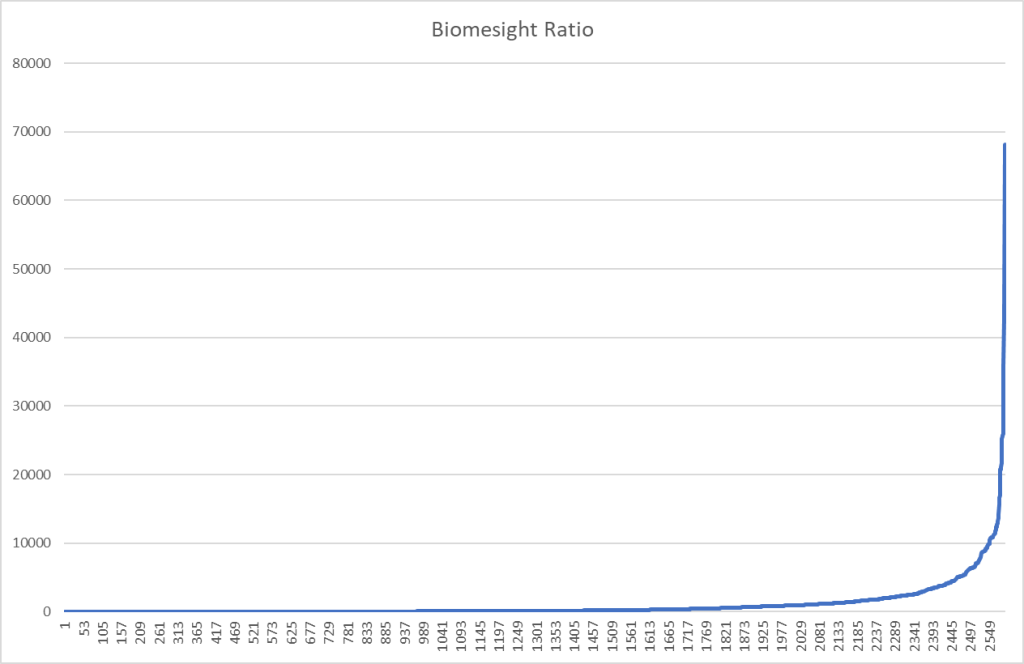
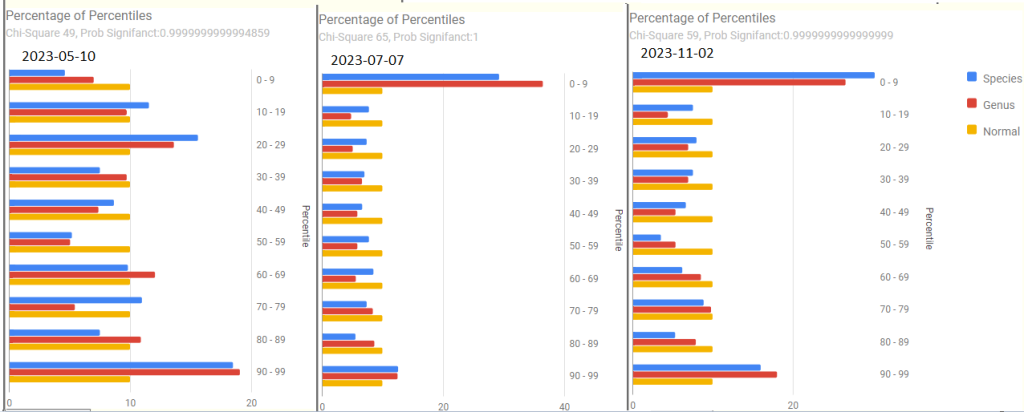
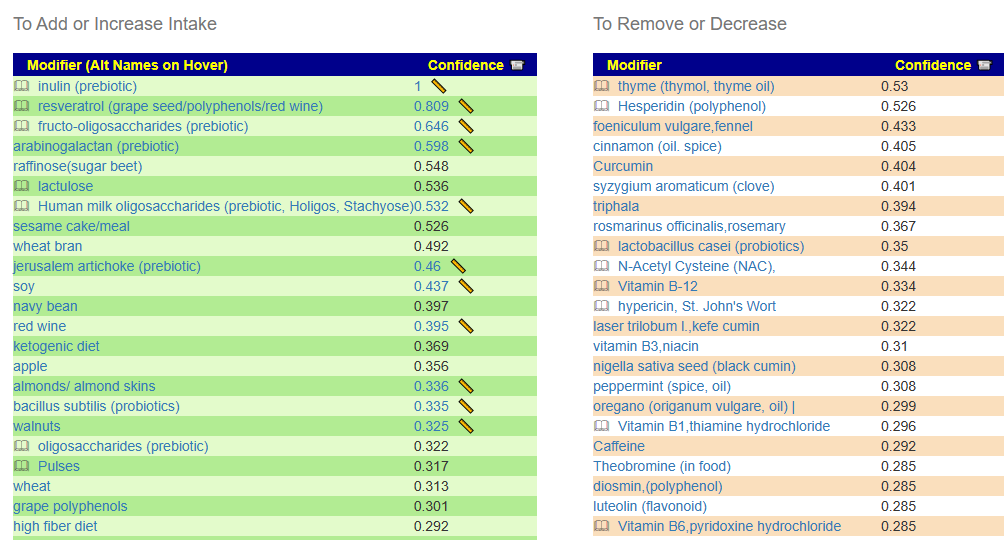
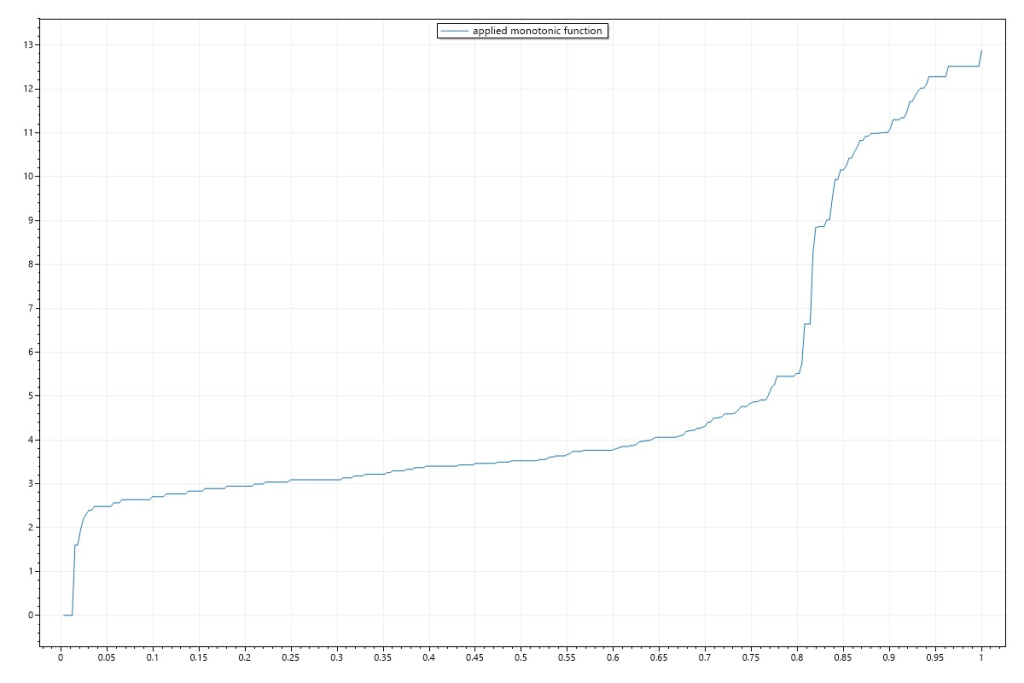
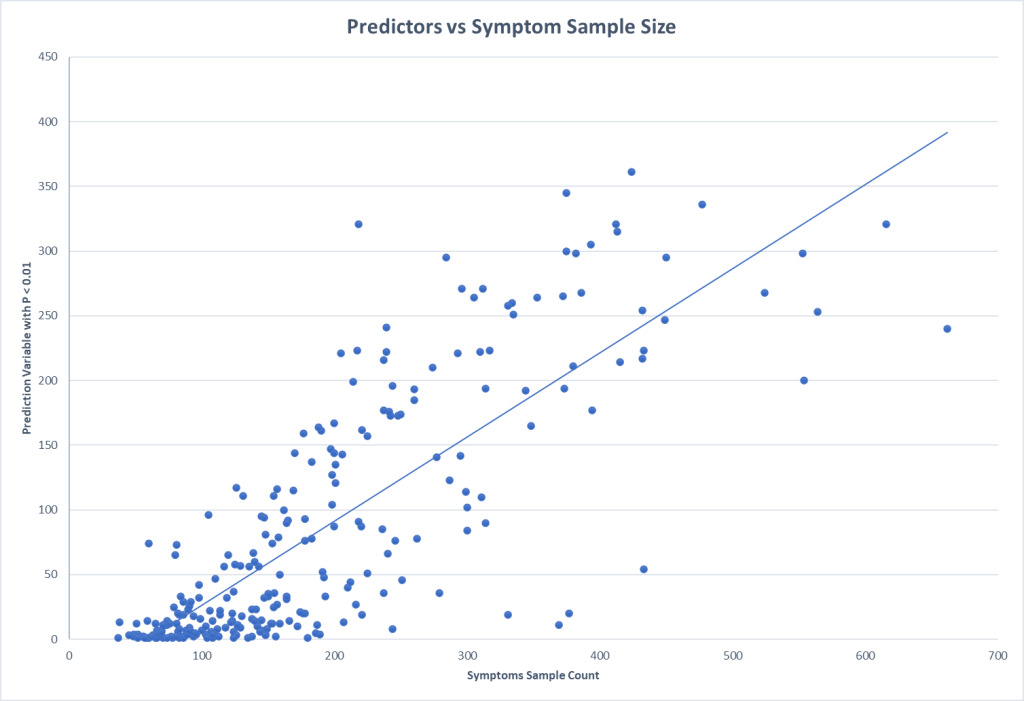
What we want is to increase one bacteria and decrease another bacteria without looking at the percentile. I just added a subsection on the Research Features tab to make that available. It requires the the taxon numbers be entered. In this case: Decrease: 1239, Increase 1678 (Bifidobacterium).
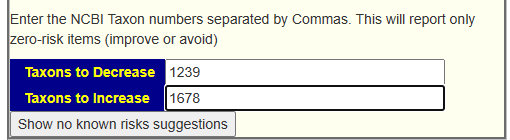
See this video for a walk thru of the process.
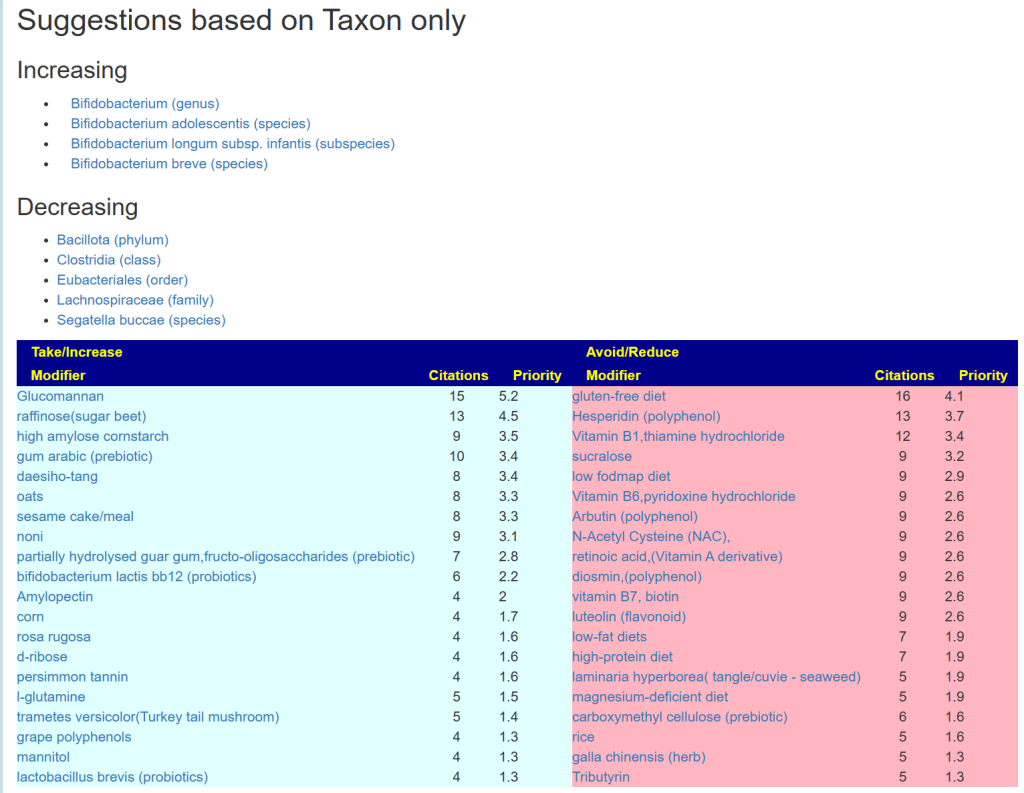
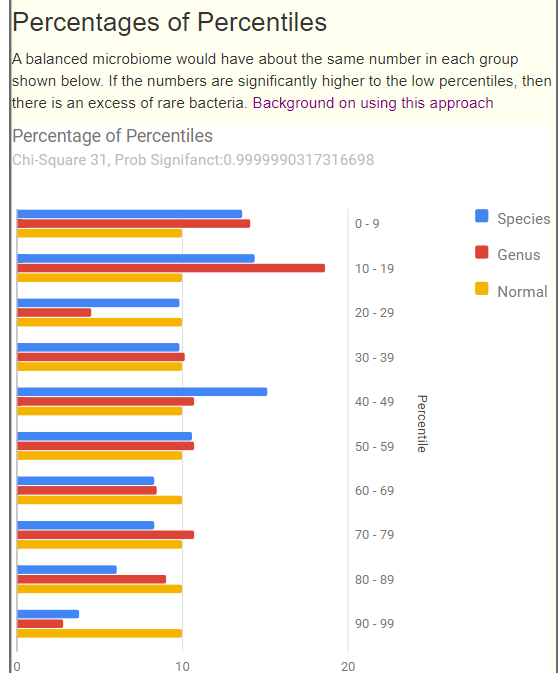
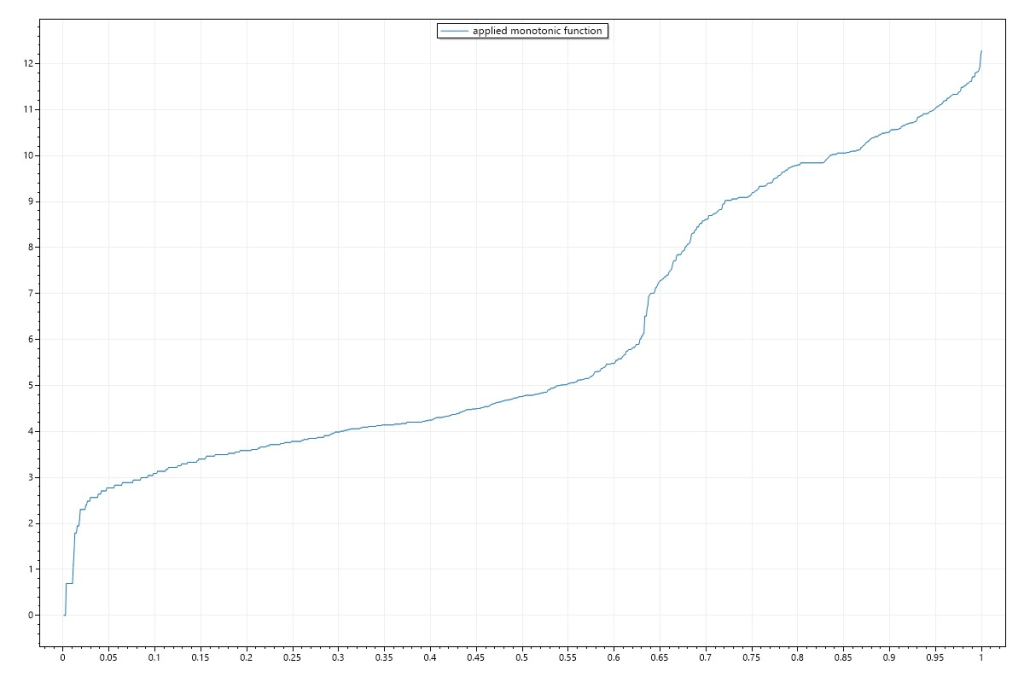
This results in this page
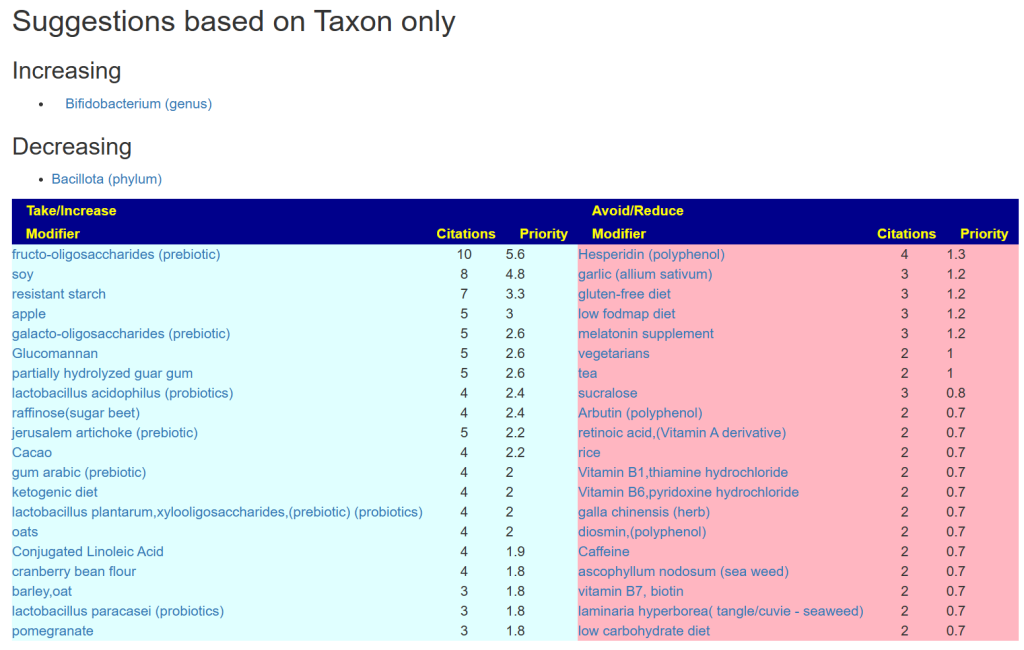
You can click on each modifier to verify that it only impacts the bacteria named by taxon in the desired way.
In toddlers, several Bifidobacterium species are commonly found in their gastrointestinal tract. Among these species, Bifidobacterium longum, Bifidobacterium breve, and Bifidobacterium infantis are frequently observed in the gut microbiota of toddlers. These species play essential roles in maintaining gut health, aiding in digestion, and supporting the immune system during early childhood.
ChatGPT
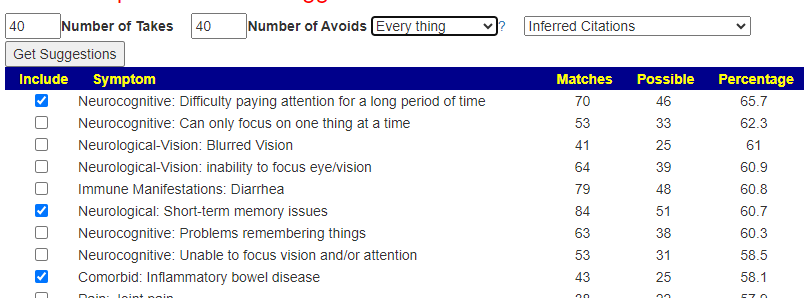
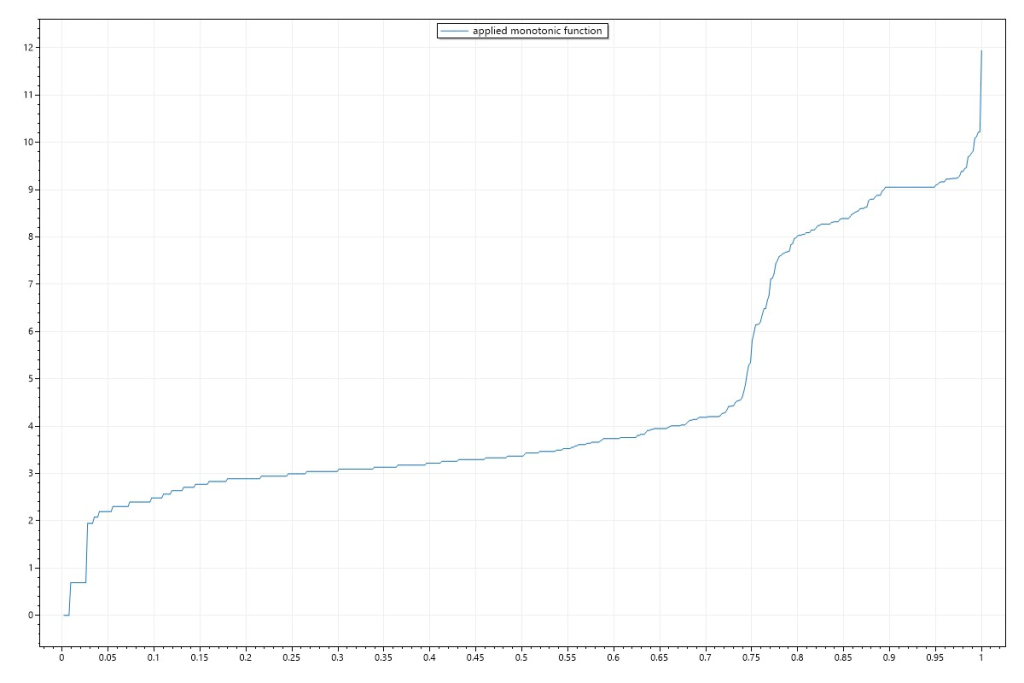
We can take this one step further, picking specific children :
- Increase: 1678,1680,1682,1685 (the usual toddler species)
- Decrease: 1239, 186801 (Clostridia), 186802 (Eubacteriales), 186803 (Lachnospiraceae) the biggest ones under Bacillota

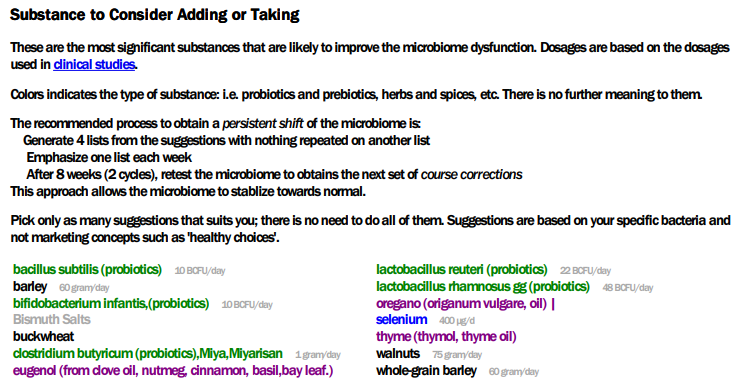
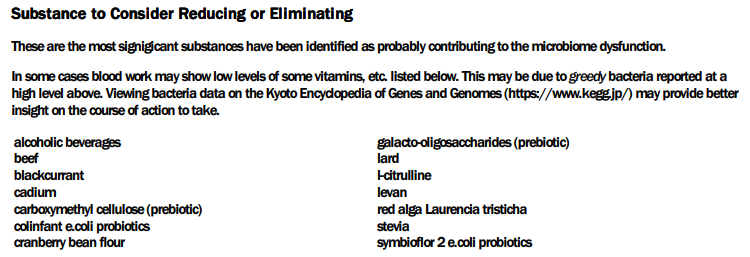
With a deeper set of suggestions:

Feed Back
I usually send drafts to the person for comments, concerns etc. This was the response:
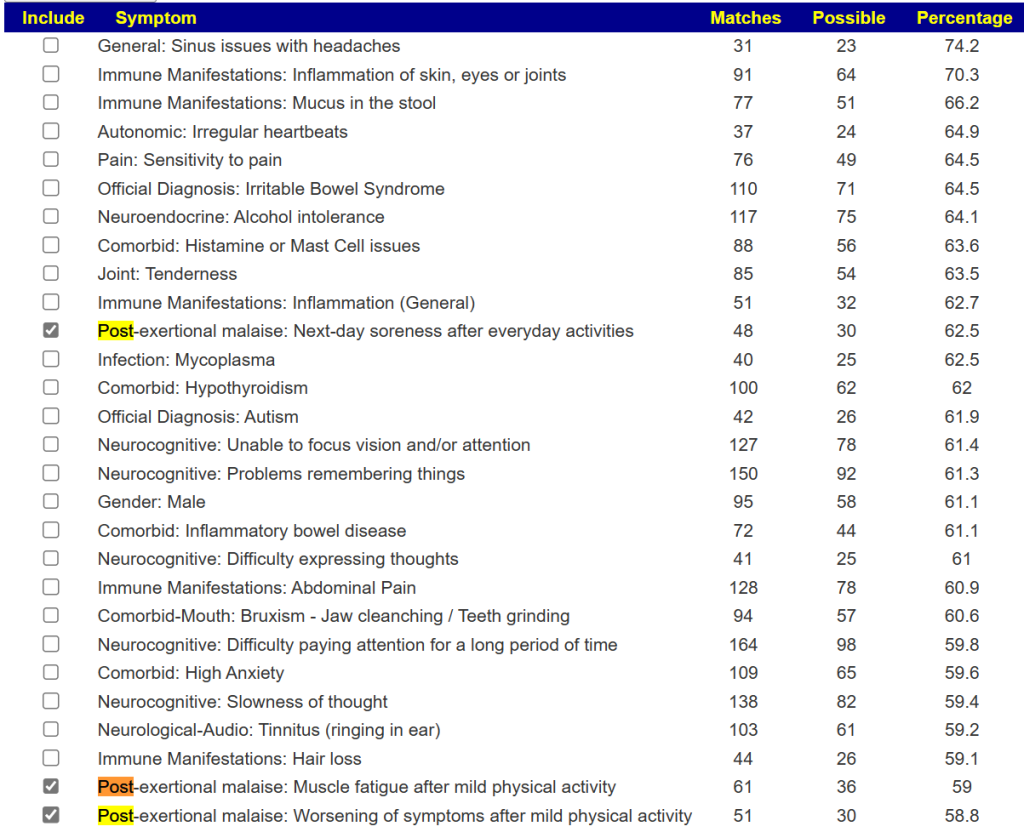
I wondered whether prevotella/segatella buccae was a concern as it was the highest species in the sample and bacteroides was extremely low. The practitioner we saw prescribed HMO and lactulose after reviewing Biomesight raw data.
Mother of child
The HMO suggestion is reasonable if you do not check all of the literature. We have contradictory results from studies for HMO. Remember Bacillota is the modern name for Firmicutes.
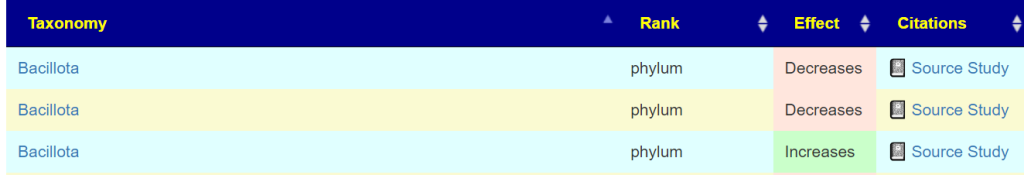
Similarly, we have some contradiction in results with Bifidobacterium — so it was not deemed ultra safe.
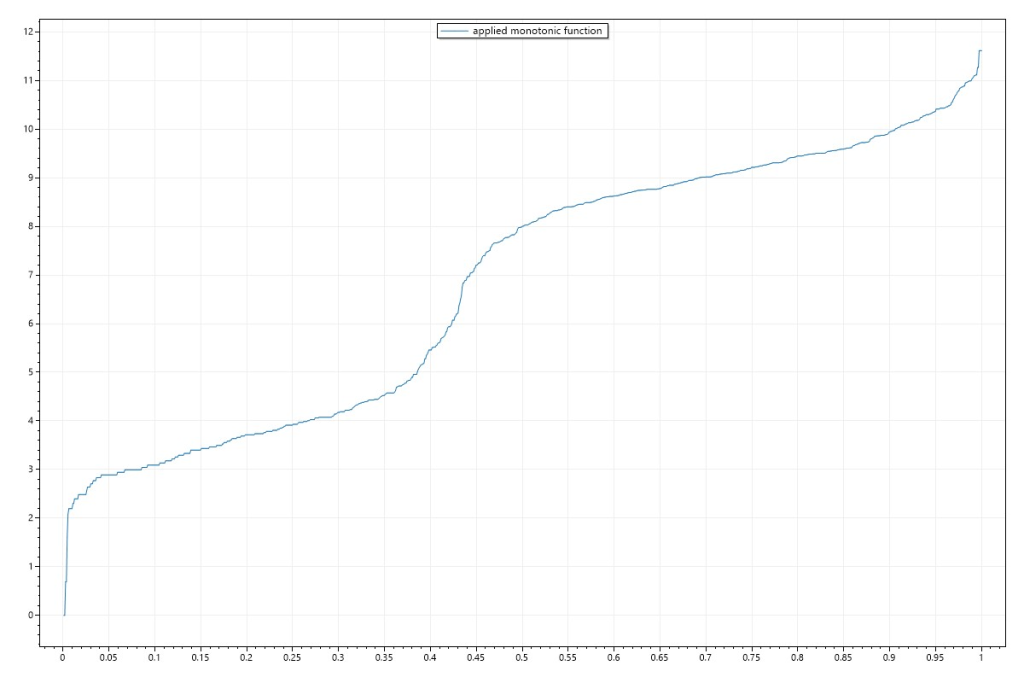
This suggests adding segatella buccae (NCBI 28126) be added.
The results are similar, with less items on the to avoid.
Trying a different combinations, for example
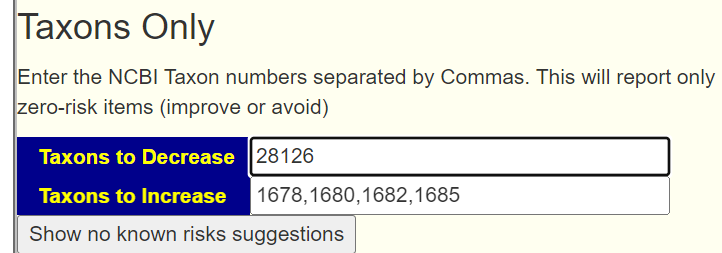
We get different ordering and a few changes.
Bottom Line
We have various sets of suggestions, doing a consensus is likely the best path forward.
Postscript – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I can compute items to take, those computations do not provide information on rotations etc.
I cannot tell people what they should take or not take. I can inform people items that have better odds of improving their microbiome as a results on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting.
The answers above describe my logic and thinking and is not intended to give advice to this person or any one. Always review with your knowledgeable medical professional.Posted on b




Recent Comments