The question of which bacteria may induce coagulation issues and micro clots with Myalgic encephalomyelitis/chronic fatigue syndrome and Long COVID has been an interest for many years (pre-COVID). This week I started digging (again) and this time we got sufficient information to do a sharing post.
Blood coagulation often accompanies bacterial infections and sepsis and is generally accepted as a consequence of immune responses. Though many bacterial species can directly activate individual coagulation factors, they have not been shown to directly initiate the coagulation cascade that precedes clot formation. Here we demonstrated, using microfluidics and surface patterning, that the spatial localization of bacteria substantially affects coagulation of human and mouse blood and plasma. Bacillus cereus and Bacillus anthracis, the anthrax-causing pathogen, directly initiated coagulation of blood in minutes when bacterial cells were clustered.
Spatial localization of bacteria controls coagulation of human blood by ‘quorum acting‘ [2008]
In Gut Microbiota and Coronary Plaque Characteristics [2022] we actually get some names:
- Paraprevotella had a positive correlation with fibrinogen
- Succinatimonas had positive correlations with fibrinogen and homocysteine
- Bacillus had positive correlations with fibrinogen and high-sensitivity C-reactive protein
- Paraprevotella, Succinatimonas, and Bacillus were also associated with greater plaque volume
Helicobacter pylori, Chlamydia pneumoniae, Mycoplasma pneumoniae, Haemophilus influenzae, Streptococcus pneumoniae, Staphylococcus aureus, Streptococcus pyogenes, Pseudomonas aeruginosa, Klebsiella pneumoniae, Bartonella henselae and Escherichia coli, causing infections may increase the risk of thrombotic complications through platelet activation or may lead to an inflammatory reaction involving the fibrinolytic system. Acinetobacter, Burkholderia pseudomallei [2020]
“The found slight increases in FVIII:C and CRP levels might support the hypothesis that a vancomycin-induced gram-negative shift in the gut microbiome could induce increased systemic inflammation and thereby a procoagulant state.” [2021]
“significantly abundant genera were observed in the coronary thrombus in the patients: Escherichia, 1.25%; Parabacteroides, 0.25%; Christensenella, 0.0%; and Bacteroides, 7.48%. ” [2020]
Bottom Line
I have added this data to the Medical Conditions with Microbiome Shifts from US National Library of Medicine page.
Cross Validation
This means do prediction agree with reasonable expectation.
Looking at the suggestions, they appear to be full of items connected to ME/CFS or to blood thinning
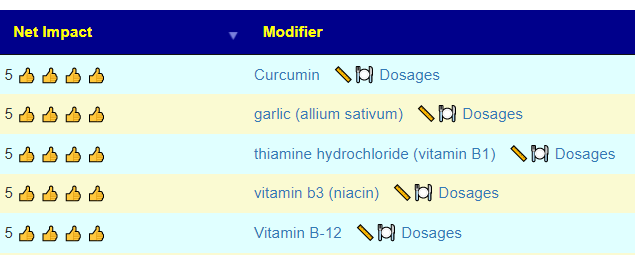
- Curcumin, hemostasis, thrombosis, and coagulation [2018] “support the positive activity of curcumin in hemostasis, anticoagulation, and fibrinolysis.”
- Consumption of a garlic clove a day could be beneficial in preventing thrombosis [1995]
- Evaluation of thiamine as adjunctive therapy in COVID-19 critically ill patients: a two-center propensity score matched study [2021] “it was associated with a lower incidence of thrombosis.”
- Antiatherothrombotic effects of nicotinic acid [2023] –
- Vitamin B12 And Folic Acid Reduce The Risk Of Blood Clots In The Brain [2005]
The artificial intelligence producing these suggestions knows nothing about coagulation, it made these suggestions to solely reduce the bacteria identified above. Bacteria which may cause coagulation.
We would expect more matches for high bacteria levels (defined as > 75%ile) of the bacteria identified above with people with Long COVID and people with ME/CFS. This appears to be shown in the data. The reason that exogene has a very high number is that it reports on all of the candidate bacteria — which is not the case for 16s tests. Second, we see post-COVID people with full recovery having less matches then the combination of samples which includes those that provided no information (and which would likely contain some Long COVID and ME/CFS people)
| Condition Reported | Lab | Reported | Not Reported |
| COVID | BiomeSight | 2.44 | 2.23 |
| Fully Recovered from COVID (No Long Covid) | BiomeSight | 2.28 | |
| ME/CFS | es-xenogene | 6 | 3.25 |
| SequentiaBiotech | 2.5 | 1.3 | |
| OmbreLabs | 2.08 | 1.94 | |
| American Gut | 5.74 | 3.10 | |
| BiomeSight | 2.29 | 2.27 | |
| uBiome | 1.54 | 1.51 |
The list of bacteria above is known to be incomplete but the above results does suggest at least a partial identification of the bacteria responsible for coagulation and micro clots.
This post from 2015, may be of interest to people with coagulation / micro-clots issues: Coagulation: Thick Blood Supplements for CFS and Long COVID
2 thoughts on “Bacteria Triggering Coagulation and Micro clots”
Comments are closed.