Reminder:
I am a computer scientist and a statistician. I am not licensed to practice medicine, and where I live has strict laws about ‘appearing to practice medicine’. What I can do for readers is to write a public blog (anonymous) from your data and back story as an education post on using the software and the statistics it produces. I cannot consult. The content should be reviewed by a medical professional before implementing.
Back Story
35yr old, female with ME of around 15 years, Coeliac and Crohn’s diagnosed in 2014 plus simple temporal lobe seizures and endometriosis.
I have tested extremely extensively and most labs are generally normal with the exception of:
- Prolactin- always slightly above high end of range
- Lyme ELISA IgM positive but Blot negative (possibly cross-reactive with RF)
- Rheumatoid factor – one point over upper range
- LDH – consistently slightly above range
- Aldolase – tested once, slightly above range
- ALT – occasionally slightly above range
- EBV – positive for past infection but never any evidence of reactivation
- SIBO breath test positive for hydrogen only
I am really struggling with acne… I have been offered Lymecycline for the acne but don’t know if it’s worth the risk. I am currently on a 7-day course of Co-amoxiclav (amoxicillin + clavulanic acid) for an infected cyst (my Biome sample was taken before this).
I was able to control my crohn’s with an elemental diet, followed by strict paleo, then gradually reverting to a more relaxed diet. I did a course of oregano oil which was very harsh on the gut but it got rid of my constant bloating for the first time in my life (this came back and remains since reintroducing carbs). I’m 99.9% sure I’m on the autism spectrum. Interestingly, some of my autistic traits and my ME symptoms abate somewhat for a short period at the beginning of a cold virus (the first couple of days while fever is present). I had a similar temporary reaction to Sulforaphane.
My ME started while I was working full time, following glandular fever in 2006. The onset was characterised by ‘tired but wired’ and rolling PEM, finding it almost impossible to fall asleep until it was nearly time to get up and a complete inability to get into deep sleep. I reduced my working hours gradually but eventually gave up work fully in 2008. Even when ‘healthy’ I never had normal stamina, muscle mass and was really ready for bed by the end of the work day.
Possibly coinciding with my gastrointestinal diagnoses and subsequent avoidance of gluten, my symptoms calmed a bit from the ‘acute’ years, and I began to sleep a little better and get brief symptom-free interludes while at rest. Now, prolonged activity above baseline will lead to a return of the PEM and ‘tired but wired’ symptoms (inability to switch off nonsensical chattering thoughts at night leading to insomnia, feeling hot with chills, feverish, sweats, tossing and turning all night. These symptoms stop on rising but leave me extremely brain fogged from the sleep deprivation, and then repeat the next night. I also experience myalgia, headaches, orthostatic intolerance and strong need to lay horizontal throughout the day. I wake with heavy puffy face and eyelids most days. I go through periods of extreme dry mouth, worse on waking despite always hydrating well.
Even in my symptom-free-at-rest periods, I still struggle to get to sleep some nights, although I keep a strict routine 10pm-10am. I find it very difficult to get into the deeper stages of sleep almost all of the time. Even with all reasonable interventions and ear plugs I am easily startled awake by household sounds and there is usually activity from others from 4-5am onwards.
Microbiome Analysis
I am going to do three levels of Analysis. I will start with generic, then move on to diagnosis using US National Library of Medicine studies and ending with the latest refactor, using bacteria associated with symptoms discovered from uploads to this site.
The purpose of these analysis to get suggestions for the most probable bacteria causing issues.
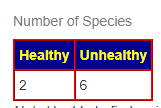
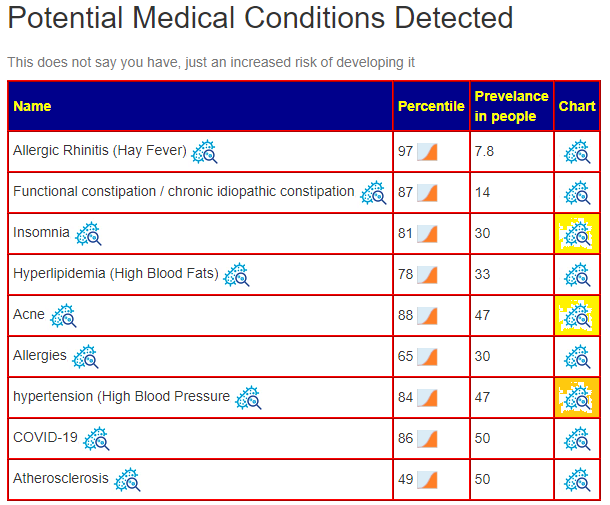
Overall Health
I will not go step by step (see this post with video for how to do this) but do the following suggestion generation and then look at the consensus
- Jason H – 10 bacteria picked
- Standard Lab Ranges (+/- 2 Std Dev) – 7 bacteria picked
- Box Plot Whisker – 61 bacteria picked
- Kaltoft-Moltrup Normal Ranges – 98 bacteria
- Top Bottom at 5%: 41 bacteria
Then I went to Advance Suggestion with Percentile: 15% and the following PubMed conditions (Remember that Display Level must be Intermediate or higher to see this option):
- Acne – 3 bacteria
- Crohn’s Disease – 24 bacteria
- Celiac Disease – 14 bacteria
- Chronic Fatigue Syndrome – 13 bacteria
Then I went to Symptom Associated to Bacteria (Citizen Science) and found the following applicable items:
- Official Diagnosis: Chronic Fatigue Syndrome (CFS/ME) – 10 bacteria
- Autism – 1 bacteria
- Insomnia – 9 bacteria
- Brain Fog –
For Official Diagnosis: Chronic Fatigue Syndrome (CFS/ME), most of the matched were at the Genus Level
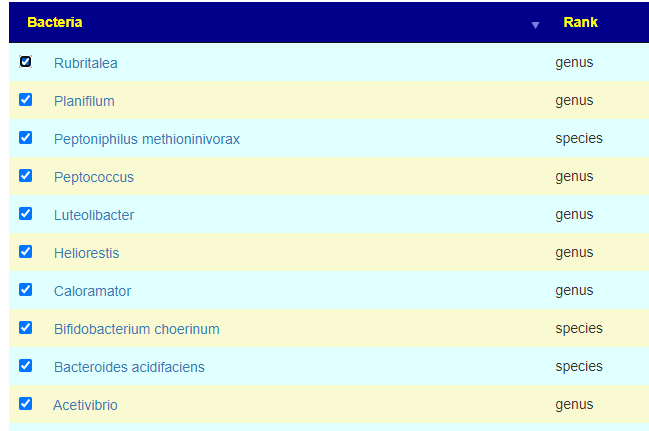
The result is 40 bacteria added to our hand picked list.
Consensus Highlights
We have a lot of different suggestions over our 10 analysis, often more than 1000!
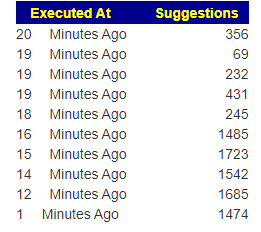
Suggestions to discuss with your medical professional
- lauric acid(fatty acid in coconut oil,in palm kernel oil,) aka Monolaurin – 10 recommends
- whole-grain barley, barley,oat
- apple (as a personal note, my wife has Crohn’s and Pink Lady Apples work best for her)
- Cacao – there are studies with ME/CFS that is effective, 85% or higher is suggested
- bifidobacterium longum (probiotics)
- chondrus crispus (red sea weed)
- lactobacillus paracasei (probiotics)
On the avoid list:
- folic acid,(supplement Vitamin B9) – often I see that B-Vitamins are split between take and avoid, this suggests that B-Complex capsules may not be the best choice.
- high red meat
- low-fat diets
- quercetin,resveratrol
- saccharin
- cannabinoids
Also listed was gluten-free diet. I suspect the type of gluten may be significant.
KEGG Probiotics:
The usual one for ME/CFS are at the top (and were also listed in Safer or Safest Takes) :
- miyarisan (jp) / miyarisan aka clostridium butyricum (probiotics)
- lactobacillus plantarum (probiotics) – available in many products
For supplements:
- beta-alanine – Percentile: 9.7
- D-Ribose – Percentile: 4
- Glycine – Percentile: 13.6
- L-Cysteine – Percentile: 13.6
- L-Threonine – Percentile: 6.5
- Magnesium – Percentile: 0.1
Both D-Ribose and Magnesium are well studied supplements in a ME/CFS context (confirming predictions to clinical practice the items are linked to CFSRemission Blog).
Bottom Line
At this point I will stop for several reasons:
- Purpose was to show the method
- Person has brain fog often, so more notes may be counter productive
- ME/CFS usually have restricted funds, so keeping the number of items low reduces frustrations over not being able to acquire.
A video will be added in the next few days
Questions And Answers
Q: I forgot to mention it, but I do have allergic rhinitis and high cholesterol (as listed under the detected conditions) so this is very accurate.
A: Although I see this often, it keeps surprising me about the accuracy of predictions!
Q: Interesting that it doesn’t pick up on any CFS-related bacteria at a species level, I wonder if this fluctuates and could possibly be because I was relatively low-symptom at the time of the sample, i.e. not in a PEM flare?
A: You are very likely correct, it does fluctuates. Also, keep in mind that there are many subsets of ME/CFS, so this can be a little hit-and-miss.
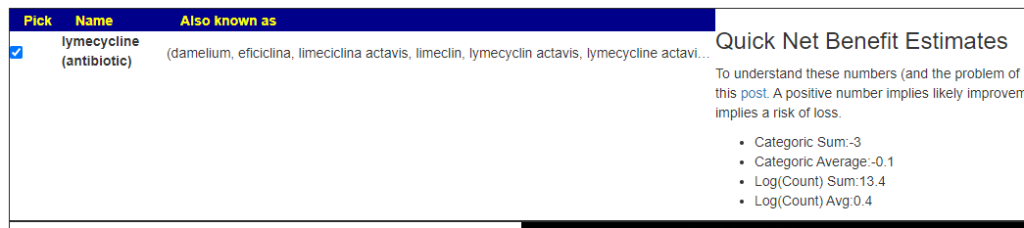
Should I take Lymecycline?
A: This is a little complex, we have mixed results.
But when I tried a different antibiotic often prescribed for acne, it is all positive
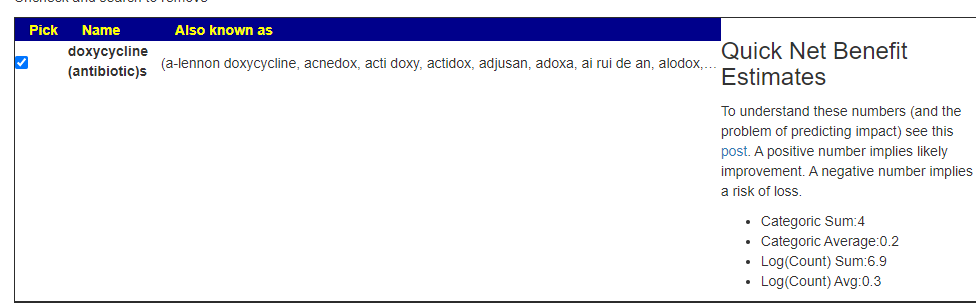
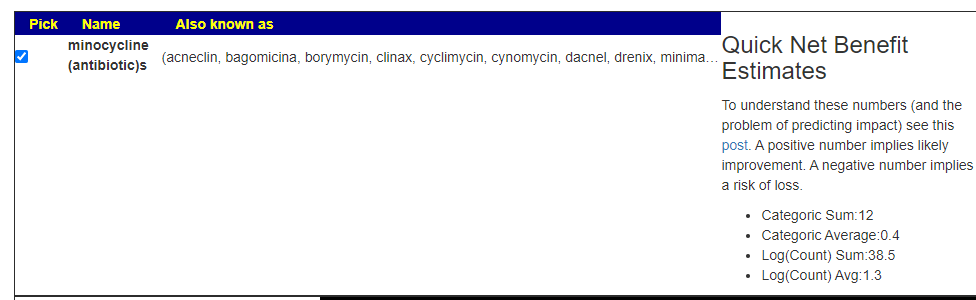
I would suggest making a counter proposal to your medical professional of minocycline instead.
Q: I’d be interested in your opinion on IgY hyperimmune egg powder supplements for targeting gut pathogens
A: There are many retail products like this. What I found are some vet studies[36 listed here]. I found a list of clinical studies here. My general impression is that it is favorable. There is one word of caution, it appears similar to transfer factor — i.e. the IgY may be targeted to specific bacteria/infections only. Hence, my advice would be to buy just one unit of it, if no response, change to a different brand when you finish it. Remember my motto: Rotate, rotate, rotate….
- Protection Efficacy of Multivalent Egg Yolk Immunoglobulin against Eimeria tenella Infection in Chickens [2013] ” Chickens fed IgY resulted in reduced mortality, increased body weight gain (BWG), reduced oocyst shedding, reduced caecal lesion score and increased anti-coccidial index.”
- “Oral immunotherapy using egg yolk polyclonal IgYs against Eimeria sp. represents an effective and natural resource against severe E. tenella infection favoring the gradual withdrawal of the anticoccidial drugs and antibiotics.” [2021]
- Impact of Dietary Egg Yolk IgY Powder on Behavior, Meat Quality, Physiology, and Intestinal Escherichia coli Colonization of Broiler Chicks [2022] “Our study concluded that dietary supplementation of 3,000 and/or 4,000 μg/ml IgY improved the growth rates, behavioral activities, intestinal health indices, and meat quality of broiler chicks.”
- Passive Immunization of Chickens with Anti-Enterobactin Egg Yolk Powder for Campylobacter Control [2021] “Collectively, oral administration of broiler chickens with the anti-Ent egg yolk powder failed to confer protection against intestinal colonization of C. jejuni,”
Recent Comments