Backstory
Much longer and detailed than usual. Most of the data is “outside of my wheelhouse” of expertise, but readers may have additional insight.
- 22 Years ago, I had a UTI. It wouldn’t go. I had 5 antibiotics. None of them worked. By the sixth week I was beside myself. A new doctor gave me ciprofloxacin. Finally it went away. Unfortunately, being naïve and a bit dumb back in the day, I started drinking alcohol the following weekend and the UTI came back. I didn’t realize but the bladder lining was weakened and presumably still some residual bacteria there. They got to work again.
- I had ciprofloxacin again. 7 day course. My bladder sort of got back to normal but I had to drink more water than usual to stop it from feeling uncomfortable. This lasted four years. I could pee normally, everything was good but I was always conscious things weren’t quite the same as they had been. I stopped drinking alcohol completely.
- NB: I developed hay fever pretty immediately after finishing the second course of Cipro. I believe something got knocked out of my microbiome that I’ve never got back.
- After a period of huge stress at the age of 30, my bladder suddenly got very hot and tight and uncomfortable. Numerous tests showed no infection. I was offered a urethal stretch. This worked to some extent but I then landed in a pattern that lasted 18 years:
- From days 5-14 of my cycle my bladder would feel like I had a UTI. But from days 15 – 28 and then days 1 – 4, I had pretty much no symptoms. My bladder during non-high estrogen days was good. My bladder was like normal. I could eat all foods and drink alcohol somewhat.
- However I did have to be careful. I couldn’t drink every night (not that I would anyway) and citrus, black tea, coffee, I had to wary. Too much and it would set things off. Same with stress. High stress periods would see my bladder get very hot and tight and it would take weeks for it to calm back down.
- During this 18 year period, I found this pattern that on estrogen-high phases my bladder would go off, feel like a UTI, reduced flow, more frequency, but once progesterone kicked in, everything was fine. During low hormone times, during my period, my bladder was best of all. Worked perfectly.
- Two years ago I found out I have osteoporosis. I trialed HRT, using estradiol gel. Within 24 hours, my bladder was very very unhappy. I felt like I needed to pee constantly. Tiny amounts. It was far worse than during my own cycle of estrogen.
- I stopped on day 20 because it was so uncomfortable. I really wanted to take the estrogen but I couldn’t. . But I don’t seem to be able to do this. I believe this messing with my hormones sent me straight into much stronger menopause symptoms. I suddenly gained weight around my middle (sign of leaky gut, low estrogen unable to keep the intestinal junctions tight) and my spine and sternum started to ache like they never had before. Brain fog, terrible sleep, frequency of peeing but this time for no reason, just bladder more sensitive overall.
- I trialed progesterone only this summer, in the hope that it helps my bladder usually – well my own progesterone seems to. However after a while the familiar burning and uncomfortable feeling came back. It seems like external hormones aren’t for me.
- I have rosacea on one cheek.
- I have got telogen effluvium [hair loss] which started 2.5 months ago.
- Prof XXXX from Imperial ran a DAO blood test on me and it came out at 8 U/mL. He said this shows I’m am histamine intolerant.
- I’m currently taking Hydroxyzine 25mg per day at night to calm my bladder down as it had another ‘episode’ this summer. Too much stress again.
- I think I have mast cell activation syndrome in my bladder. Prof says the same. I think estrogen kicks of the degranulation sequence and my immune pathways/signaling have got messed up. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3537328/, https://www.mdpi.com/1422-0067/19/6/1554
- He trialed me on ketotifen but it made things worse. 5% of users can get cystitis type symptoms. Looks like I was one of them.
- He now wants me to trial Famotidine (stomach acid suppressant) and Loratadine to switch off H1 and H2 receptors. I’m reluctant to do that. He also thinks I may have a staph epidermis infection but I find this hard to believe because my bladder goes through very good periods for months at a time – it’s only with stress or estrogen that things get bad. It’s true to say though that with every period of stress, my bladder loses function and so now, it’s harder to get all the urine out. It is inflamed at the base, the ultrasound showed.
- He’s prescribed Nitrofurantoin twice per day for 2 weeks. I’m really reluctant to take yet more antibiotics.
- Additionally I’ve been diagnosed with stage 2 kidney disease just recently, sightly high creatinine and just on the cusp range of too high for calcium too in the blood.
- I am low in Vitamin D, just below normal. I am low in ferritin from a recent blood test in August. I am trying to correct these two with supplements the last few weeks but I know it takes time.
- I feel overall I’m inflamed. I feel like I don’t absorb things as well as I used to. I don’t sleep very well.
- Taking hydroxyzine helps with the aches in my spine and sternum. They have almost gone away. Nice side effect but I know antihistamines are not good long term. I see Fexofenadine seems to do the same thing too https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8421647/
I’d like to get to the stage where maybe I could take the hormones to protect my bones? At least have the choice.
Analysis
We have actually two samples taken a few weeks apart. Technically, there was a little improvement between the samples (one had 9 “9” and the other just 8 “9”).
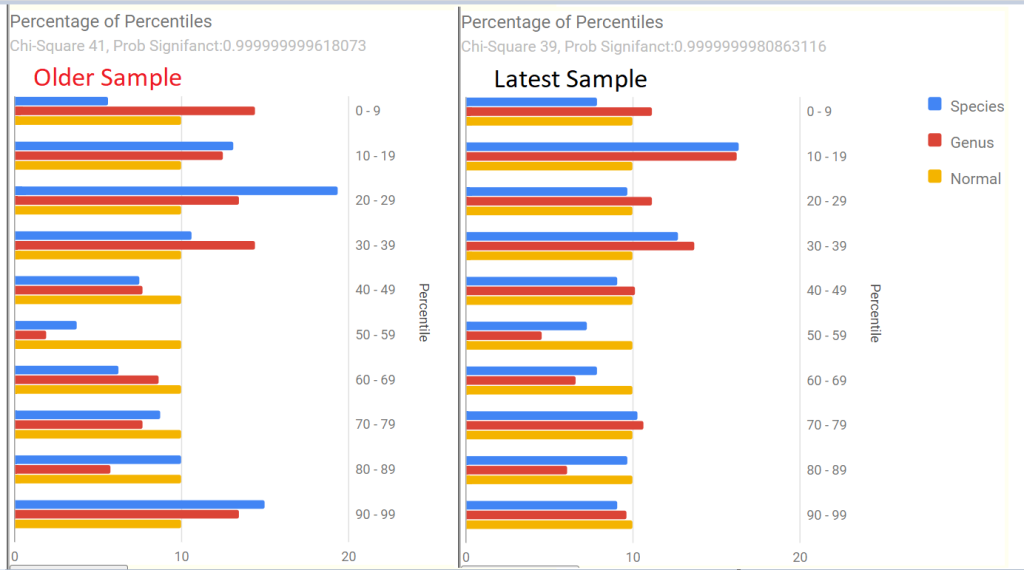
Both samples had similar profile with Dr. Jason Hawrelak Recommendations. With the following significant items:
- Too high: Akkermansia,Bacteroides, Methanobrevibacter
- Too low: Bifidobacterium, Roseburia,Bilophila wadsworthia (was too high prior), Faecalibacterium prausnitzii
- Anti inflammatory Bacteria Score: 43%ile, Prior was 31%ile
Bacteria deemed Unhealthy had several items of interest:
- Bacteroides uniformis: 100%ile (100%ile prior) – 16% of the microbiome (was 18% prior)
- Bacteroides fragilis: 100% (99%ile prior) – 9% of the microbiome (was 7% prior)
Potential Medical Conditions Detected use pattern matching to published studies. We have the following items of note:
- hypertension (High Blood Pressure) risk
- Hyperlipidemia (High Blood Fats) risk
- Prior sample also had: Allergies risk and Colorectal Cancer risk.
Special Studies pattern matching (using other samples uploaded with their declared symptoms) had only one strong match: COVID19 (Long Hauler), with a weaker match for Allergies And Food Sensitivity. The person had COVID but appears to be full required (no symptoms for long hauler).
Going Forward
There are many things happening with this person. There are no really strong microbiome pattern matches for the main symptoms of concern, so I will just work from the standard “just give me suggestions” on each sample and then do an uber-consensus. Every microbiome report has some fuzz factors in measurements, combining two or more (close in time) reduces the noise from the fuzz.
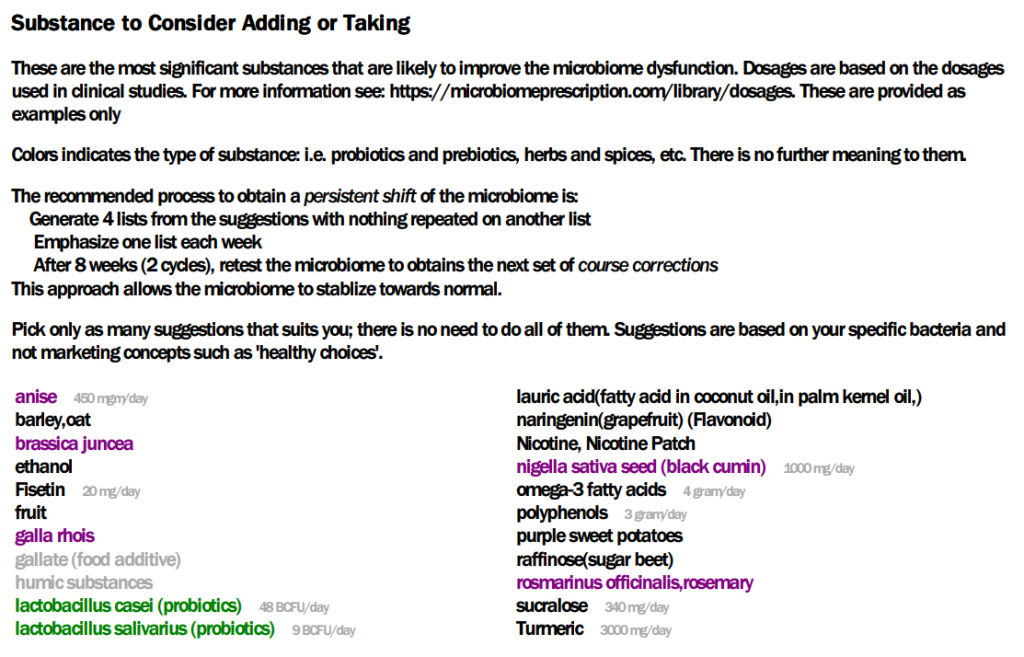
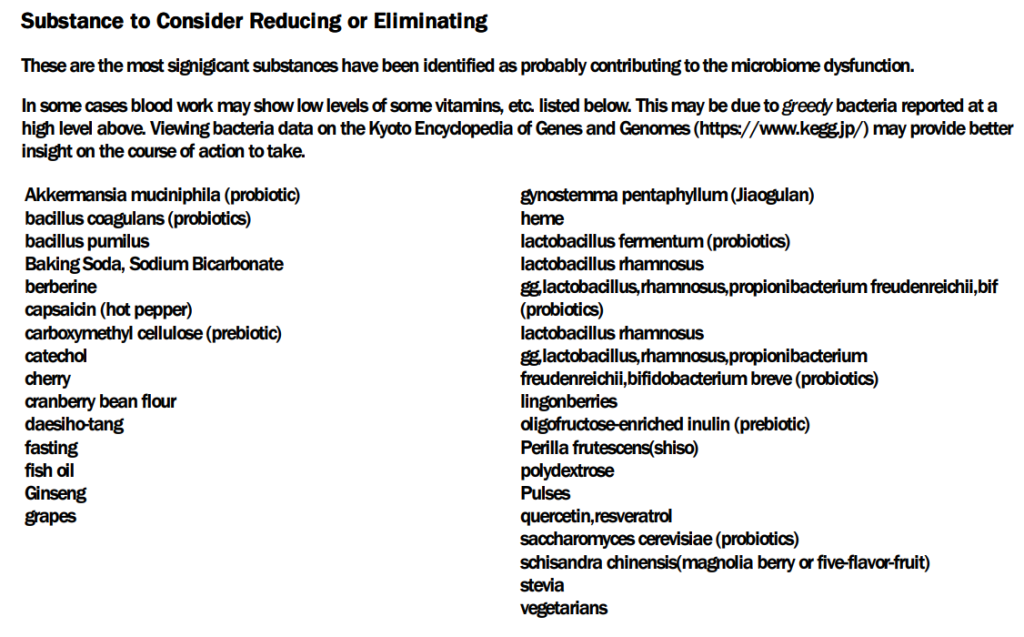
The highest priority was 470 and the lowest was -543. Applying the 50% rule, we will focus on items over 235 or below -272.
Some interpretation notes:
- Avoid being a vegetarian does not mean avoid vegetables. It means have some fish or meat.
- Fruit is a take with some specific fruits being an avoid (cherry, grapes, lingonberries). Coconuts and Grapefruits
- Avoid fish oil is not inconsistent with taking omega-3 fatty acid. See this listing of what is in fish oil. So beware of supplements saying “high in omega-3” that is effectively fish oil. An example of a non fish oil source of Omega-3.

Review of Previous Consumptions
Items between -272 and 235 are unlikely to cause a significant contribution and likely complicates life without a clear benefit. All of the items cited fall in this indifference range.
- ciprofloxacin (antibiotic)s: 203
- hydroxyzine dihydrochloride,(prescription): 129
- ketotifen fumarate,(prescription): 129
- progesterone,(prescription): 129
- famotidine,(prescription): 132
- nitrofurantoin (antibiotic): 162
- vitamin d: -233
- Ferric citrate(iron): -157
- brown rice: 104
- oats: 34
- Coffee: 138, teas: -50 to 176 depending on type
- Cacao: 169
- Cacoa flavonoids: -19
I also decided to look at the top prescription items as a discussion point with your MD. I have a hypothesis that many prescription items work via their impact on the microbiome. This leads down a speculation path that conditions associated to the top recommended prescription items may be in a pre-significant state — a potential developing risk.
I found what appear to be an association to be aware of. The earlier sample had a pattern matching to a form of cancer.
- daunorubicin hydrochloride,(prescription): 470, an anthracycline antibiotic mainly used to treat various types of cancers, especially leukemias.
- cefoxitin (antibiotic)s: 421 – often used with cancer patients [1979]
- moxifloxacin (antibiotic): 417 – “Moxifloxacin is an orally administrated fourth‐generation quinolone with broad‐spectrum coverage against tumor‐associated bacteria” [2020]
- doxorubicin hydrochloride,(prescription): 327 – “Doxorubicin is an antibiotic derived from the Streptomyces peucetius bacterium. It has had wide use as a chemotherapeutic agent since the 1960s. ” [NIH]
- pentamidine isethionate,(prescription): 351 – Repurposing pentamidine for cancer immunotherapy by targeting the PD1/PD-L1 immune checkpoint [2023]
Questions
Q: Can I ask – would you consider taking any pre-biotics? Not probiotics but prebiotics? I’m looking at HMOs and PHGG? For increasing bifido? Not sure if this is a good idea…
- A: There are no prebiotics that makes it over the threshold for good odds to help. The two that you cite are both negative.
- The suggestions are based on considering the impact on all abnormal bacteria. Trying to fix just one bacteria can often result in other bacteria being made worse. I looked at PHGG and found this 2021 study:
- Increases Bacteroides fragilis – partially hydrolysed guar gum
- Increases Bacteroides uniformis – partially hydrolysed guar gum
- You are at 100%ile for both of these…. you do not want to feed them more!
Q: I wasn’t sure from what was written in the article if I should be seeking an antibiotic to reduce down the fragilis and uniformis?
- A:
- IMHO, we should try non-antibiotic methods first. Often they may require minor diet changes that may become established and keep them away.
If after 2 months and a retest show no improvement, then it is time to start negotiating with your MD. This means reaching an agreement on an antibiotic that addresses them BUT does not make your gut worse… To get the first choice list of antibiotics, just click this button.
NOTE: Not all are suitable. Some are for vet usage, others may be injected only, etc. Your MD has to evaluate them.
Postscript – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I can compute items to take, those computations do not provide solid information on rotations, dosages, etc.
I cannot tell people what they should take or not take. I can inform people items that have better odds of improving their microbiome as a results on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting. Some suggestions may be counterindicated for other medications you are taking and medical conditions.
The answers above describe my logic and thinking and is not intended to give advice to this person or any one. Always review with your knowledgeable medical professional.
Recent Comments