This document presents the results of statistical analysis on symptoms from viable, self-annotated Biomesight microbiome samples. The methodology for data acquisition is outlined in New Standards for Microbiome Analysis?.
Tables have been refined to display only genus- and species-level taxa, the 20 most prominent entries per group, and associations achieving statistical significance (P < 0.01).
The following sections provide the processed data, accompanied by guidance on interpretation and application. Counts of significant bacterial taxa are included, reflecting the application of non-standard but rigorously validated statistical approaches to extensive sample and reference populations, where statistical power derives from dataset scale.
| Significance | Genus |
| p < 0.01 | 223 |
| p < 0.001 | 199 |
| p < 0.0001 | 181 |
| p < 0.00001 | 164 |
Averages and Medians
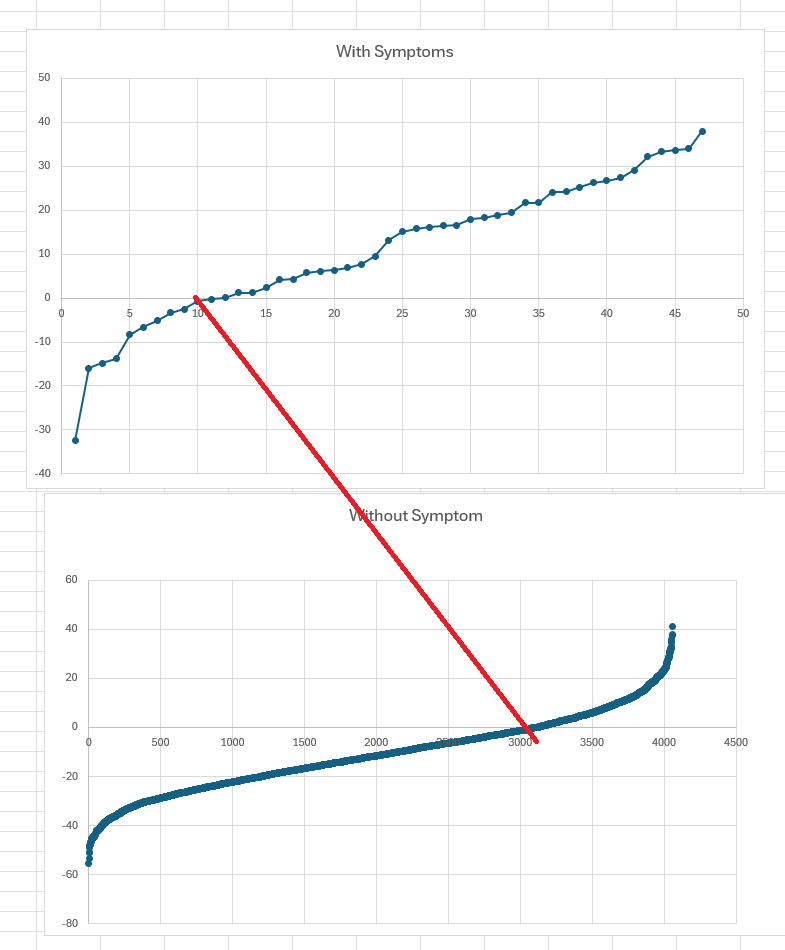
I prefer medians over averages. Medians are the values where half of the people have less and half has more. If the data was a bell-curve, then the values will almost be the same… with bacteria that happens rarely. Look at the bacterua below, we see that for some the average is above and the median below. Should one increase or decrease this bacteria?
If symptom median is higher than reference median, it means there is more of this bacteria. If lower, then less. This ignores how often the bacteria is seen (we average only over reports). IMHO using average value instead of median will often result in a worse situation for the patient
| tax_name | Rank | Symptom Average | Reference Average | Symptom Median | Reference Median |
| Faecalibacterium prausnitzii | species | 13.575 | 12.086 | 11.275 | 12.554 |
| Phocaeicola dorei | species | 3.484 | 2.854 | 0.395 | 0.746 |
| Roseburia | genus | 2.432 | 2.876 | 1.812 | 1.484 |
| Lachnospira | genus | 2.424 | 2.755 | 1.901 | 1.631 |
| Roseburia faecis | species | 0.855 | 1.239 | 0.594 | 0.378 |
| Sutterella wadsworthensis | species | 0.75 | 0.65 | 0.049 | 0.239 |
| Coprococcus | genus | 1.083 | 1.463 | 0.741 | 0.609 |
| Pedobacter | genus | 1.299 | 0.971 | 0.551 | 0.651 |
| Blautia wexlerae | species | 0.474 | 0.589 | 0.324 | 0.27 |
| Anaeroplasma | genus | 1.197 | 0.432 | 0.003 | 0.05 |
| Dorea | genus | 0.454 | 0.486 | 0.299 | 0.256 |
| Parabacteroides goldsteinii | species | 0.585 | 0.569 | 0.133 | 0.171 |
| Thermicanus | genus | 0.206 | 0.188 | 0.101 | 0.127 |
| Odoribacter | genus | 0.28 | 0.189 | 0.122 | 0.146 |
| Bacteroides stercorirosoris | species | 0.166 | 0.196 | 0.139 | 0.116 |
| Collinsella aerofaciens | species | 0.154 | 0.172 | 0.05 | 0.071 |
| Acetivibrio alkalicellulosi | species | 0.237 | 0.261 | 0.1 | 0.08 |
| Acetivibrio | genus | 0.246 | 0.27 | 0.105 | 0.085 |
| Dorea formicigenerans | species | 0.111 | 0.136 | 0.086 | 0.067 |
| Anaerofilum | genus | 0.23 | 0.273 | 0.109 | 0.092 |
Bacteria Incidence – How often is it reported
The common sense belief is that if a bacteria is reported more often, then the amount should be higher. This is often not true. The microbiome is a complex thing.
| tax_name | Rank | Incidence Odds Ratio | Chi2 | Symptoms % | Reference % |
| Lactococcus | genus | 1.27 | 7.2 | 60.5 | 47.6 |
| Sporotomaculum | genus | 0.72 | 8.8 | 31.6 | 43.8 |
| Sporotomaculum syntrophicum | species | 0.73 | 8.5 | 31.3 | 43.2 |
| Enterobacter hormaechei | species | 0.7 | 6.9 | 18 | 25.8 |
| Actinopolyspora | genus | 0.58 | 9.9 | 10.6 | 18.2 |
| Rothia mucilaginosa | species | 0.62 | 8.3 | 11.7 | 18.8 |
| Citrobacter | genus | 0.65 | 7.1 | 12.5 | 19.2 |
| Peptoniphilus lacrimalis | species | 1.47 | 8.2 | 20.7 | 14.1 |
| Chromatium | genus | 0.63 | 7.3 | 11.2 | 17.6 |
| Chromatium weissei | species | 0.64 | 7.3 | 11.2 | 17.6 |
| Anaerococcus hydrogenalis | species | 1.48 | 6.9 | 16.1 | 10.9 |
More or Less often based on Symptom Median All Incidence
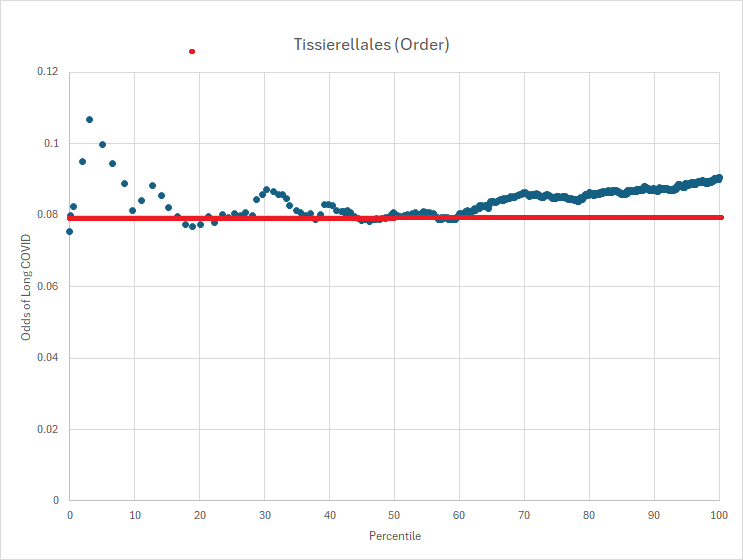
This is a little more complex to understand. If we compute the mid point for people with the symptom, then if the bacteria was not involved then half of the reference should be above this value and half below this value. If not, it means that the symptom tends to over or under growth.
| tax_name | Rank | Symptom Median | Odds Ratio | Chi2 | Below | Above |
| Isoalcanivorax | genus | 0.002 | 0.27 | 76.7 | 370 | 99 |
| Isoalcanivorax indicus | species | 0.002 | 0.27 | 76.7 | 370 | 99 |
| Alcanivorax | genus | 0.002 | 0.27 | 76.6 | 380 | 103 |
| Nostoc flagelliforme | species | 0.002 | 0.25 | 74.8 | 311 | 78 |
| Niabella aurantiaca | species | 0.002 | 0.32 | 71.5 | 534 | 172 |
| Pelagicoccus croceus | species | 0.002 | 0.3 | 66 | 378 | 115 |
| Psychrobacter glacialis | species | 0.002 | 0.36 | 65.8 | 654 | 233 |
| Deferribacter autotrophicus | species | 0.002 | 0.31 | 65.2 | 378 | 116 |
| Deferribacter | genus | 0.002 | 0.31 | 64.6 | 381 | 118 |
| Salidesulfovibrio | genus | 0.002 | 0.32 | 63.2 | 386 | 122 |
| Salidesulfovibrio brasiliensis | species | 0.002 | 0.32 | 63.2 | 386 | 122 |
| Actinopolyspora | genus | 0.002 | 0.36 | 60.6 | 537 | 192 |
| Niabella | genus | 0.002 | 0.36 | 60.1 | 571 | 208 |
| Rickettsia marmionii Stenos et al. 2005 | species | 0.002 | 0.33 | 60 | 394 | 130 |
| Lentibacillus | genus | 0.002 | 0.36 | 57.6 | 500 | 181 |
| Psychroflexus | genus | 0.002 | 0.32 | 57.5 | 343 | 111 |
| Psychroflexus gondwanensis | species | 0.002 | 0.32 | 57.5 | 343 | 111 |
| Lentibacillus salinarum | species | 0.002 | 0.36 | 57.2 | 485 | 175 |
| Viridibacillus neidei | species | 0.002 | 0.36 | 56.6 | 463 | 166 |
| Bacillus ferrariarum | species | 0.002 | 0.34 | 56.1 | 361 | 121 |
More or Less often based on Reference Median All Incidence
This is like the above, but with a different line in the sand. Instead of the median of those with the condition, we use the median of the reference set.
| tax_name | Rank | Reference Median | Odds Ratio | Chi2 | Below | Above |
| Actinopolyspora | genus | 0.003 | 0.16 | 326.3 | 628 | 101 |
| Nostoc | genus | 0.003 | 0.33 | 281.5 | 1134 | 376 |
| Flammeovirga | genus | 0.003 | 0.35 | 186.1 | 742 | 261 |
| Asticcacaulis | genus | 0.003 | 0.42 | 185.9 | 1064 | 446 |
| Flammeovirga pacifica | species | 0.003 | 0.35 | 185.6 | 741 | 261 |
| Planococcus | genus | 0.003 | 0.32 | 182.4 | 613 | 194 |
| Planococcus columbae | species | 0.003 | 0.31 | 176.2 | 575 | 179 |
| Streptococcus oralis | species | 0.003 | 0.48 | 167.3 | 1358 | 652 |
| Psychrobacter glacialis | species | 0.002 | 0.36 | 164.8 | 654 | 233 |
| Niabella aurantiaca | species | 0.002 | 0.32 | 158.7 | 534 | 172 |
| Clostridium tepidiprofundi | species | 0.003 | 0.38 | 152.9 | 659 | 248 |
| Niabella | genus | 0.002 | 0.36 | 142.4 | 571 | 208 |
| Alcanivorax | genus | 0.002 | 0.27 | 142.3 | 380 | 103 |
| Isoalcanivorax | genus | 0.002 | 0.27 | 140.7 | 370 | 99 |
| Isoalcanivorax indicus | species | 0.002 | 0.27 | 140.7 | 370 | 99 |
| Atopobium fossor | species | 0.003 | 0.37 | 138.2 | 555 | 203 |
| Lentibacillus | genus | 0.002 | 0.36 | 128.3 | 500 | 181 |
| Nostoc flagelliforme | species | 0.002 | 0.25 | 127.5 | 311 | 78 |
| Desulfitobacterium | genus | 0.005 | 0.38 | 126.8 | 525 | 197 |
| Lentibacillus salinarum | species | 0.002 | 0.36 | 125.5 | 485 | 175 |
More or Less often based on Symptom Median High Incidence
Above we see that many of the top bacteria identified are sparse, that is not reported often. We then restrict them to those that occur above 50% or the time.
| tax_name | Rank | Symptom Median Freq | Odds Ratio | Chi2 | Below | Above |
| Clostridium taeniosporum | species | 0.003 | 0.62 | 17.5 | 1284 | 800 |
| Dethiosulfovibrio | genus | 0.004 | 0.67 | 12.7 | 1433 | 961 |
| Tetragenococcus doogicus | species | 0.003 | 0.68 | 11.8 | 1289 | 875 |
| Mycoplasmopsis | genus | 0.005 | 0.7 | 10 | 1707 | 1203 |
| Hydrocarboniphaga daqingensis | species | 0.004 | 0.72 | 9 | 1533 | 1097 |
| Tetragenococcus | genus | 0.003 | 0.74 | 6.8 | 1270 | 946 |
| Pediococcus | genus | 0.004 | 0.75 | 6.6 | 1239 | 926 |
More or Less often based on Reference Median High Incidence
Above we see that many of the top bacteria identified are sparse, that is not reported often. We then restrict them to those that occur above 50% or the time.
| tax_name | Rank | Reference Median Freq | Odds Ratio | Chi2 | Below | Above |
| Actinopolyspora | genus | 0.003 | 0.16 | 326.3 | 628 | 101 |
| Nostoc | genus | 0.003 | 0.33 | 281.5 | 1134 | 376 |
| Flammeovirga | genus | 0.003 | 0.35 | 186.1 | 742 | 261 |
| Asticcacaulis | genus | 0.003 | 0.42 | 185.9 | 1064 | 446 |
| Flammeovirga pacifica | species | 0.003 | 0.35 | 185.6 | 741 | 261 |
| Planococcus | genus | 0.003 | 0.32 | 182.4 | 613 | 194 |
| Planococcus columbae | species | 0.003 | 0.31 | 176.2 | 575 | 179 |
| Streptococcus oralis | species | 0.003 | 0.48 | 167.3 | 1358 | 652 |
| Psychrobacter glacialis | species | 0.002 | 0.36 | 164.8 | 654 | 233 |
| Niabella aurantiaca | species | 0.002 | 0.32 | 158.7 | 534 | 172 |
| Clostridium tepidiprofundi | species | 0.003 | 0.38 | 152.9 | 659 | 248 |
| Niabella | genus | 0.002 | 0.36 | 142.4 | 571 | 208 |
| Alcanivorax | genus | 0.002 | 0.27 | 142.3 | 380 | 103 |
| Isoalcanivorax | genus | 0.002 | 0.27 | 140.7 | 370 | 99 |
| Isoalcanivorax indicus | species | 0.002 | 0.27 | 140.7 | 370 | 99 |
| Atopobium fossor | species | 0.003 | 0.37 | 138.2 | 555 | 203 |
| Lentibacillus | genus | 0.002 | 0.36 | 128.3 | 500 | 181 |
| Nostoc flagelliforme | species | 0.002 | 0.25 | 127.5 | 311 | 78 |
| Desulfitobacterium | genus | 0.005 | 0.38 | 126.8 | 525 | 197 |
| Lentibacillus salinarum | species | 0.002 | 0.36 | 125.5 | 485 | 175 |
Summary
A large number of bacterial taxa exhibit shifts with P < 0.01 in association with this condition. The subsequent challenge is determining how to modulate these taxa, since the volume of candidates exceeds what most individuals can practically consider. Moreover, for many of the taxa identified, there is no published evidence in the U.S. National Library of Medicine describing how to alter their abundance.
A deep optimization model, such as the one implemented on the Microbiome Taxa R2 site, can be used to inform probiotic selection. This model provides coverage for each identified taxon and infers which probiotics are most likely to shift their levels. Its output may then be integrated with more conventional recommendations derived from literature indexed in the U.S. National Library of Medicine where such evidence exists, with the two recommendation sets reconciled by giving priority to probiotic-based suggestions.
Development of a dedicated database based on Biomesight samples is in progress. The current model uses data contributed by PrecisionBiome, and datasets generated with differing laboratory processing pipelines cannot be safely combined, as discussed in The taxonomy nightmare before Christmas…. Once the Biomesight-specific database is complete, an option for generating (offline-only) personalized suggestions will be added to the Microbiome Prescription website.
Probiotics Suggestions
The following are based on a simplified algorithm using R2 data for Biomesight. These are tentative numbers subject to future refinements. Bacteria listed are only for probiotics detected with Biomesight tests. Probiotics include some that are available only in some countries and some that are pending approval for retail sale.
- Good Count: Number of bacteria expected to shift in desired direction
- Bad Count: Number of bacteria expected to shift in wrong direction
- Impact: Estimator of impact based on Chi-2, Slope and R2 vectors
| Blautia hansenii | 194.64 | 19 | 0 |
| Blautia wexlerae | 147.38 | 8 | 0 |
| Faecalibacterium prausnitzii | 74.57 | 10 | 3 |
| Enterococcus faecalis | 19.48 | 34 | 44 |
| Lactobacillus johnsonii | 9.37 | 29 | 62 |
| Streptococcus thermophilus | 4.1 | 8 | 0 |
| Escherichia coli | 3.35 | 8 | 2 |
| Segatella copri | 2.83 | 2 | 4 |
| Enterococcus faecium | 2.16 | 10 | 45 |
| Bifidobacterium breve | 1.91 | 2 | 3 |
| Heyndrickxia coagulans | 1.89 | 7 | 39 |
| Bifidobacterium longum | 1.7 | 2 | 2 |
| Bifidobacterium adolescentis | 1.46 | 2 | 0 |
| Enterococcus durans | 1.4 | 27 | 30 |
| Bifidobacterium bifidum | 0.48 | 3 | 2 |
| Bifidobacterium catenulatum | 0.27 | 3 | 4 |
| Lacticaseibacillus paracasei | 0.2 | 5 | 14 |
| Bifidobacterium animalis | 0.16 | 1 | 1 |
| Leuconostoc mesenteroides | 0.09 | 11 | 26 |
| Limosilactobacillus fermentum | 0.04 | 9 | 29 |
| Veillonella atypica | -0.03 | 2 | 4 |
| Ligilactobacillus salivarius | -0.11 | 5 | 21 |
| Lacticaseibacillus casei | -0.13 | 1 | 12 |
| Lacticaseibacillus rhamnosus | -0.23 | 1 | 14 |
| Lactiplantibacillus plantarum | -0.26 | 0 | 12 |
| Limosilactobacillus reuteri | -0.47 | 24 | 31 |
| Akkermansia muciniphila | -0.51 | 3 | 15 |
| Lactobacillus acidophilus | -0.7 | 5 | 42 |
| Lactobacillus crispatus | -0.95 | 1 | 43 |
| Odoribacter laneus | -0.96 | 0 | 3 |
| Bacillus subtilis | -0.99 | 29 | 55 |
| Limosilactobacillus vaginalis | -1.33 | 21 | 70 |
| Parabacteroides distasonis | -1.35 | 0 | 1 |
| Bacteroides uniformis | -2.4 | 3 | 3 |
| Lactobacillus jensenii | -2.56 | 6 | 82 |
| Bifidobacterium pseudocatenulatum | -3.11 | 5 | 43 |
| Lactobacillus helveticus | -5.05 | 35 | 100 |
| Bacteroides thetaiotaomicron | -5.17 | 2 | 3 |
| Clostridium butyricum | -5.21 | 0 | 35 |
| Pediococcus acidilactici | -9.29 | 40 | 51 |
| Parabacteroides goldsteinii | -9.3 | 0 | 12 |
Recent Comments