Today, I looked at the bacteria associated to histamine conditions and found the quality of research lacking. I had imported a lot of data from Alison Vickery web site. Unfortunately some of the bacteria cited as producing histamines according to Kyoto Encyclopedia of Genes and Genomics lack the enzymes to produce histamine. Today, I spent the morning checking published studies on the US National Library of Medicine to see if there is any evidence of histamine production there — little luck. As a result, I deleted the data since it was not at the desired quality.
Quick Summary
- It is strongly recommended that the sources be read before taking any actions
- Items that may help:
- DAO
- Anti-Histamines
- HNMT histamine N-methyltransferase (prescription)- is possible help
- Items to Avoid:
- Vitamin B1
- Vitamin C
- Histamine Liberators [2015] – Many of these items have zero histamine (research is sparse)
- Tomatoes, eggplant, spinach, fish, chicken and every stored meat. All fermented food (cheeses, sausages, sauerkraut, wine, beer, champagne …
- Pineapple, bananas, citrus fruits, strawberries, nuts, papaya, tomatoes, liquorice, spices, legumes, cocoa [2021] [2005], alcohol; fish, seafood, pork, egg white
- MECHANISM: “The presence of putrescine, which may interfere with histamine degradation by the DAO enzyme at the intestinal level, could partly explain the reason why certain foods (i.e., citrus fruits and bananas) were also frequently reported in low-histamine diets” [2021] This link has a table showing the amount in various foods.
- In Medicine:
- Painkillers (morphine, pethidine, codeine, metamizole, antiflogistics (acetylsalicylic acid), antibiotics (d-cycloserine, chloroquin, pentamidine), anti-hypotensives (dobutamine), antihypertensive drugs (verapamil, alprenolol), antitussives (codeine), cytostatics (cyclophosphamide), diuretics (amilorid), iodine-containing contrast medium, local anaesthetics (mesocaine, procaine, marcaine, prilocaine), muscle relaxant (d-tubocurarin), narcotics – anaesthetics (barbiturates, thiopental) Painkillers – antipyretics (acetylsalicylic acid, diclofenac, flurbiprofen, indomethacin, ketoprofen, mefenamin, naproxen…)
- DAO Reducers:
- Antiarrhythmics (verapamil, propafenone), antibiotics (cefuroxime, cefotiame, acidum clavulanicum, doxycyclinum, isoniazid, framycetin), painkillers (metamizole), antidepressants, psychiatric medication (amitriptiline, diazepam, inhibitors MAO–1, haloperidol), antiemetics (metoclopramide), antihistamines (promethazine, cimetidine), antihypertensive drugs (dihydralazine), antimalarials (chloroquin), bronchodilators (aminophylline, theophylline), diuretics (furosemide), mucolytics (N-acetylcysteine, ambroxol), muscle relaxant (alcuronium, pancuronium, d-tubocurarin), antiseptics (acriflavinium chloride), chinidin
- Aspirin (Acetylsalicylic acid)
- NAC (N-Acetylcysteine) aka Acetylcysteine
- L-Glutamine [2022]
- Nonsteroidal anti-inflammatory drugs
- ibuprofen.
- naproxen.
- diclofenac.
- celecoxib.
- mefenamic acid.
- etoricoxib.
- indomethacin.
See below for detail
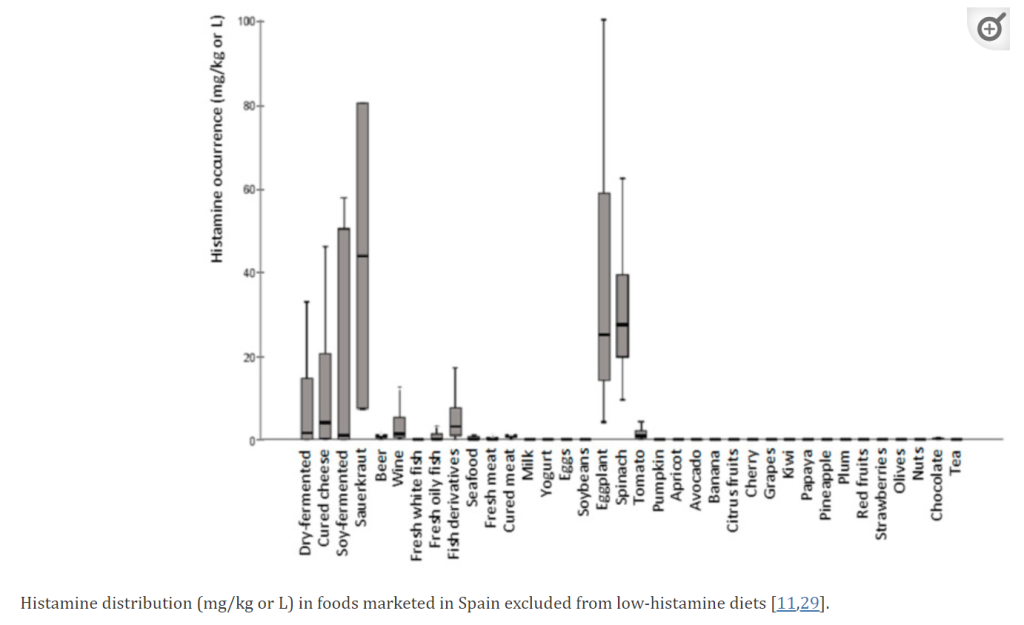
From Low-Histamine Diets: Is the Exclusion of Foods Justified by Their Histamine Content? [2021]
The PDF below is from the Swiss Interest Group Histamine Intolerance (SIGHI) food list that appears to be awesome! They also have a smart phone application.
Analysis and Research
This post is the next step — checking the latest literature and summarizing it in this post. I jump started by using Perplexity.
- Genetic Factors
- “An increased risk for migraines was demonstrated in patients with some DAO genotypes and allelic variants” [2015]
- Genetic mutations that result in lower production or impaired function of the DAO enzyme, which breaks down histamine.
- SNP: Amine Oxidase Copper Containing 1 (AOC1) [2023]
- rs2052129 (minor allele T) [2011][2024]
- rs2268999 (minor allele T) [2011][2024]
- rs10156191 (minor allele T) [2011][2024]
- rs1049742 (minor allele T) [2011][2024]
- rs1049793 (minor allele G) [2011][2024]
- rs1050891 (C314T polymorphism) with the minor T allele [2010]
- Gastrointestinal Disorders
- Medications: Certain medications like antibiotics, antidepressants, antiarrhythmics, muscle relaxants, and NSAIDs can inhibit DAO activity or block histamine breakdown. Table below is from a [2021] article.
| Medications | Generic Name |
|---|---|
| Analgesics | Acetylsalicylic acid, Metamizole, Morphines, Nonsteroidal anti-inflammatory drugs, Pethidine |
| Antiarrhythmics | Propafenon |
| Antibiotics | Cefuroxime, Cefotiam, Isoniazid, Pentamidine, Clavulanic acid, Chloroquine |
| Antidepressants | Amitriptylline |
| Antifungal | Pentamidine |
| Antihypertensives | Verapamil, Alprenolol, Dihydralazine |
| Antihypotensives | Dobutamine |
| Antimalarial | Chloroquine |
| Broncholytics | Aminophylline |
| Cytostatics | Cyclophosphamide |
| Diuretics | Amiloride |
| H2 receptor antagonists | Cimetidine |
| Local anesthetics | Prilocaine |
| Motility agents | Metoclopramide |
| Mucolytics | Acetylcysteine, Ambroxol |
| Muscle relaxants | Pancuronium, Alcuronium, D-Tubocurarin |
| Narcotics | Thiopental |
| Vitamins | Ascorbic acid (Vitamin C), Thiamine (Vitamin B1) |
- Diet: Consuming foods rich in histamine (aged cheese, fermented foods, alcohol, etc.) can overwhelm the body’s ability to break down histamine, leading to an accumulation.
- Repeatedly state with reference in this [2021] study.
- Low-Histamine Diets: Is the Exclusion of Foods Justified by Their Histamine Content? [2021]
- “The dietary treatment of histamine intolerance reduces the abundance of some histamine-secreting bacteria of the gut microbiota in histamine intolerant women. A pilot study” [2022]
- “Reduction of Proteus and Raoultella and the species Proteus mirabilis. “
- Perplexity AI suggested: “Conditions like inflammatory bowel disease (IBD), leaky gut syndrome, and other gastrointestinal disorders can impair DAO production and histamine breakdown.” Unfortunately it’s sources were poor. Checking PubMed, we see the following studies indicate that it appears to apply possibly apply only to one type of IBS.
- “DAO levels were significantly higher in Crohn’s patients with the active stage compared to controls.” [2019]
- “histamine levels were normal in CD and UC.” [2015]
- “subjects with irritable bowel syndrome[IBS] could be discriminated from healthy controls using their metabolic fingerprints… Levels of some urinary metabolites including histamine correlated significantly with irritable bowel syndrome symptom severity scores.” [2019]
- “The mast cells’ histamine release appears linked to GI-involving diseases like celiac disease (CD), eosinophilic gastroenteritis (EGE), and mast cell activation syndrome (MCAS) “[2020]
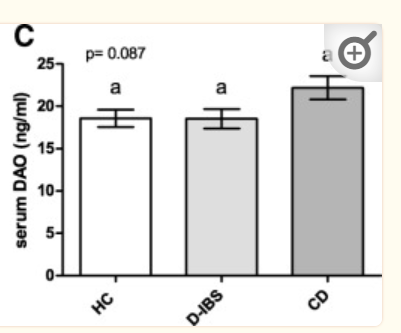
The above chart from Noninvasive biomarkers of gut barrier function identify two subtypes of patients suffering from diarrhoea predominant-IBS: a case-control study [2018] shows there is not a reduction of DAO with IBS, and an increase with Crohn’s Disease (as cited in another study above). When IBS was decomposed by type, one was below the controls and the other was above the controls (same level as CD).
- Intestinal barrier dysfunction: Impaired intestinal barrier function (leaky gut) can allow increased absorption of histamine from the gut into the bloodstream, contributing to histamine overload.
- No clear strong evidence found, a reasonable speculation
- But evidence of bacteria shifts:
- Bacterial overgrowth: An overgrowth of certain bacteria in the gut can lead to excessive production of histamine, overwhelming the DAO enzyme’s capacity to break it down
- “a significantly higher abundance of histamine-secreting bacteria, including the genera Staphylococcus and Proteus, several unidentified genera belonging to the family Enterobacteriaceae and the species Clostridium perfringens and Enterococcus faecalis” [2022]
Probiotics
For a list of studies, click here. The following has some evidence of reducing histamines
- Bifidobacterium bifidum
- Bifidobacterium lactis
- Enterococcus faecium
- Lactobacillus casei Shirota
- Lactobacillus paracasei
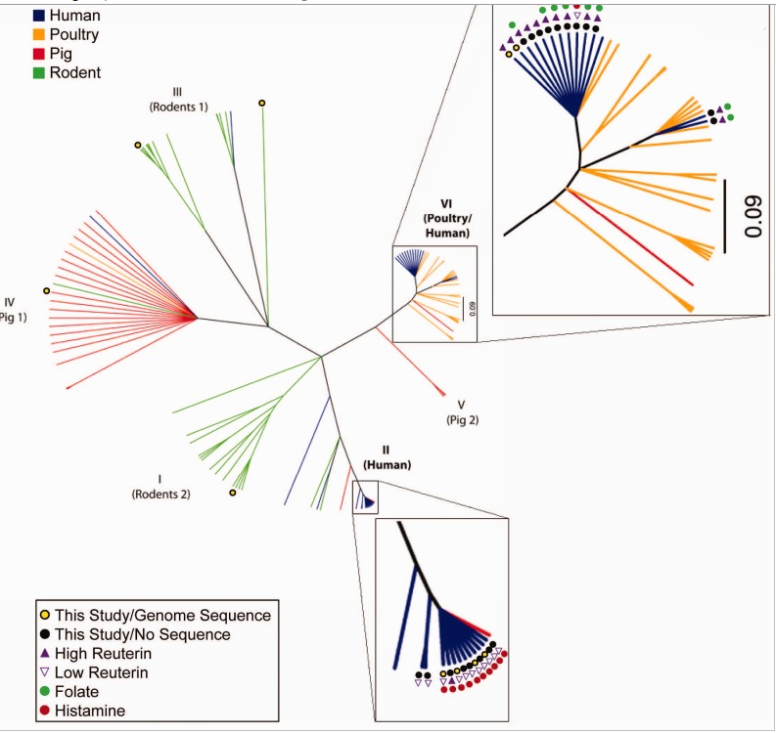
- Lactobacillus reuteri
- Lactobacillus rhamnosus GG & GR-1
- Mutaflor (Escherichia coli strain Nissle 1917)
Caution should be taken because one strain may produce histamine and another reduces it. The chart below show different strain of Lactobacillus reuteri. Some produces histamine and others do not. Bifidobacterium are in general safe. Lactobacillus has risks — if you try them, do one at a time when you are stable. Remember most probiotics are sold by Species and not Strain; same species from two different manufacturers may be different strains — so how lucky do you feel.
Your level of Histamine Producers in your Gut
This is now on Microbiome Prescription and is based on the count of species known to produce histamine in your sample.
Histamine N-methyltransferase
A reader asked about this item that I missed.
Histamine N-methyltransferase (HNMT) is an enzyme that plays a crucial role in the inactivation of histamine in central nervous system, kidneys and bronchi. Inhibition of HNMT is known to have a potential role in treating attention-deficit hyperactivity disorder, memory impairment, mental illness and neurodegenerative illnesses.
Molecular docking studies of Nigella sativa L and Curcuma xanthorrhiza Roxb secondary metabolites against histamine N-methyltransferase with their ADMET prediction [2021]
Genetic polymorphisms in histamine-related genes, including FcεRI and HNMT, were suggested to be involved in mast cell activation and histamine metabolism. Several genetic polymorphisms of leukotriene-related genes, such as ALOX5, LTC4S, and the PGE2 receptor gene PTGER4, were suggested to be involved in leukotriene overproduction, a pathogenic mechanism.
Molecular genetic mechanisms of chronic urticaria [2013]
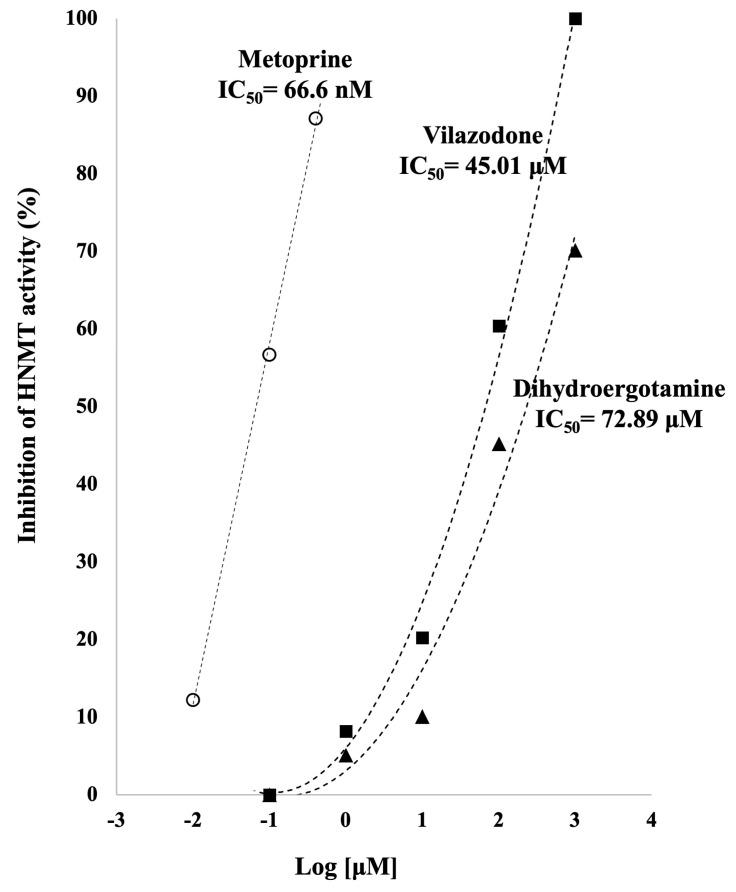
From Drug Repurposing to Inhibit Histamine N-Methyl Transferase[2023] we have this chart suggesting that Metoprine is the best performing of the drugs tested.
There is a sparseness of explicit studies, but it may be worth discussing with your MD who is better able to evaluate the literature.
Recent Comments