Backstory
I’m in my early thirties and I caught COVID in November 2022. I’ve had dizziness from the beginning which is slowly going away, shortness of breath which is going away, weakness and pains all across my body, numbness, and this general feeling of derealization. Some days it felt I couldn’t even walk up the stairs. After extensive testing it was revealed that i had EBV reactivated, toxic mold, and whatever damage was left from long COVID. The big symptom that I’m still dealing with to this day are some sort of MCAS presentation where when i eat high histamine foods, exercise, sauna, or go for too long of a walk my throat will get tight, which is pretty scary. I also get dizzier upon anaerobic exercise.
For other analysis for Long COVID click here.
Analysis
We again see the typical pattern for Long COVID and ME/CFS. Over representation of the 0-9%ile. For more information see Background on using this approach
| Percentile | Genus | Species |
|---|---|---|
| 0 – 9 | 77 | 101 |
| 10 – 19 | 24 | 20 |
| 20 – 29 | 16 | 18 |
| 30 – 39 | 11 | 18 |
| 40 – 49 | 12 | 27 |
| 50 – 59 | 12 | 19 |
| 60 – 69 | 15 | 12 |
| 70 – 79 | 4 | 15 |
| 80 – 89 | 13 | 19 |
| 90 – 99 | 19 | 24 |
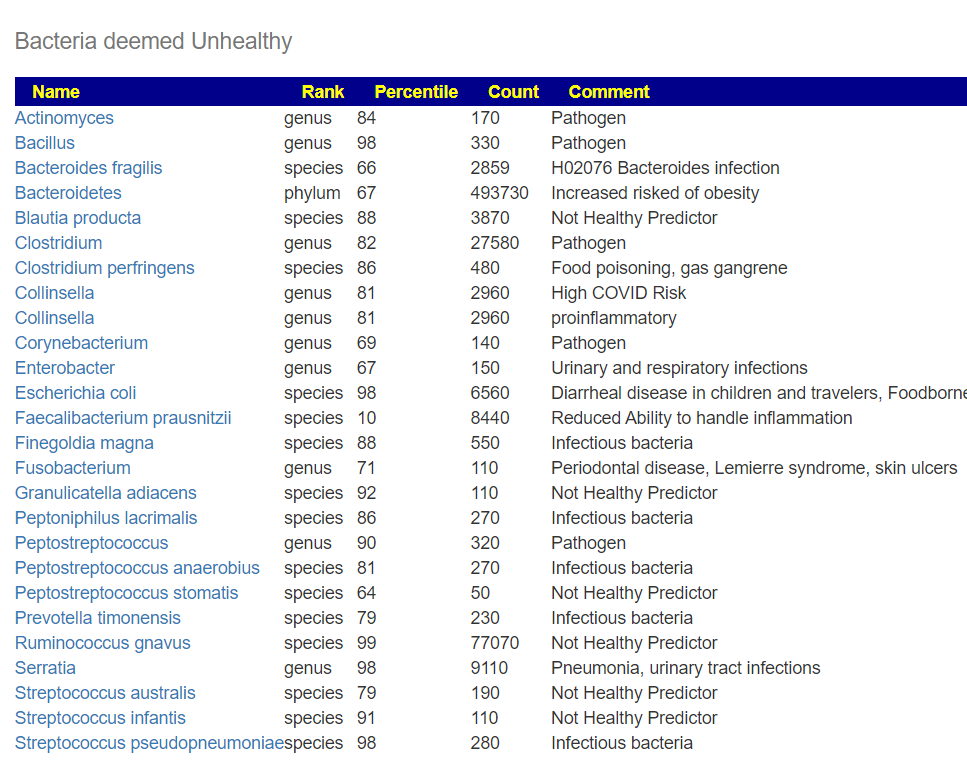
In this case we see a number of bacteria flagged as likely causes of the above.
| Rank | Bacteria | Importance | Percentile |
|---|---|---|---|
| genus | Bacteroides | 4 | 95%ile |
| species | Bacteroides stercoris | 3.2 | 100%ile |
| species | Phocaeicola vulgatus | 3 | 94%ile |
| genus | Ruminococcus | 2.7 | 93%ile |
| genus | Mediterraneibacter | 2.2 | 99%ile |
| species | Ruminococcus gnavus | 2.2 | 99%ile |
| genus | Escherichia | 2.2 | 99%ile |
| genus | Mitsuokella | 2.1 | 100%ile |
| species | Mitsuokella multacida | 2 | 100%ile |
Comparing to the COVID Literature
Going over to Understanding the Relationship of the Human Bacteriome with COVID-19 Severity and Recovery [2023] We see the following cited as being higher: Mediterraneibacter. And Gut microbiota and COVID‐19: A systematic review [2023] cites higher Bacteroides stercoris, Phocaeicola vulgatus, Ruminococcus, Ruminococcus gnavus, Escherichia. Interesting that Gut microbiota in COVID-19: new insights from inside [2023] cites that Mitsuokella decreases with recovery. Our hope is that we will see this drop with our suggestions – there is only one known reducer: Nicotine.
Looking at the standard quick health overviews, we see a massive number of bacteria of concerns. While many are of low count, they are much higher than usually seen. This is in agreement with the over representation of the 0-9%ile range.
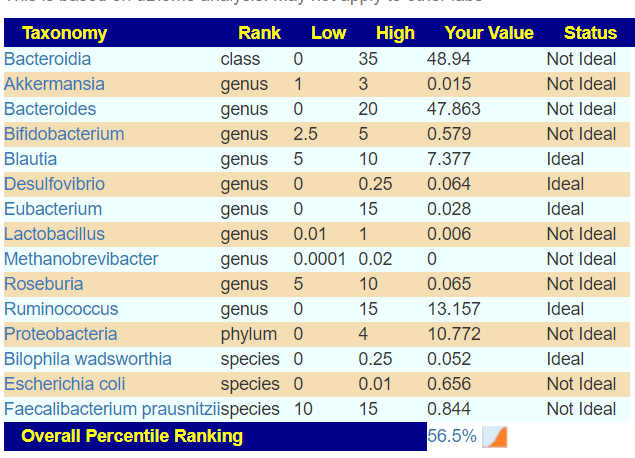
We see similar red flags with Dr. Jason Hawrelak Recommendations
Going Forward
There are so many items of concern that most practitioners would really not know where to start. Fortunately, the Artificial Intelligence engine was built to handle such complexities. Doing the quick route, I clicked the “Just Give Me Suggestions” and then click on the more technical details which takes us over to the consensus report.
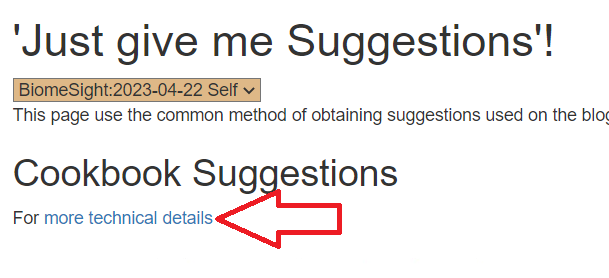
The Consensus Report is done using all possible modifiers, including antibiotics and prescription drugs (that we have information on their microbiome impact). The quick suggests auto-picks items commonly used in treating ME/CFS and Long COVID.
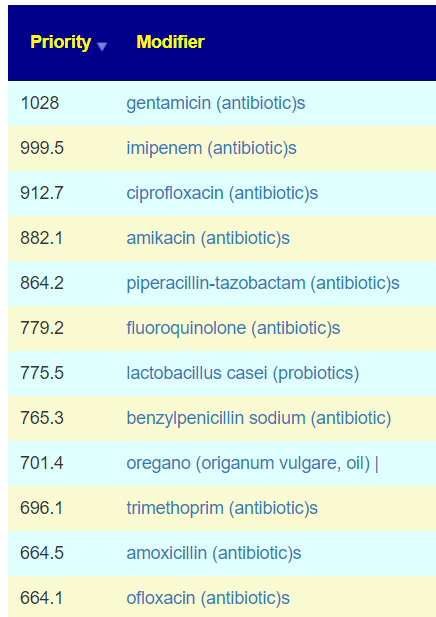
The top suggestions are high in antibiotics, which is atypical.
Getting antibiotic prescribed off-label is a challenge.
Reader’s Question: “Any idea how to go about getting those prescription antibiotics? “
Ideally, you can get your primary care physician to be willing to prescribe one of those above. It does not need to be the first one. If the physician suggests something not on the list, use the filter feature to see it estimated benefit. Negotiate. I attach an article on Long COVID from this week’s edition of New Scientist.
Some practitioners may be uncooperative — there are several alternative approaches.
- Look for a naturopath or MD that deals with Lyme infections. It is unlikely that you have Lyme BUT the gut disruption will often result in some Lyme tests returning a false positive. Getting that positive, even a weak one, will rationalize to that practitioner the prescription of antibiotics. Some of those listed above are used by Lyme physicians.
- The following are not recommended but people have reported doing these approaches:
- If you live near the Mexican border, many of the antibiotics are available there without prescription.
- See if you can order directly from Vet Supply shops
- If you have friends travelling to Mexico (or India or many 3rd world countries), they could buy at local pharmacies and bring it home to you.
- The best way is always under medical supervision!
How to explain to your MD on how these suggestions are computed?
We have been developing an Artificial Intelligence program based on the pattern of the 1972 MYCIN system developed by Stanford University in California. Unlike the popular AI systems based on machine learning or large language models (Chat GPT), we use Probabilistic Inductive Logic Programming with over a million facts manually curated from the U.S. National Library of Medicine.
LInks to more information are in above quote
Not walking the Prescription Path
Fortunately, we also have some herbs and species listed near the top. These include the following
- oregano (origanum vulgare, oil)
- thyme (thymol, thyme oil)
- garlic (allium sativum)
- syzygium aromaticum (clove)
- foeniculum vulgare (Fennel)
- neem
And a few specific probiotics
- lactobacillus casei (probiotics) – I would go with Custom Probiotics and use their dosages (240 BCFU)
- enterococcus faecium (probiotic) – I personally used bioflorin, but that is more challenging to obtain.
- lactobacillus reuteri (probiotics) – I would also go to Custom Probiotics and use their dosage (80 BCFU/day)
- lactobacillus rhamnosus gg (probiotics) – ditto with Custom Probiotics (320 BCFU)
I have no financial interest in Custom Probiotics — they are just by far the cheapest per BCFU and advocate therapeutic dosages.
I would encourage you to look at the avoids and remove the high value items. See video below.
I would not be surprised if you have a Jarisch–Herxheimer reaction from some of the above. I usually advocate the Cecile Jadin approach which is to take one or two items at a time for up to 2 weeks and then rotate to other items. Start with a low dosage and slowly work up the dosage. This will usually reduce the risk of a strong herxheimer reaction. This approach reduces the risk of antibiotic (or equivalent) resistance happening. There will always be a bacteria mutations that will tolerate specific herbs, probiotics and antibiotics. The odds of the bacteria tolerating multiple substances is very low.
I would suggest doing the rotating suggestions for 8 weeks and then retest. Always use the same lab so comparisons are valid.
Postscript – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I cannot tell people what they should take or not take. I can inform people items that have better odds of improving their microbiome as a results on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting.
The answers above describe my logic and thinking and is not intended to give advice to this person or any one. Always review with your knowledgeable medical professional.
Recent Comments