After a recent hospital visit for cellulitis (with many different antibiotics, both orally and by IV), my blood pressure was significantly elevated that the substitute MD (my usual was on vacation), that I was put on Lisinopril. Within a week I developed a dry cough that has for 35 years has been a “tell” for a relapse into Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Checking the literature, I found that about 30% of people develop this cough. To me it is an important tell, if it shows up — I need to do quick re-examination of what is going on. For a prescription drug to do so, really made me uncomfortable.
I then check Lisinopril against the bacteria shifts reported for ME/CFS, and it made them worst. In short, staying on it may well increase the risk of relapsing into ME/CFS. That is not acceptable.
I did a little more research and found a variety of different opinions on COVID and the use of ACE2, one example is Long-term ACE Inhibitor/ARB Use Is Associated With Severe Renal Dysfunction and Acute Kidney Injury in Patients With Severe COVID-19: Results From a Referral Center Cohort in the Northeast of France, 2020
In 2019, I had done a posting on hypertension citing Nutrients and Nutraceuticals for the Management of High Normal Blood Pressure: An Evidence-Based Consensus Document. [2019].
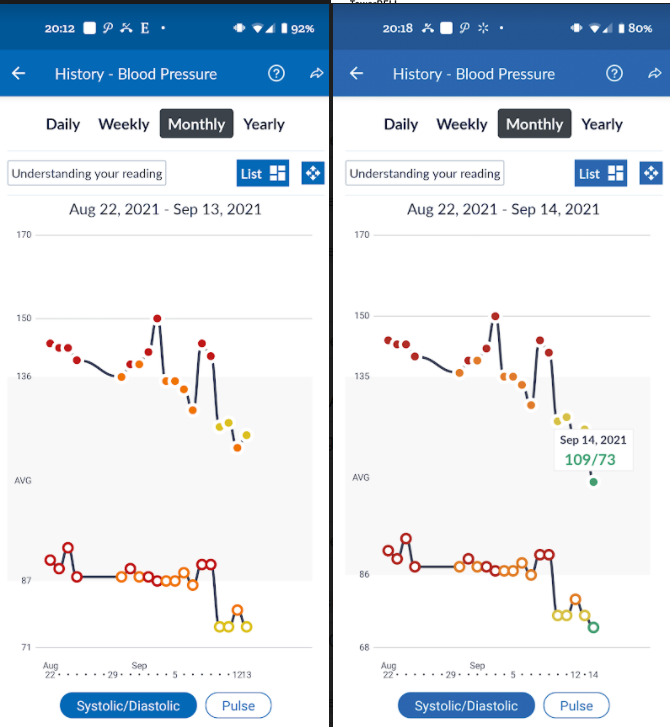
I stopped the lisinopril and proceeded to take the nutrients etc cited above, at or above the specified dosages. I know that it will take a little time for the microbiome to respond, but it did.
Bifidobacterium Correlation
Reviewing the literature, there is the appearance of blood pressure being strongly associated with the amount of bifidobacterium as we age. Children are very high in Bifidobacterium and low in BP. As the typical amount of bifidobacterium decreases with age, blood pressure increases.
I found this recent study,
- The effect of dietary fiber (oat bran) supplement on blood pressure in patients with essential hypertension: A randomized controlled trial [2021] “Increased DF (oat bran) supplement improved BP, reduced the amount of antihypertensive drugs, and modulated the gut microbiota. The use of antihypertensive drugs in the DF group was significantly reduced. The changes[increase] of Bifidobacterium and Spirillum in the DF group were significant.”
As a result, I add 2 tablespoons of bran to the typical 4 table spoons of oats porridge that was doing. I also added a package of Holigos (Human Milk Oligosaccharides) which I know is a super feeder of bifidobacterium.
This corresponded to the severe drop shown above.
Possible Probiotic Impact
I was taking the following based on modelling of the bacteria shifts seen in hypertension:
- Lactobacillus plantarum Lp-115 📚
- Lactococcus lactis JCM5805 (L. lactis plasma) 📚
- Bacillus subtilis DE111 📚
Samples are coming…
Just got notification from the lab that last weeks was received.
One addendum, when I was in hospital for cellulitis, my potassium was very low and I required a (painful) IV of potassium. I examined the amount of potassium that my usual diet provided… It was very low, so I started to supplement with potassium citrate also.
Bottom Line
I was able to normalize (for an almost 70 year old) blood pressure by using existing research and having patience. I believe the key items was encouraging bifidobacterium growth (sorry, bifidobacterium probiotics do not persist usually and have little impact), correcting mineral content (potassium, magnesium, calcium).
One more addendum, I usually did 10,000 steps a day with weekend hikes often being as high as 20,000 steps.
Recent Comments