I have known for years that conventional MD knowledge often trail science by generations. It means that patients need to educate themselves (and in some cases, their MD). The first example is simple:
Stress being the Cause of Ulcers
The discovery that ulcers are caused by bacteria, specifically Helicobacter pylori, was made by Australian researchers Barry Marshall and Robin Warren in 1982. They identified H. pylori as a major cause of gastritis and peptic ulcer disease, challenging the prevailing belief that stress and lifestyle factors were the primary causes of ulcers.[23 years of the discovery of Helicobacter pylori: Is the debate over?]. In 1994, the National Institutes of Health (NIH) held a consensus meeting that concluded the key to treating gastric and duodenal ulcers was the detection and eradication of H. pylori. Then it spent the next decade educating MDs.
But wait! John Lykoudis, MD. after treating himself for peptic ulcer disease with antibiotics in 1958 and finding the treatment effective, Lykoudis began treating patients with antibiotics. After experimenting with several combinations of antibiotics he eventually arrived at a combination which he termed Elgaco and which he patented in 1961. So it took 4 decades from demonstration to acceptable practice.
BMI and Life Expectancy
If you go to CDC Calculator for BMI, Age is not a factor
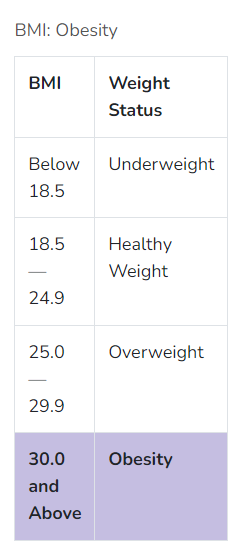
“One BMI will rule them all”. Except, if we are talking about health — this is wrong
Older adults with BMI <25 and >35 kg/m2 were at a higher risk of a decrease in functional capacity, and experienced gait and balance problems, fall risk, decrease in muscle strength, and malnutrition. Data from this study suggest that the optimum range of BMI levels for older adults is 31–32 and 27–28 kg/m2 for female and male, respectively.
Going to What is the Optimal Body Mass Index Range for Older Adults? [2022]
Where as CDC shows this evaluation and would encourage older people to move to an unhealthy BMI. As a FYI, I am at 31.7 and working to reduce to 28 using probiotics see Probiotics, Obesity and Diabetes.
Blood Pressure and Stroke Risks
For those over 65, a recent study Association of Blood Pressure With Stroke Risk, Stratified by Age and Stroke Type, in a Low-Income Population in China: A 27-Year Prospective Cohort Study [2019] found some very interesting results. If you over 65 and have BP < 130, you actually have an increased risk of stroke (i.e. 1/.80) = 25% greater odds of having a stroke then if you were in the 130-140 range. In the 140-150 range, it is a toss up — with odds of one type of stoke still low and the other marginally increasing.
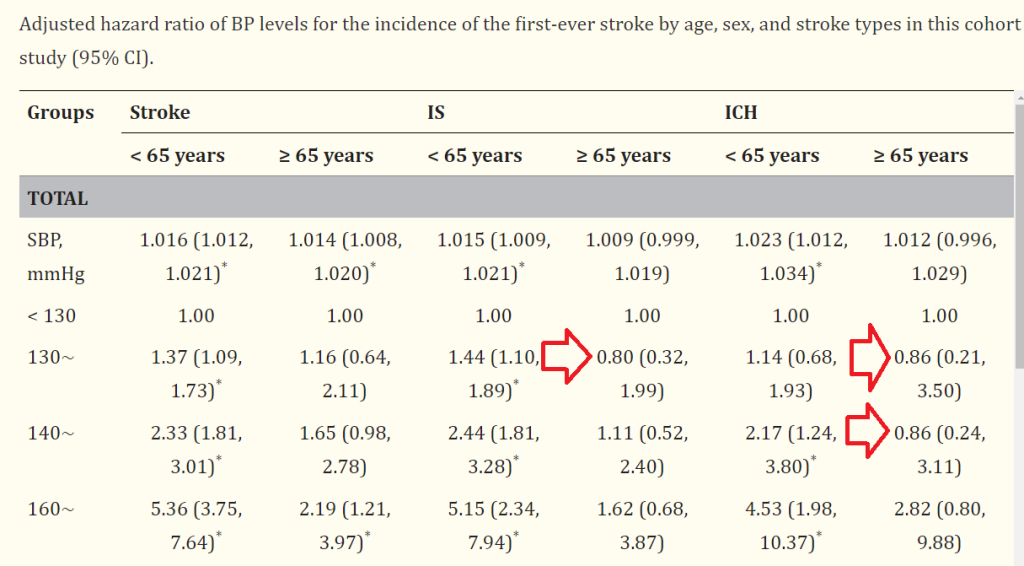
Among older Japanese adults with isolated systolic hypertension and baseline SBP values ≥160 mm Hg, the on-treatment SBP level at which CVD event risks and all-cause mortality were minimized was 130 to < 145 mmHg. On-treatment SBP values of < 130 or ≥145 mmHg were associated with increased CVD event risk and all-cause mortality.
On-Treatment Blood Pressure and Cardiovascular Outcomes in Older Adults With Isolated Systolic Hypertension [2017]
Isolated systolic hypertension (ISH) is a condition characterized by an elevated systolic blood pressure (the top number) of 130 mm Hg or higher, while the diastolic blood pressure (the bottom number) remains below 80 mm Hg
Bottom Line
The reality is that your MD knowledge may be stale and not in agreement with the latest research. Use the US National Library of Medicine to find the latest research — be specific for age and gender in your research. Share it with your MD.
Recent Comments