For other analysis of Microbiomes. see Analysis Posts on Long COVID and ME/CFS.
Backstory
My mom got the AstraZeneca Vaccine last year, after which she didn’t really have any major problems, so later she got her 2nd shot with BionTech/Pfizer. Shortly after she caught Covid. While the course of the disease was very mild, she experienced severe hair loss in the following days, which reverted 6 months later. Also, she started feeling tired fast and could not work anymore (nurse). That was about a year and a half ago.
She developed hypertension after she received the vaccination for COVID
As of now, she still has the same issue with CFS, though it’s gotten better on most days. Some days she gets a crash and doesn’t feel too good. What’s helping her is going outside twice to three times a day for extended walks, and she says when she goes into the pine forest nearby she feels refreshed afterwards.
Her CFS isn’t as severe as my brothers, though it still restricts her from working.\
The Lab used was BiomeSight which ships world wide. An equivalent alternative in the US is Ombre.
Analysis
I am going to do a pro-forma review, i.e. a process that other can follow easily.
My Profile/Health Analysis
- Potential Medical Conditions Detected
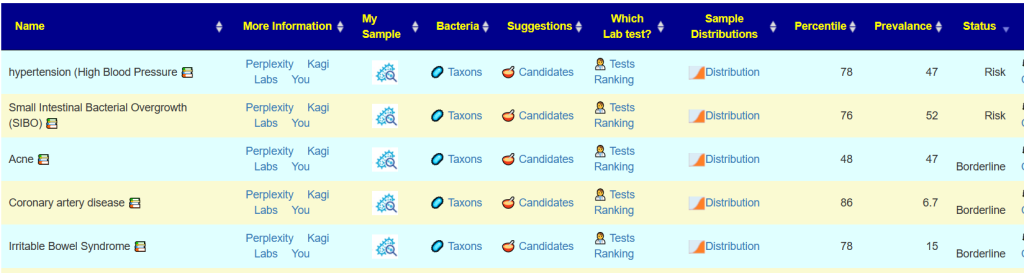
- hypertension (High Blood Pressure 78%ile (12 of 35) prevalence 47%, so likely (and confirmed)
- Acne 48%ile (4 of 20) , prevalence 47% — so very unlikely.
- Bacteria deemed Unhealthy
- Prevotella copri – 86%ile,, 20% of the microbiome
- Dr. Jason Hawrelak Recommendations – 89%ile
- Low Bifidobacterium
- Low Akkermansia
- Low Lactobacillus
- Low Roseburia
- High Bacteroidia
Since we have a condition, Long COVID or ME/CFS, we look at:
- PubMed data first ( After logging in, Go to https://microbiomeprescription.com/Library/PubMed pick the sample OR see bottom of Changing Microbiome tab)
- Long COVID – 3%ile
- ME/CFS without IBS – 82%ile
- ME/CFS with IBS 53%ile
- Chronic Fatigue Syndrome 43%ile
- Citizen Science
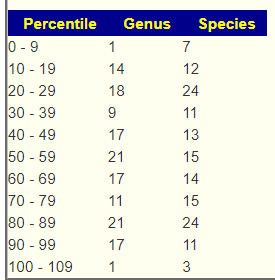
Looking at balance there was no strong shift to the lower or upper.
This leads to using several filtered sets of suggestions:
- PubMed: ME/CFS without IBS
- Citizen Science: ME/CFS without IBS ( 544 candidate bacteria) with highest z-score of 11.1
Proactive Factors
Going to Medical Conditions with Microbiome Shifts from US National Library of Medicine and sorting by status can be used to look at risks of slipping into additional issues. In this case IBS and SIBO are shown — both are commonly associated with ME/CFS. Coronary artery disease has been associated with COVID (“The risk of heart failure increased by 72%” [2022]). These could be included in building consensus suggestions.
Suggestions
- Antibiotics List for MDs produced a list of many antibiotics often prescribed for ME/CFS by some specialist ✅, including:
- macrolide ((antibiotic)s) ✅
- azithromycin,(antibiotic)s ✅
- doxycycline (antibiotic)s ✅
- penicillin-moxalactam (antibiotic)s
- I strongly favor Dr. Cecile Jadin approach which would be do each month a course (7-10 days) of one of the above and then move on to the next one in the following month. (See Manly Conference February 1999)
Building Consensus
We use the 2 above and the following
Kegg Computed Probiotics
Escherichia coli is the top one, which agrees with the Alison Hunter Memorial Foundation presentations in 1998. E.Coli does not get reported in 16s reports and hence tends to be ignored in studies :-(.
Other ones included (in amount of contribution to deficient enzymes):
- Brevibacillus brevis
- Bacillus licheniformis
- Bacillus subtilis
- Bacillus subtilis subsp. natto
- Akkermansia muciniphila
- Clostridium butyricum
- Lactiplantibacillus plantarum
- Enterococcus faecalis
Consensus Report
There was a good long list of items that were suggested by all 5 suggestions sets. A few of note are below:
- raffinose(sugar beet)
- Apple
- Slippery Elm
- fructo-oligosaccharides (prebiotic)
- Lard
- bifidobacterium (probiotics)
- palm kernel meal
- almonds/ almond skins
- zinc
- jerusalem artichoke (prebiotic)
- resveratrol (grape seed/polyphenols/red wine)
Avoids included the following:
- oregano (origanum vulgare, oil) |
- lactobacillus salivarius (probiotics)
- neem , tulsi
- high carbohydrate diet
- Baking Soda (Sodium Bicarbonate)
- chicken
See attached for details.
Bottom Line
This patient history and their microbiome are in agreement. The antibiotics suggestions (off label usage) matches what has been used by some ME/CFS specialists. Light exercise (within tolerance and without causing Post-exertional malaise (PEM)) has been reported to improve ME/CFS and is often suggested by AI. A reader forwarded me this study on walking in the forest: A comparative study of the physiological and psychological effects of forest bathing (Shinrin-yoku) on working age people with and without depressive tendencies [2019] and Effect of forest bathing trips on human immune function [2010] which hints that location, location, location is important. It even comes in a COVID presentation factor, Green spaces, especially forest, linked to lower SARS-CoV-2 infection rates: A one-year nationwide study [2022]. As a FYI, I do “Shinrin-yoku” whenever the weather permits with my three corgis.
I explicitly checked against the new list of Bacteria Triggering Coagulation and Micro clots, and they were none at over 75%ile; so coagulation is unlikely to part of the situation. I view coagulation as a potential feedback loop to keep CFS/Long COVID going. The coagulation drops oxygen levels which encourages the growth of bacteria that produces coagulation – a nasty feed back loop.
Postscript – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I cannot tell people what they should take or not take. I can inform people items that have better odds of improving their microbiome as a results on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting.
The answers above describe my logic and thinking and is not intended to give advice to this person or any one. Always review with your knowledgeable medical professional.
Recent Comments