A person asked:
Should I be taking flushing niacin with Crohn’s Disease. I feel better after taking it, but I read that it encourages the release of prostaglandins, particularly prostaglandin D2 (PGD2) and prostaglandin E2 (PGE2), rather than histamine.
My first step is to go to Perplexity.AI and ask questions there and then check the sources cited. I then use this to jump into PubMed to get better information. As with all AI, you need to learn to ask clear specific questions.
Questions:
- What are the consequences of using flushing niacin with Crohn’s Disease?
- The full answer.
- After reading the studies, I go to the PubMed Summary and look at Similar articles and Cited By. Often this will lead to other studies.
- Next I return to Perplexity and look at the follow up questions that it proposes.
- The process is repeated — every item to be consider should check the source study.
The next step is take all of the key words above and do a full text search on PMC
- Crohn’s Disease
- Niacin
- prostaglandin D2 (PGD2)
- D prostanoid receptor 1 (DP1)
- inflammation.
For words that you are not familiar with, just ask Perplexity.
- “What is the role of D prostanoid receptor 1 (DP1).”
- Full Answer.
- Follow up Question (asking the question from a different direction) “What is its impact on Crohn’s disease”
Searching PMC
Just go to the site: https://www.ncbi.nlm.nih.gov/pmc/
- Entering: Niacin and inflammation => 12,000 hits
- Changing to: Niacin inflammation Crohn’s => 1127 hits
I changed to default order (most relevant first) and spotted some interesting titles:
- Niacin in the Central Nervous System: An Update of Biological Aspects and Clinical Applications [2019]
- Niacin ameliorates ulcerative colitis via prostaglandin D2‐mediated D prostanoid receptor 1 activation [2017]
- Effects of ileocolonic delivered vitamin B2, B3[NIACIN] and C (ColoVit) or the Groningen anti-inflammatory diet on disease course and microbiome of patients with Crohn’s disease (VITA-GrAID study): a protocol for a randomised and partially blinded trial [2023] – Pending study
- Niacin Ameliorates Neuro-Inflammation in Parkinson’s Disease via GPR109A
- Niacin Suppresses Progression of Atherosclerosis by Inhibiting Vascular Inflammation and Apoptosis of Vascular Smooth Muscle Cells [2015]
- Nutrient Intake of Crohn’s Patients: Is There Consistency between Crohn’s Disease Activity Index, Subjective Global Assessment and Body Mass Index? [2021]
- Daily energy, carbohydrate, monosaccharide, starch, sucrose, fructose, poly-unsaturated fatty acids, omega-3 fatty acids, fiber, vitamin E and C, thiamine, niacin, pyridoxine, Mg, P, Fe, Cu, Zn intakes were significantly lower in Crohn’s Group than in Control Group.
- Nutritional deficiencies in patients with Crohn’s disease in remission [2006]
- “More than 50% of patients had low plasma concentrations of vitamin C (84%), copper (84%), niacin (77%), and zinc (65%).”
- Association between dietary niacin intake and cognitive function in the elderly: Evidence from NHANES 2011–2014 [2023]
- “High niacin intake favors a decrease in the incidence of low cognition”
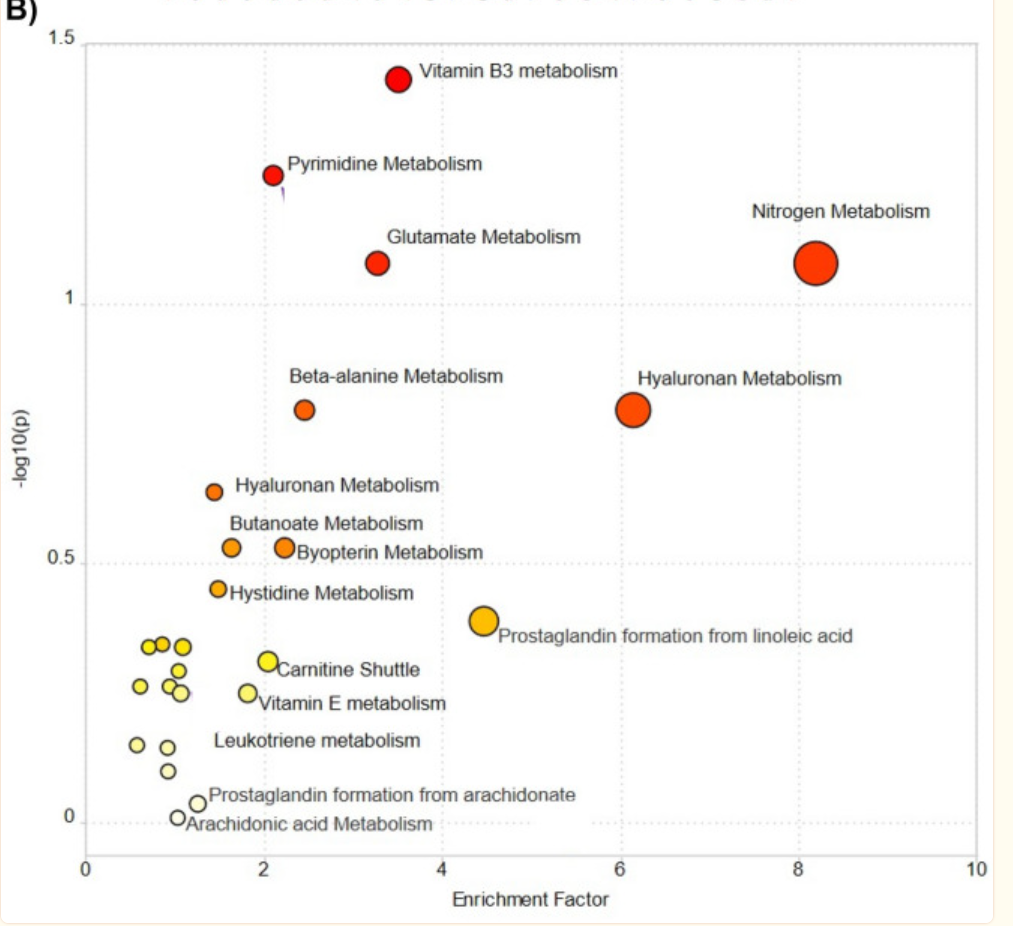
This study was of particular interest: Identifying metabolic shifts in Crohn’s disease using ‘omics-driven contextualized computational metabolic network models [2023]
“Interestingly, high-dose vitamin B3 treatment has been shown to ameliorate ulcerative colitis through increased prostaglandin D2 synthesis in mice54. Thus, niacin supplementation can be a potential therapeutic target to be investigated in CD as well. In addition, untargeted metabolomics showed the dysregulation of pathways related to pyrimidine, glutamate, and nitrogen metabolism. “
Second Question: Niacin and MCAS
Mast cell activation syndrome (MCAS) is another issue that the person is dealing with.
Asking more we get a yes/no with lacking studies.
Digging more we see other things that are EITHER/OR. Thus PGD2 in isolation is not connected to activation; rather activation is conditional on multiple factors (one of them is PGD2). “MCAS is associated with a variety of mediators beyond PGD2, including histamine, tryptase, leukotrienes, cytokines, heparin, PAF, neuropeptides, and other eicosanoids.”
- “Tests for serum PGD2 have similar drawbacks, as processing of peripheral blood samples can trigger non-MC cellular elements to release PGD2; ingestion of niacin is also associated with elevations in serum PGD2 ” [1994] so this may rendering test results invalid.
- Using the Right Criteria for MCAS [2023]
- “Mediators other than tryptase, including urinary metabolites of histamine, prostaglandin D2 (PGD2), and leukotrienes, are also available but less specific for MCs and MCAS [28, 29, 30••]. Additionally, the sensitivity and specificity of these markers have not been determined, nor have the reliable indicators of systemic MC activation, such as significant increase and cut-off levels. ‘
- “PGD2, while primarily released by MC, is also produced by other immune and nonimmune cell types [42–45]..elevations in PGD2 might be due to a pathologic process independent of MC activation.”
- Concentrating on Niacin and Histamine, Perplexity gives plus and minus, concluding “In summary, niacin can both positively and negatively impact histamine levels and symptoms.” So, our bottom line is that it depends on the individual.
The responses mention S-adenosylmethionine (SAMe) being consumed with Niacin.
Which implies SAMe should be taken with the Niacin.
Bottom Line
The final decision is always the person in consultation with their medical professional. Using Niacin as a treatment for Crohn’s Disease is heading for clinical trial and suggested by a 2023 metabolic shifts study on Crohn’s. Given the low risk (assuming medical monitoring for niacin risk), I personally would favor doing it (making sure their usual MD is aware of the dosage and a possible need to monitor).
The purpose of this post is to show a method of gathering information to make better health choices. I have fallen in love with Perplexity.AI because it cites studies on PubMed often and it’s suggestions are easy to verify and evaluate. It also prompts for follow up questions.
We discovered a multitude of deficiencies that may need to be supplemented (factoring in poor absorption due to Crohn’s) including:
- SAMe (because of the niacin use)
- fructose,
- poly-unsaturated fatty acids,
- omega-3 fatty acids,
- vitamin E and C,
- thiamine,
- niacin,
- pyridoxine,
- Mg,
- P,
- Iron,
- Copper,
- Zinc
This lead to the logic questions: What are all the deficiencies seen in Crohn’s disease that can be supplemented? Full Answer.
P.S. The time it took to do the above was about 90 minutes,
Recent Comments