I’ve been suffering from myalgic encephalomyelitis for over a year now (long covid or not, I don’t know), in an almost severe state for the last 6 months.
I recently had a Biomesight test and a long covid friend told me that you might be able to help me interpret my results.
Overview
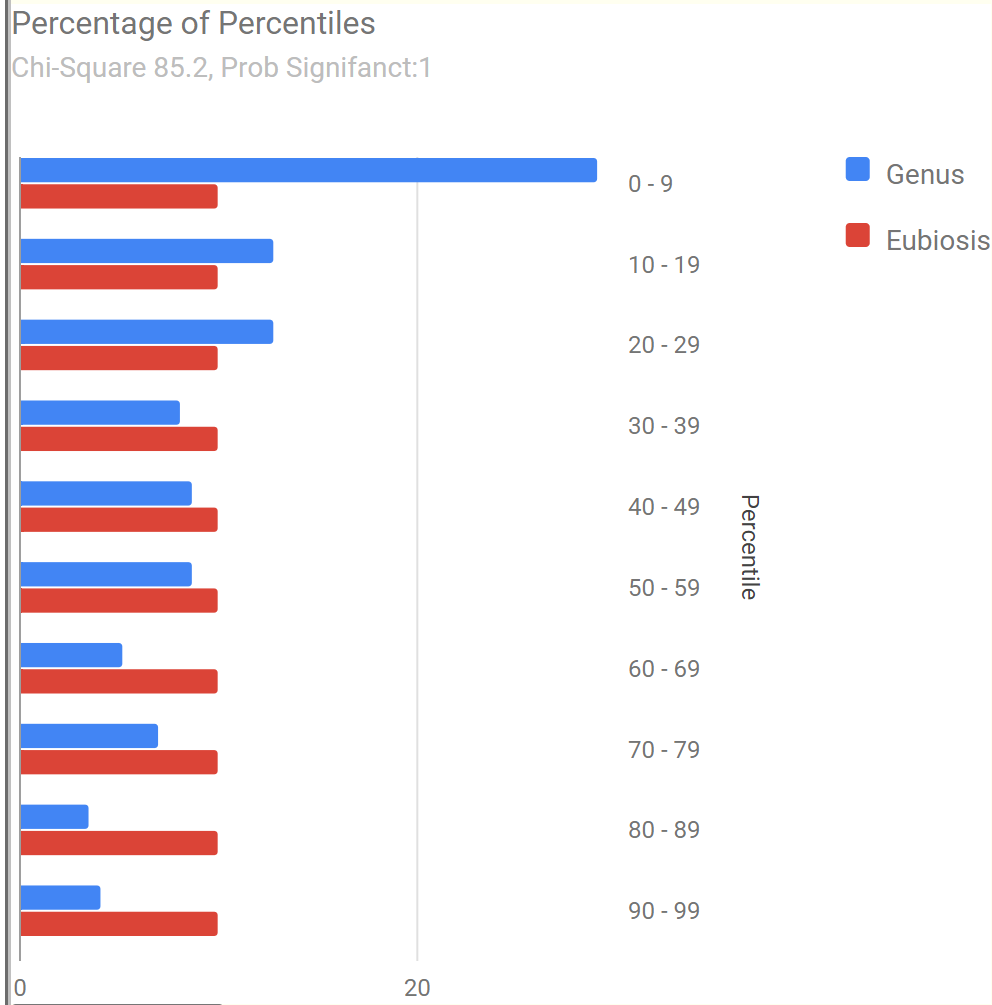
Our usual first look visuals shows the dysbiosis and the typical pattern for ME/CFS and long COVID – an over abundance of bacteria at a low levels.
The forecast symptoms matches ME/CFS and Long COVID patterns
- 83.3 % match for Neurological-Sleep: Inability for deep (delta) sleep on 42 taxa
- 76.3 % match for Immune Manifestations: Hair loss on 38 taxa
- 76.3 % match for Immune Manifestations: Mucus in the stool on 93 taxa
- 75.2 % match for Neurocognitive: Problems remembering things on 141 taxa
- 74.7 % match for Neurocognitive: Absent-mindedness or forgetfulness on 162 taxa
- 74.6 % match for Neurological: Short-term memory issues on 71 taxa
- 74.5 % match for Neuroendocrine Manifestations: cold extremities on 55 taxa
- 74.3 % match for Neurocognitive: Can only focus on one thing at a time on 101 taxa
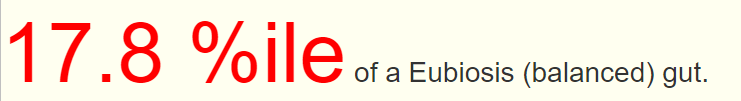
Drilling down into Health Predictors we see a rather high number, 13 items flagged. Looking at Dr. Jason Hawrelak Recommendations , we are at the 9%ile, not good.
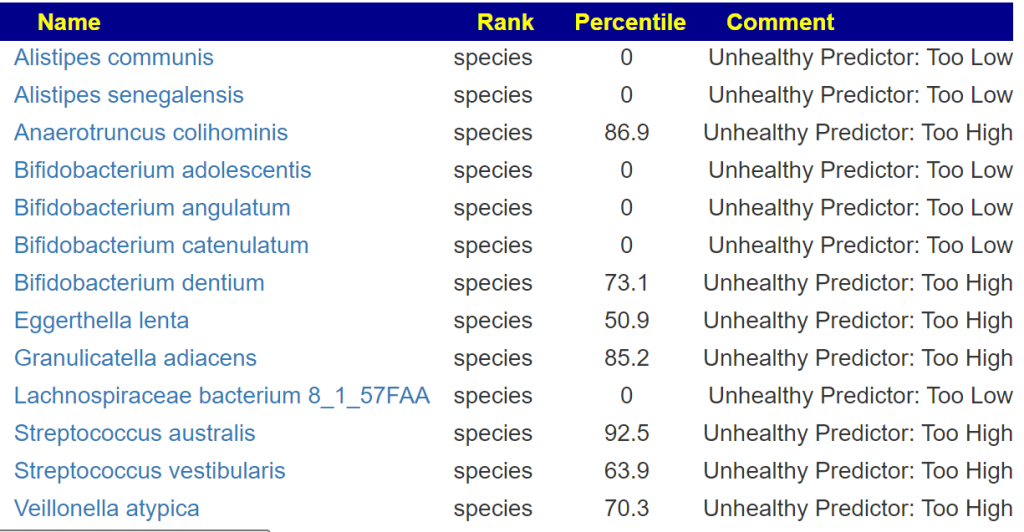
Looking at Bacteria deemed unhealthy, we see the following very significant items.
- Bilophila genus 100%ile High Level Cause Brain Fog(Cognitive impairment) Citation
Addressing the problem
The process is simple, just click this buttom
Then use the filtering button to view different suggestions. The highest priority was 1000, lowest -765 so we will look to take items over 500 and aggressively avoid items below -350. The dosages come from this summary page that links to studies, dosages should be reviewed by your MD before starting.
- Vitamins (All of these are typical for ME/CFS and shown to help in studies).
- Supplements (take at least one of these each week – see above link for suggested dosages)
- melatonin supplement
- Hesperidin (polyphenol)
- Arbutin (polyphenol)
- diosmin (polyphenol)
- luteolin (flavonoid)
- Herbs and Foods
- garlic (allium sativum)
- momordia charantia(bitter melon, karela, balsam pear, or bitter gourd)
- Caffeine
- whole-grain barley
- sucralose
- Probiotics
- lactobacillus kefiri (NOT KEFIR) — available in Italy only 🙁
- Below the 500 threshold but should have some impact
- lactobacillus reuteri (probiotics)
- bifidobacterium infantis,(probiotics)
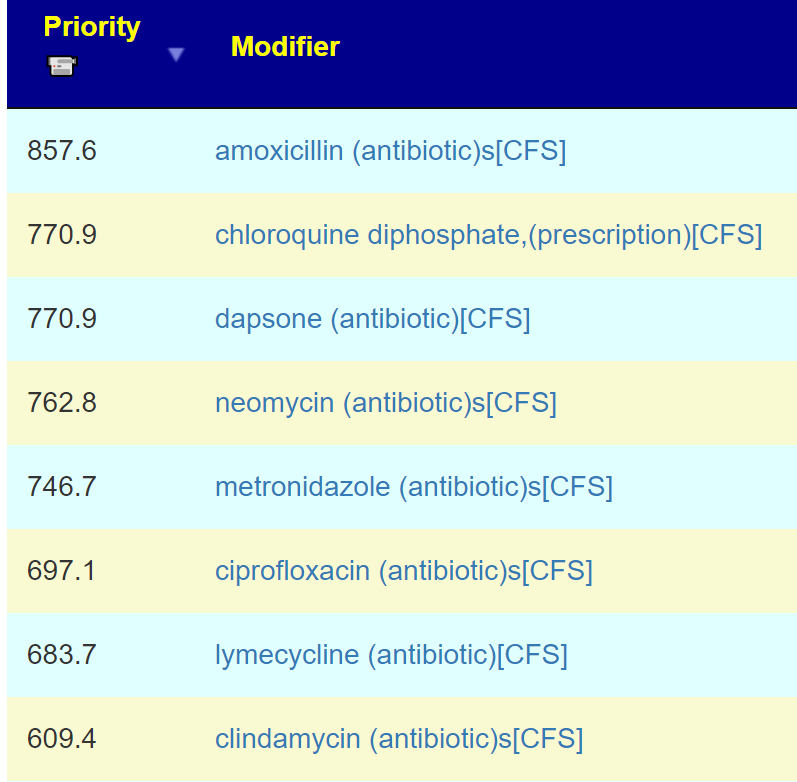
- Antibiotics (only picked those that have been used with ME/CFS by specialists). If done, they should be rotated and pulse (i.e. 7-10 days on one, 3 weeks off; then a different one is used). See Dr. C. Jadin’s approach.
The avoid list is often ignored by people. They should not be. These items feed the undesired shifts.
- Diet Style AVOIDS
- Foods AVOIDS
- Herbs AVOIDS
- Slippery Elm
- berberine
- camellia
- Supplements AVOIDS
- bile (acid/salts)
- arabinogalactan (prebiotic)
- Human milk oligosaccharides (prebiotic, Holigos, Stachyose)
- resistant maltodextrin
- xylan (prebiotic)
- resistant starch
- non-starch polysaccharides
- bacillus licheniformis,(probiotics)
- galactose (milk sugar)
Try for 8 weeks, then retest
While waiting for test results, keep to the suggestions.
- As is common with ME/CFS people, you may want to be done with the disease ASAP so much you toss yourself into it. I have been there and done that. Taking everything at once risk major herx reaction. The key is rotate and pulse. Avoid substances that cause herx that is longer than 6 hours — you are not ready for those, we need to take the longer path instead of trying to climb a cliff face.
- Try this pattern:
- Take the probiotics, herbs and non-vitamin supplements into groups.
- Week 1: take the probiotic for a week (#1 in priority)
- Week 2: take one herb for a week (#1 in priority)
- Week 3: one supplement for a week (#1 in priority)
- Then go back to probiotic BUT take a different one (i.e. #2 in priority), same pattern for other things
- After 8-12 weeks do a retest and see where suggestions have shifted
- The goal is to destabilize a stable dysbiosis. In one sense, we want to do a guerilla war against it, not form up into a line and attempt march to frontal assault.
- Take the probiotics, herbs and non-vitamin supplements into groups.
Questions and Answers
- Do you know if my ME is due to the covid with these results?
- It is impossible to tell from the microbiome. COVID could make an existing case of ME/CFS worse. If you were fine prior, then it is likely that COVID causes ME (i.e. Long COVID). Over time the dysbiosis between ME/CFS and Long COVID become very similar.
- I’m allergic to penicillin (amoxycillin, etc.). What antibiotics can I take without it?
- The best antibiotics that have been used by ME/CFS specialist were computed to be:
- chloroquine diphosphate — anti-malarial and anti-rheumatoid agent and belongs to the drug class 4-aminoquinoline
- dapsone – a sulfone, It works by decreasing swelling (inflammation) and stopping the growth of bacteria
- neomycin – belongs to the aminoglycosides group of antibiotics
- metronidazole – belongs to the nitroimidazole antimicrobials. Metronidazole is one of the mainstay drugs for the treatment of anaerobic bacterial infections, protozoal infections,
- lymecycline – tetracycline antibiotics.
- My own preference would be to start with a tetracycline (lymecycline), followed by metronidazole, and then neomycin. This is largely based on the frequency of use that I have seen in the literature. At that point you should be retested.
- I would follow Jadin’s pattern: 1 week on, 3 weeks off and then rotate to the next antibiotic.
- The best antibiotics that have been used by ME/CFS specialist were computed to be:
Postscript – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I can compute items to take, those computations do not provide information on rotations etc.
I cannot tell people what they should take or not take. I can inform people items that have better odds of improving their microbiome as a results on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting.
The answers above describe my logic and thinking and is not intended to give advice to this person or any one. Always review with your knowledgeable medical professional.
Recent Comments