Request
This person has ME/CFS and is familiar with Cecile’s Protocol (see her 2023 presentation here). So my focus will be atypically on antibiotics.
I have just uploaded a new sample and I wanted to ask you if “just give me suggestions” is enough in order to get suggestions regarding a new antiobiotic therapy? Or is there anything else you would recommend me to check on your site?
From Email
Antibiotics Analysis
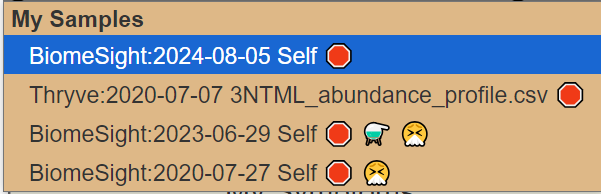
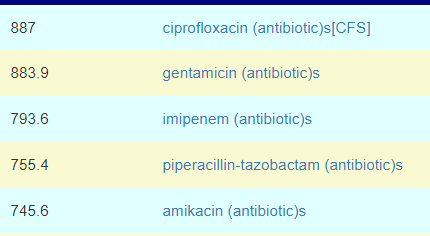
First, we have multiple samples available. Given that the microbiome is always changing. A first sample in the morning and last sample in the evening will rarely agree, I will actually review the suggestions from all 4 samples.
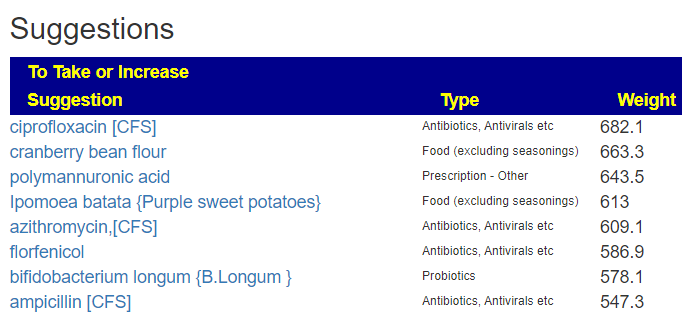
The table below contain only antibiotics that have been tried (with some degree of success) for ME/CFS
| Antibiotic | BS 2020 | Th 2020 | BS 2023 | BS 2024 |
| amoxicillin [CFS] | 137 | 181 | 743 | 746 |
| ampicillin [CFS] | 266 | -19 | 460 | 581 |
| azithromycin,[CFS] | -33 | 104 | 260 | 413 |
| chloroquine diphosphate,(prescription)[CFS] | -30 | -29 | 156 | 190 |
| ciprofloxacin [CFS] | 617 | 128 | 663 | 989 |
| clarithromycin [CFS] | -70 | 41 | 211 | 327 |
| clindamycin [CFS] | 180 | 282 | 654 | 479 |
| dapsone (antibiotic)[CFS] | -12 | -1 | 253 | 105 |
| doxycycline [CFS] | -110 | 57 | 378 | 94 |
| erythromycin [CFS] | -30 | 75 | 531 | 381 |
| lymecycline (antibiotic)[CFS] | -14 | -19 | 313 | 537 |
| metronidazole [CFS] | 192 | 445 | 582 | 707 |
| minocycline [CFS] | 65 | -30 | 326 | 377 |
| neomycin [CFS] | -11 | 69 | 144 | 289 |
| vancomycin (antibiotic)[CFS] | 40 | 92 | 547 | 418 |
My impression is that a round of metronidazole, followed by amoxicillin, followed by a short round of ciprofloxacin appears to be consistent with the pattern of suggestions. From perplexity, I got:
Amoxicillin showed a moderate risk with an adjusted odds ratio of 2.29 (95% CI, 2.02, 2.60). However, it’s important to note that amoxicillin/clavulanate had a much higher risk than amoxicillin alone
Ciprofloxacin, a fluoroquinolone, had a risk level closer to later-generation cephalosporins with an odds ratio of 6.83 (95% CI, 6.56–7.10).
Perplexity
Analysis
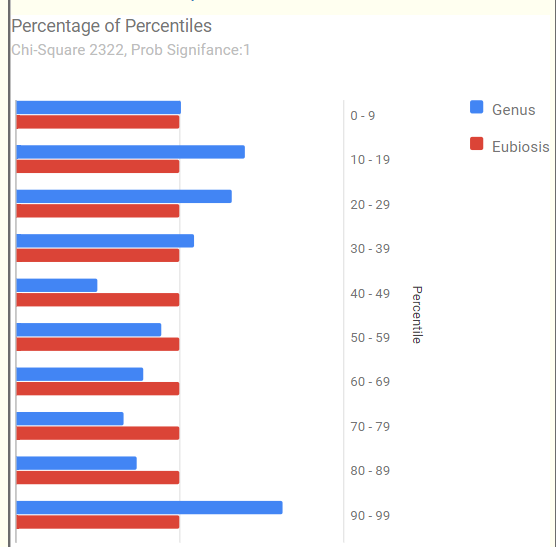
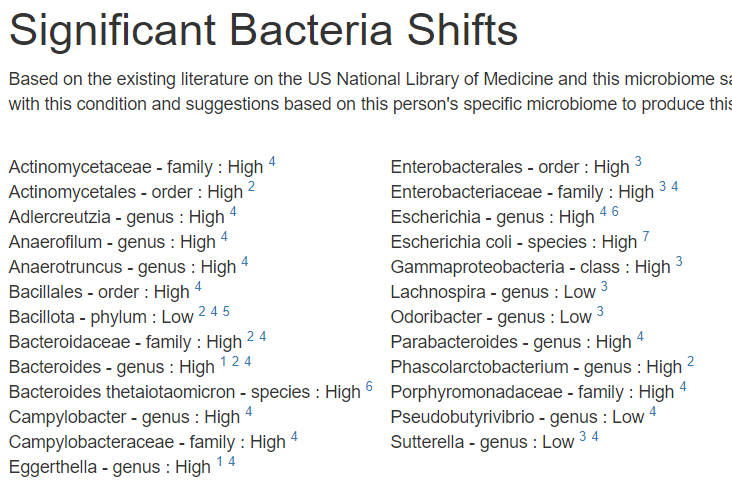
Since we have two samples over time from the same labs, I usually like doing a high level compare. First, the classic comparison which shows the two samples do not have major shifts. An increase of low enzymes usually points me to probiotics via KEGG computations.
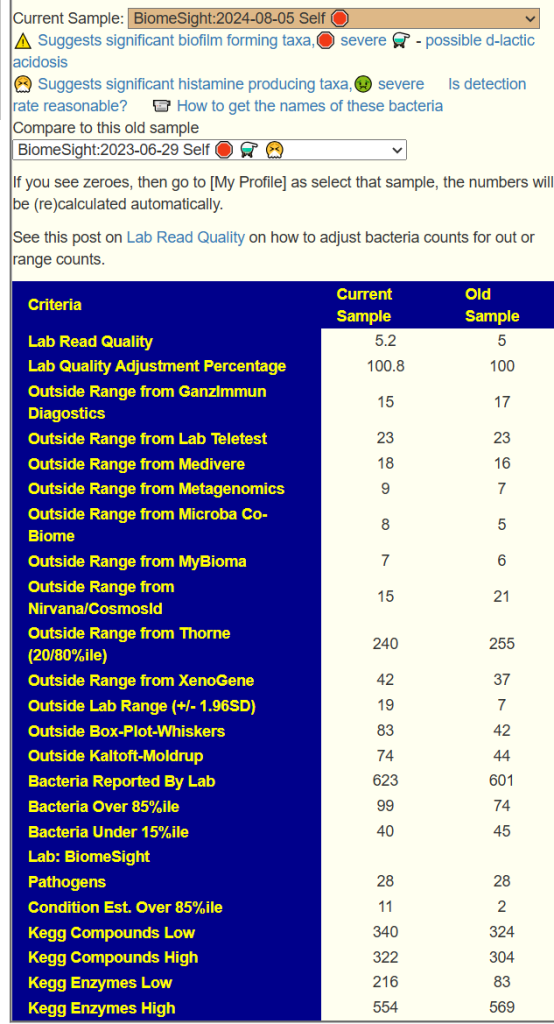
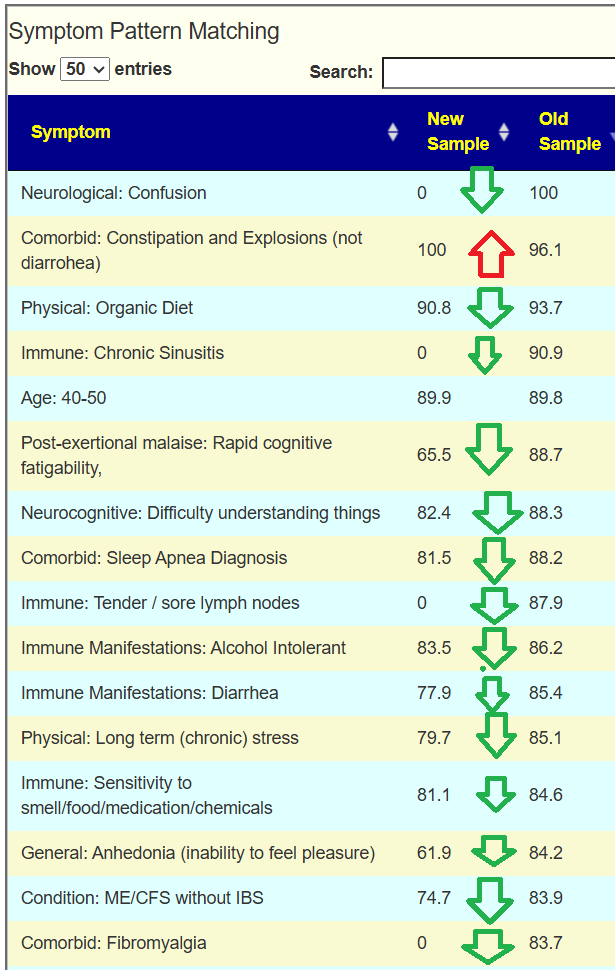
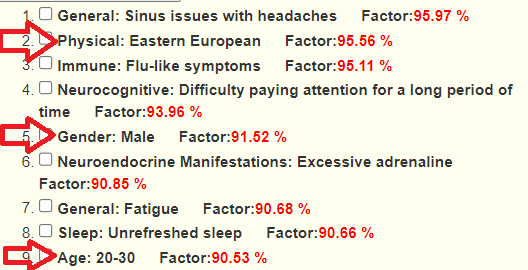
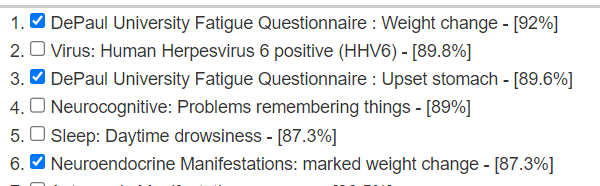
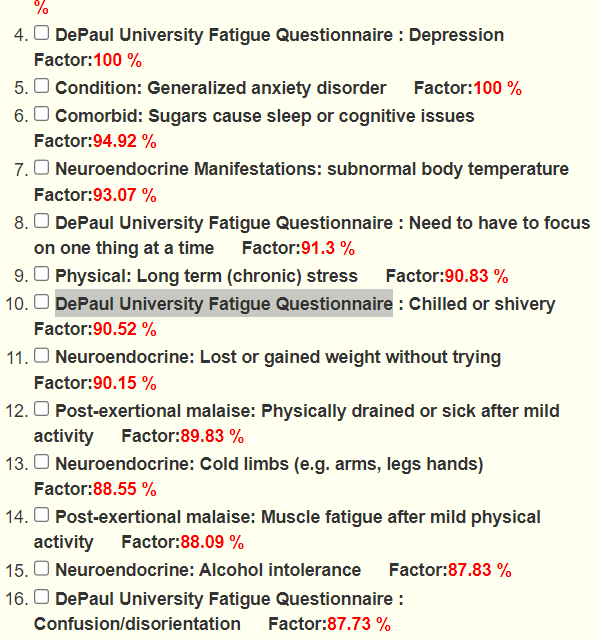
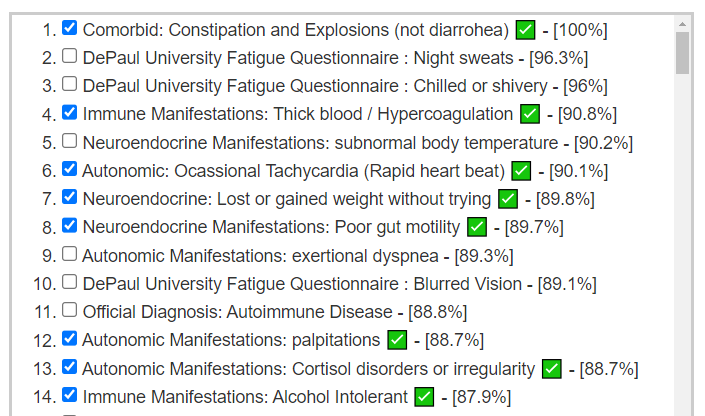
Looking at the new Symptom Pattern Matching, we see a definite improvement (defined as having less bacteria matching symptom patterns). The amount was not huge, but it shows positive change.
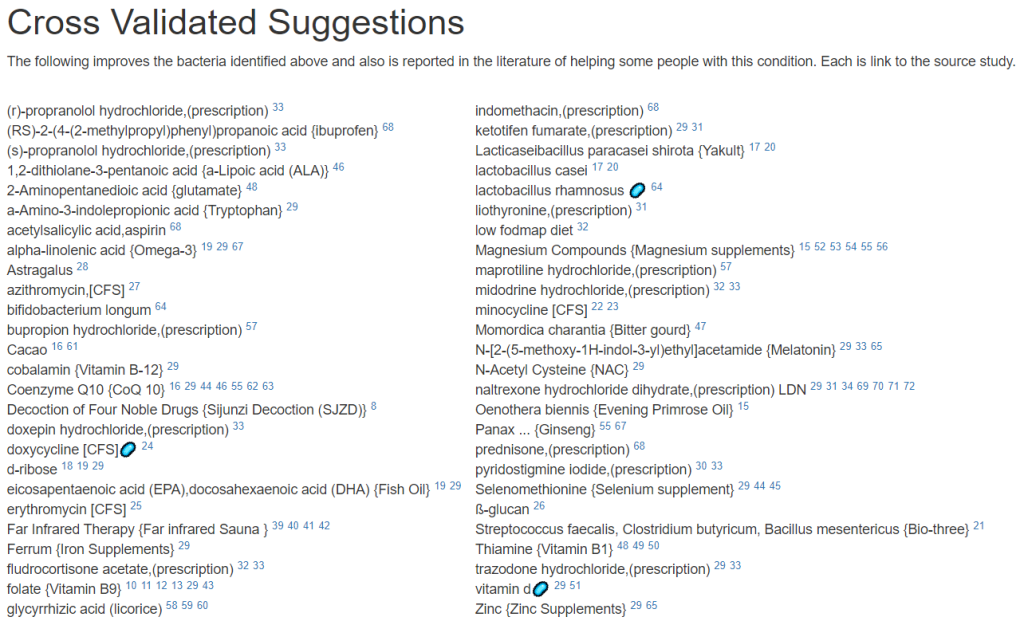
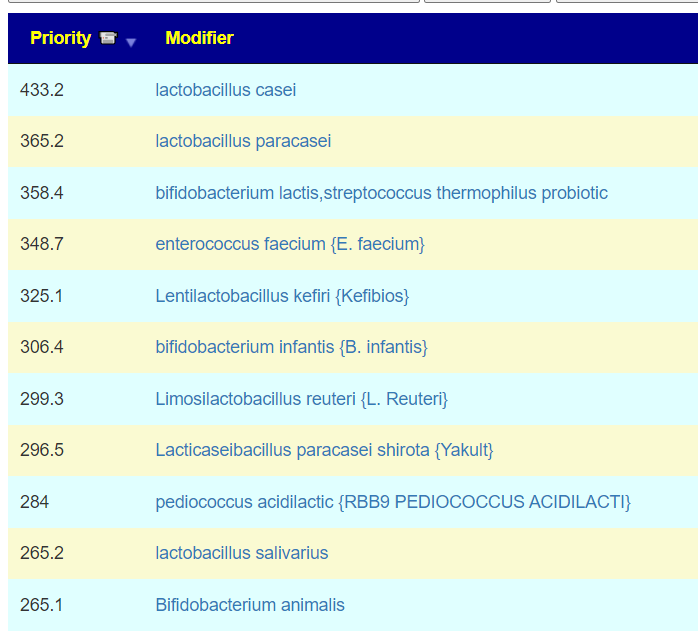
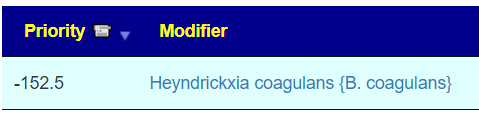
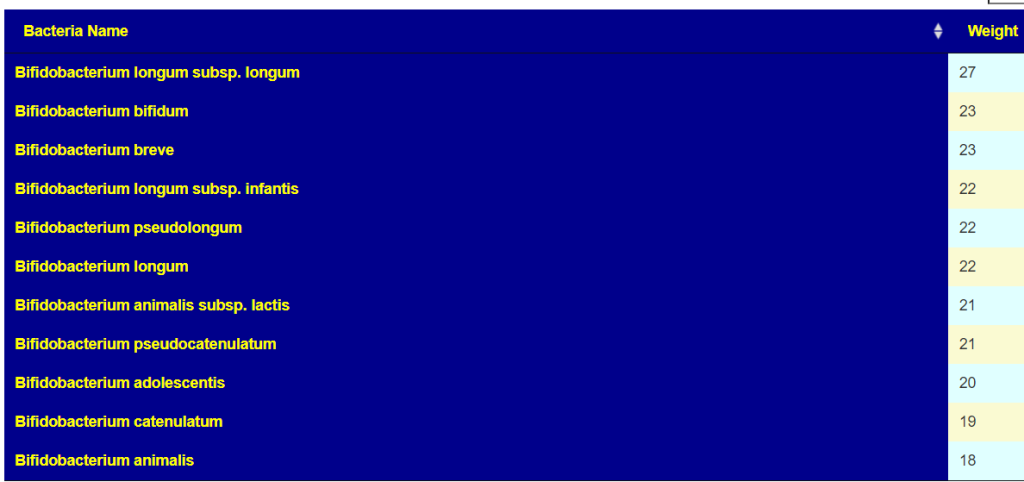
Probiotics
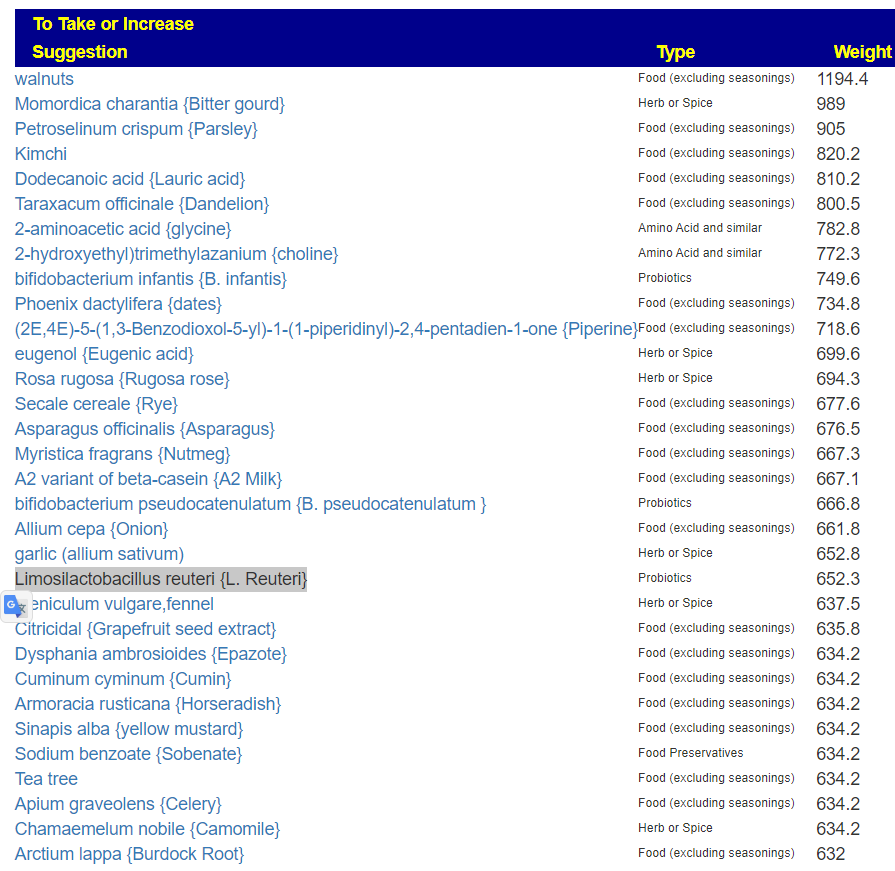
The top ones are below:
- Limosilactobacillus reuteri {L. Reuteri} [5.48]
- enterococcus faecium {E. faecium}
- bifidobacterium infantis {B. infantis} [5.79]
- pediococcus acidilactic {RBB9 PEDIOCOCCUS ACIDILACTI}
- bacillus subtilis [5.7]
- Clostridium butyricum MIYAIRI 588 (CBM 588) {Miyarisan} [6.7]
- Bifidobacterium breve {B. breve} [5.05]
- lactobacillus casei [6.29] CustomProbiotics.com / L. Casei Probiotic Powder
- lactobacillus rhamnosus gg [6.2]
From KEGG Analysis using deficient enzymes we have:
- Maple Life Science™ / Bacillus mesentericus [6.41] – there are very few studies using this, so it missing on the above list is not unexpected.
When there is a good agreement between the studies based (PubMed) and KEGG Enzyme based suggestions for probiotics, it makes them a priority.
Other Items
- Amino Acid and similar: {glycine}, {Theanine}, {choline}, {Taxifolin}
- Common and OTC Supplements: Tudca
- Diet Style: whole-grain diet
- flavonoids, polyphenols etc: quebracho, {Fisetin}
- Prebiotics and similar: {Chicory}, {gum arabic}, {Psyllium}
- Vitamins: {Vitamin B2} {Vitamin B-12} {Calcium Supplements} {Selenium supplement} {Vitamin A} {Vitamin B7}
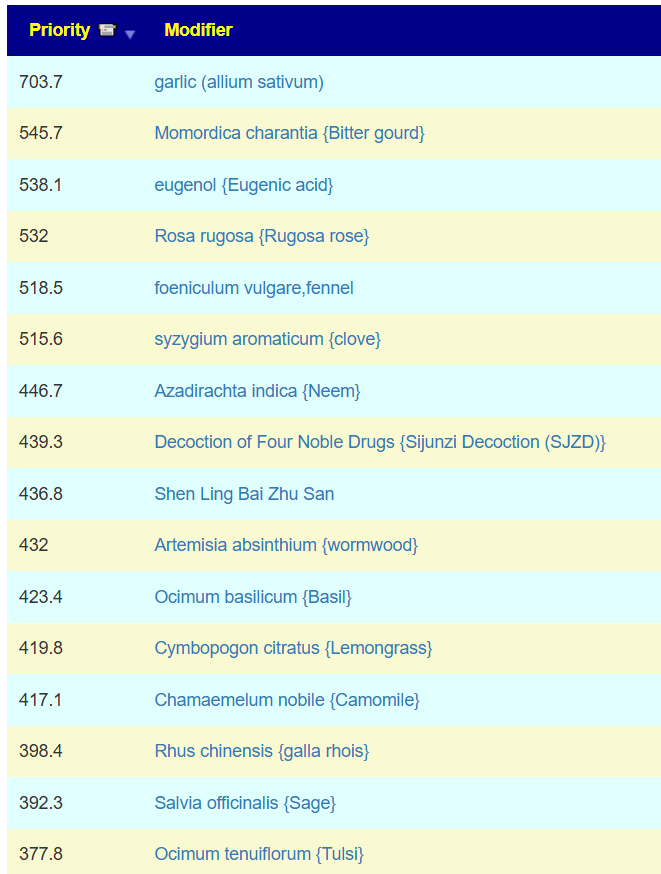
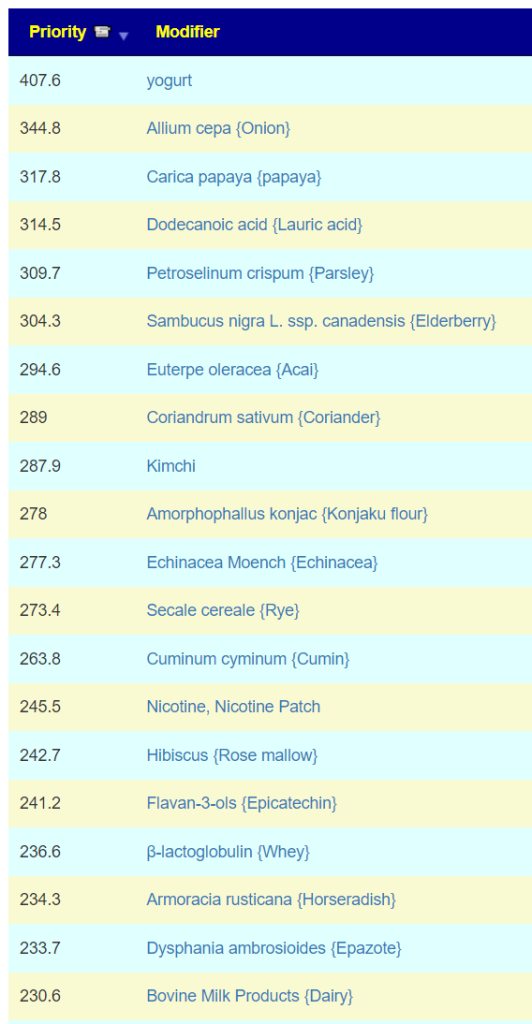
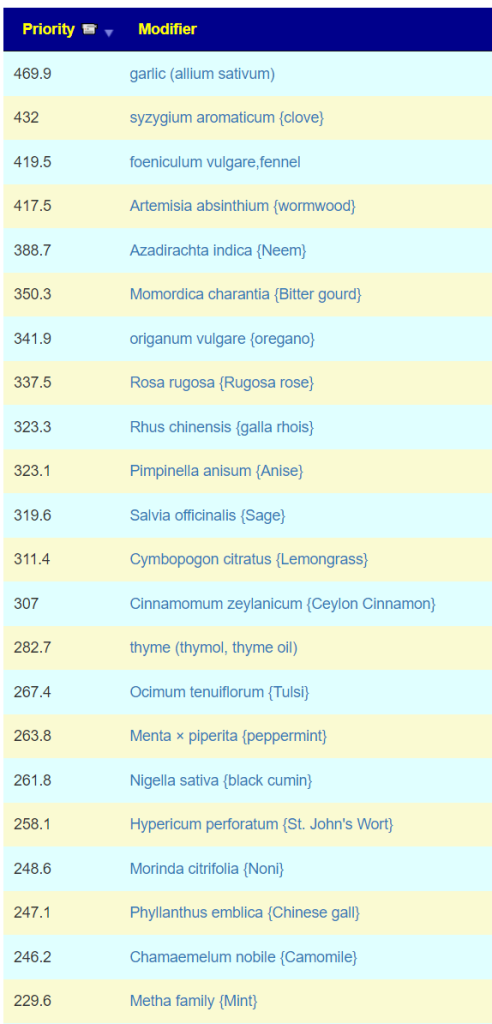
- Food, Herbs and spices

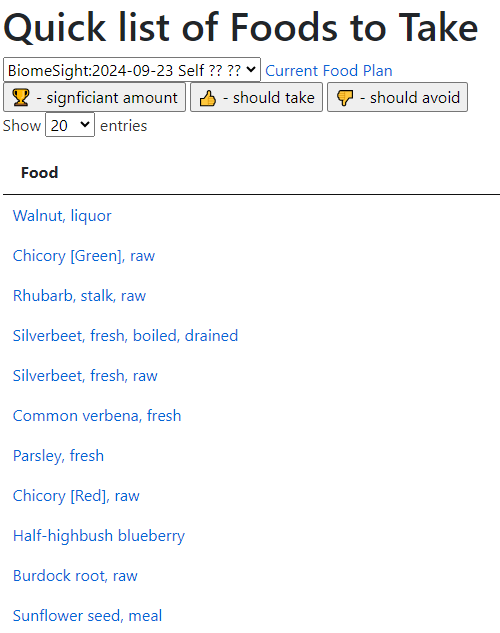
Using the new Simple UI
A quick check of symptoms entered versus forecasted had a low match ratio and identified just 7 bacteria, all low: Streptococcus, Rhodospirillaceae, Oribacterium, Natronincola, Lactobacillales, Blautia and Bacilli.
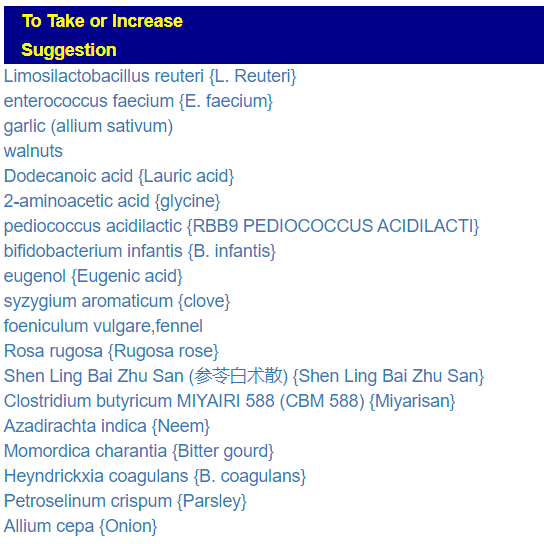
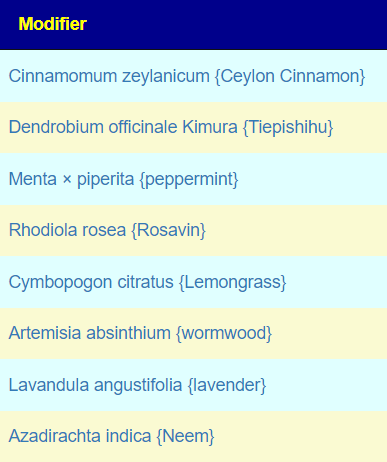
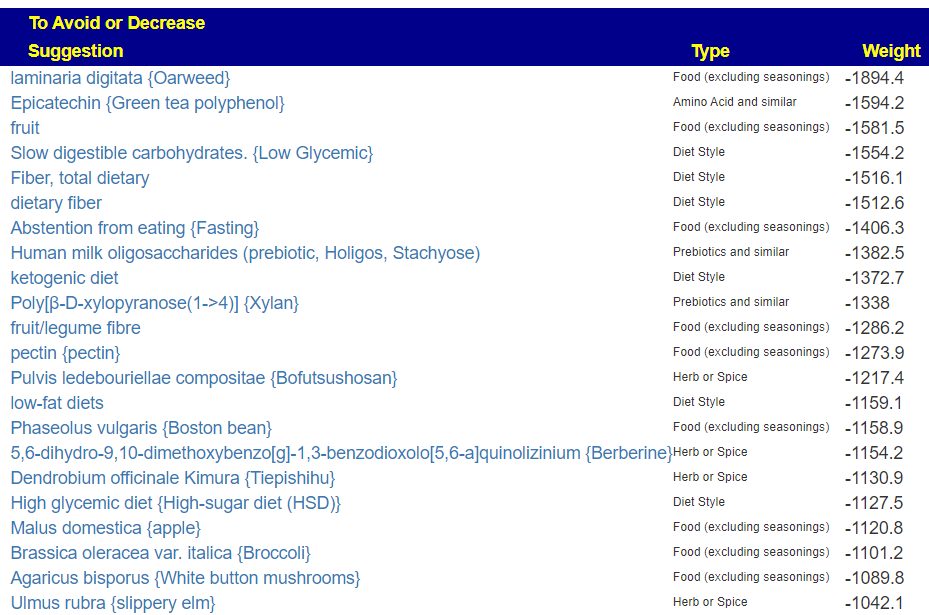
The suggestions to correct these 7 are below. Because all of these are LOW, antibacterial herbs are usually on the avoid list.
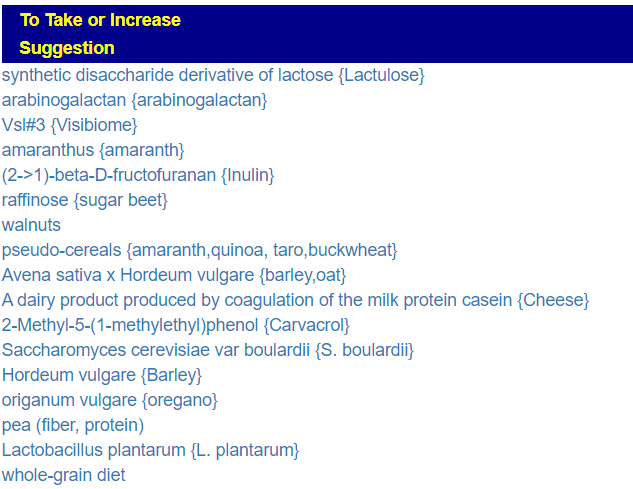 | 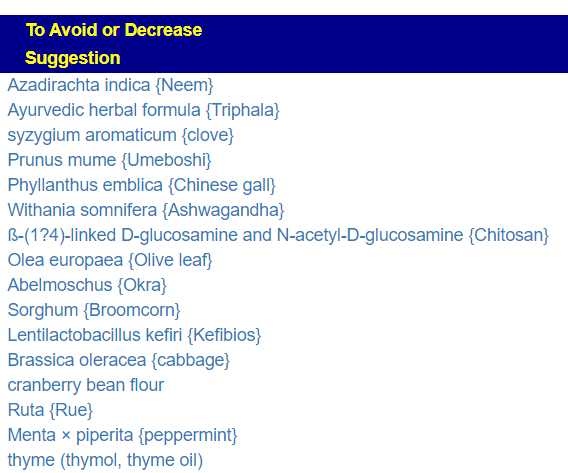 |
Going to the default Novice choice, we get 38 bacteria with both highs and lows. As expected, we have some things changed from avoid to take – for example Neem. The bacteria selected makes a major impact on the suggestions (and why I keep working on better ways of selecting bacteria).
 | 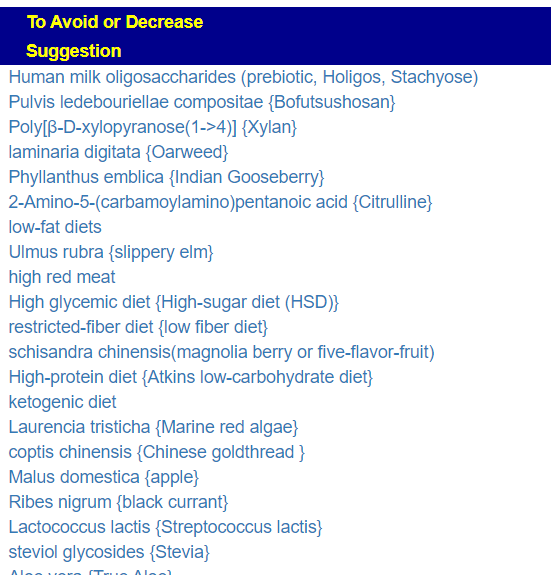 |
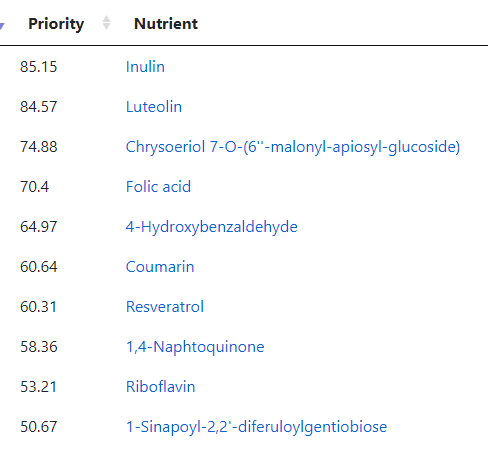
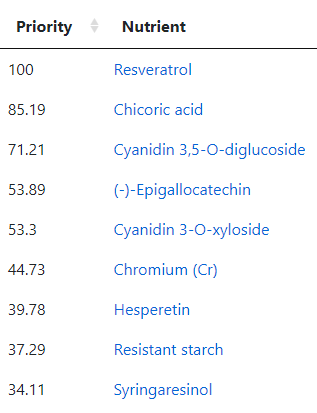
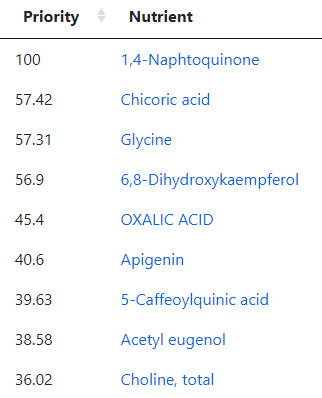
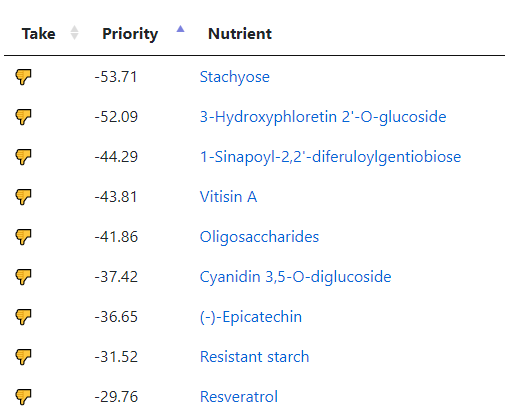
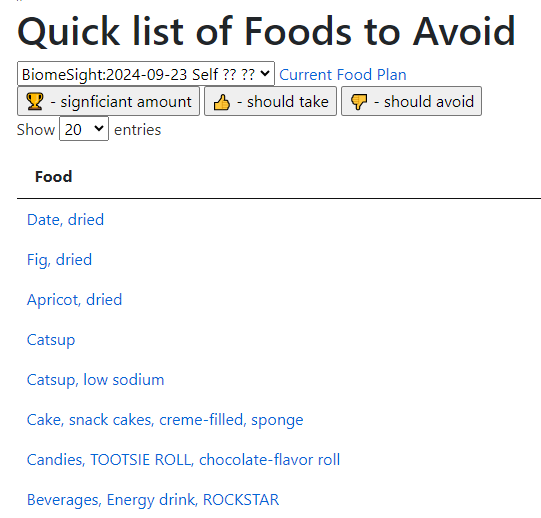
The Food Site is now working again so we can see the suggested best nutrients. The purpose of the Food Site is to transform scientific chemical names (nutrients) into foods.
 | Mexican oregano, dried x2 Chicory [Green], raw Zinc Olive, oil Watercress, Peanut, Almond x 2 Fennel x 2 Common thyme, fresh Globe artichoke, heads, raw Common sage, fresh Red huckleberry Celery seed |
And items to avoid by the food site:
- Indian bean, Chinese Foxglove
- Apple, American cranberry
- broad/Lima/KIdney Bean, Lentil,Pea, Chickpea,
- Red wine, Cloves, Peanut, Broccoli
All of these are based on the nutrients in these foods and the good/harmful nutrients calculated.
Postscript and Reminder
As a statistician with relevant degrees and professional memberships, I present data and statistical models for evaluation by medical professionals. I am not a licensed medical practitioner and must adhere to strict laws regarding the appearance of practicing medicine. My work focuses on academic models and scientific language, particularly statistics. I cannot provide direct medical advice or tell individuals what to take or avoid.My analyses aim to inform about items that statistically show better odds of improving the microbiome. All suggestions should be reviewed by a qualified medical professional before implementation. The information provided describes my logic and thinking and is not intended as personal medical advice. Always consult with your knowledgeable healthcare provider.
Implementation Strategies
- Rotate bacteria inhibitors (antibiotics, herbs, probiotics) every 1-2 weeks
- Some herbs/spices are compatible with probiotics (e.g., Wormwood with Bifidobacteria)
- Verify dosages against reliable sources or research studies, not commercial product labels. This Dosages page may help.
- There are 3 suppliers of probiotics that I prefer: Custom Probiotics , Maple Life Science™, Bulk Probiotics: see Probiotics post for why
Professional Medical Review Recommended
Individual health conditions may make some suggestions inappropriate. Mind Mood Microbes outlines some of what her consultation service considers:
A comprehensive medical assessment should consider:
- Terrain-related data
- Signs of low stomach acid, pancreatic function, bile production, etc.
- Detailed health history
- Specific symptom characteristics (e.g., type and location of bloating)
- Potential underlying conditions (e.g., H-pylori, carbohydrate digestion issues)
- Individual susceptibility to specific probiotics
- Nature of symptoms (e.g., headache type – pressure, cluster, or migraine)
- Possible histamine issues
- Colon acidity levels
- SCFA production and acidification needs
A knowledgeable medical professional can help tailor recommendations to your specific health needs and conditions.

Recent Comments