This person gave an extensive history – the microbiome reflects recent events in general so I have skipped most of it because of that.
An analogy may help, bacteria can be viewed as a city, say London or New York. An “event” happens, for example the Irish Potato Famine, or a shortage of labor causing the import of people from the colonies. The culture of the city is challenged. People are displaced and will often push back; fight back. Eventually a new status quo is established — it does not happen overnight, but over years; over decades. Returning to the old ways (London full of Saxons; New York full of tribal Indians) may be dreamt of, but never happens. An infection is a new wave of immigrants into the city. The impact does not always reflect the numbers. A small number of drug traffickers can have a huge impact on a city. This is how I think about the microbiome — a dynamic living city of bacteria that keeps changes over time. Ghettos develop where once stately manors of well-to-do people were.
Recent Back Story
In September of 2022, I had a COVID infection and fever, which caused a significant “crash”. I have been mainly bedridden ever since. Though the severity of symptoms I experience has waxed and waned from then until now, there has not been any significant differences in ability since. My symptoms are varied, and I’ve noted the ones experienced the week I took my sample on Microbiome Prescription. Positively, I have recently experienced a lowering of resting heart rate with regular electrolyte consumption, HR based pacing, NSDR, and diaphragmatic breathing. Starting Low Dose Naltrexone has helped with pain management, and I’ve needed to take less naproxen as a result.
I’ve tried oxaloacetate and pregabalin to no effect, had some significant side effects with duloxetine, and had a severe reaction with no benefits when I tried CBD/THC oil.
An interesting point is that my microbiome seems more similar to those Covid19 “Longhaulers” than to those with ME/CFS. I wonder why that may be, given that I had ME/CFS before my Covid infection?
I view both Long COVID and ME/CFS to be the same condition with one key difference. Long COVID is a recent major disruption of the microbiome. ME/CFS is often an ancient disruption that has evolved into a more stable state. Long COVID is typically an unstable microbiome that has a high rate of change. See this post on ME/CFS outbreak traced to a specific community infection. Some microbiome return to a stable normal state over time (a.k.a. remission). Going back to the cities examples above, Long COVID is akin to the mass migration of African Americans to Chicago after the civil war. ME/CFS is the state of Chicago today.
This person’s back history included:
- “Chronically anxious child with perfectionism tendencies” this pattern has been associated with ME/CFS by many. In terms of the microbiome, the stress would have significant impact on the microbiome.
- “Asthma” which has known microbiome shifts
- Severe constipation that required hospitalization, again know microbiome shifts. She has taken Polyethylene Glycol regularly. This is known to cause microbiome shifts.
- Taking fludrocortisone (fludrocortisone) and duloxetine for several years.
- Crohn’s disease, though the biopsies from the digestive tract were inconclusive. Again known microbiome shifts.
What does this mean? There is a massive amount of “microbiome noise” from these medical conditions and significant drugs. This could be classified as a hodge-podge of a microbiome.
Other questions I have regarding my sample:
Based on my sample, is it possible to tell the likelihood I have (or eliminate the possibility I have)…
- poor gut motility
- MCAS/Histamine issues
- Specific intolerances such as gluten or dairy
- SIBO
- Leaky Gut
- Celiac
Basically, can I extrapolate from the data if I may have issues to fix regarding one of the above or if I can say with some certainty that these don’t affect my gut health?
No, it is not really possible to tell the likelihood. The best that you can do is whether you have bacteria associated with those conditions. Association main purpose is to augment or suggest additional medical tests. Some examples:
- Special Studies:
- 12 % match Poor gut motility (your highest was 30% for Long COVID)
- 13 % match Allergies And Food Sensitivity
- 10 % match MCAS/Histamines
- 8 % match Small intestinal bacterial overgrowth (SIBO)
- Pub Med:
The PubMed one that you are highest in is Colorectal Cancer (with 9 of 38 matches). This some some resemblance to her recent medical history.
Around August 2020, I started experiencing rectal bleeding, abdominal cramping, mouth sores, and rectal prolapse. I had a colonoscopy and endoscopy in Dec. 2020 with general anaesthetic, and it was as if I had been “hit by a truck”. I could barely get out of bed for the next 5 months. I was diagnosed with Crohn’s disease, though the biopsies from my digestive tract were inconclusive…. Some other anomalies found include a potential cyst on my right ovary and a tender and enlarged lymph node near my right armpit. The cyst and fluid sac may just be “the more you look, the more you find”.
I seem to be intolerant to (or not digest very well) dairy products (with or without lactose), processed foods, acidic fruits (such as raspberries, oranges, lemon or pineapple), starchier foods, oils and fats, lentils, onion, garlic, asparagus, almonds, cucumbers, broccoli, tomatoes, chai, rice crackers, etc. With some foods, such as gluten or eggs, it seems to vary as to whether I tolerate it well.
My medications at the time of the sample were:
- Low Dose Naltrexone 3mg
- Nadolol 40mg
- Multivitamin
- Vitamin D 2000iu
- Vitamin C 500g
- Naproxen as needed for menstrual and joint pain
Since then, I’ve added these supplements:
- Magnesium Glycinate 90mg TID (total 270mg)
- Inulin 1tsp
- Align Probiotic 1 capsule
- Probiotic 3 1 capsule TID (total 3 capsules)
- Tributyrin-x 3 capsules
- D-Ribose 5mg
Analysis
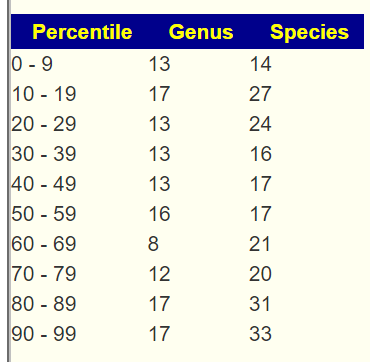
Unlike most Long COVID and ME/CFS microbiomes, the percentage in each percentile is well balanced in the percentages in each percentile. This may be due to items like Low Dose Naltrexone and other medication, or her complex medical history. In terms of Shannon Diversity Index, it was high 2.07 / 97.1%ile.
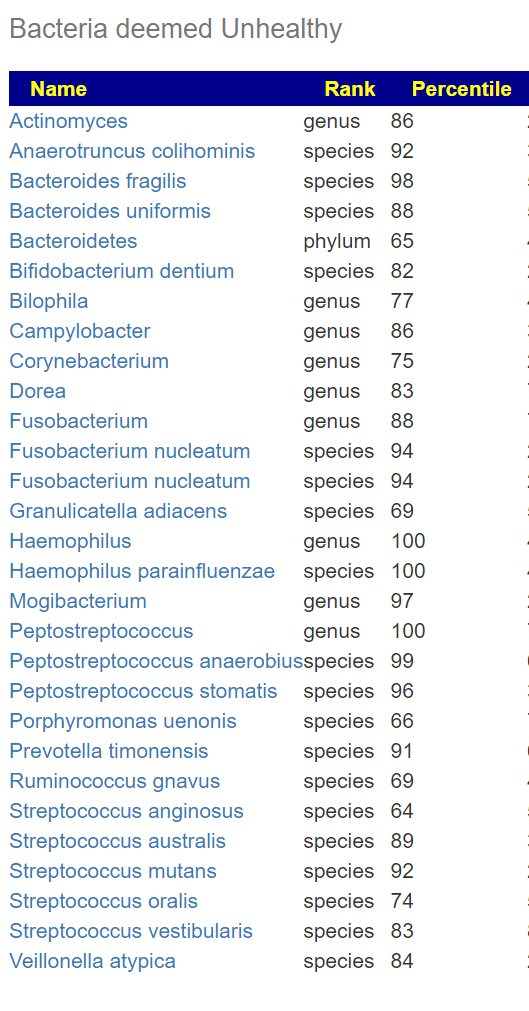
Switching over to Bacteria Deemed Unhealthy, we see a very long list. Some of these are associated with MCAS and allergies. This is a much better signature than the above ones.
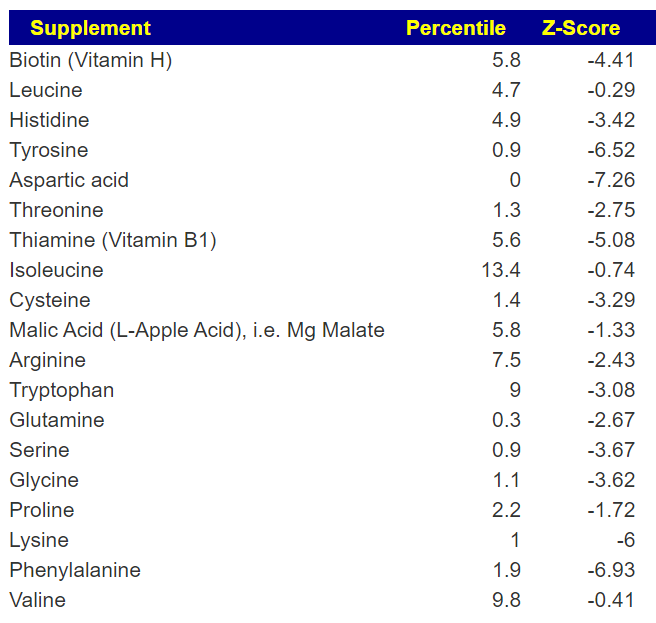
Going over to KEGG AI Computed Supplements, we see a long list, much longer than typical. Items over a Z-Score of 2 are strong candidates for taking as supplements. These are chemicals consumed by bacteria or the body and thus suggests starvation of bacteria (with misbehavior likely).
Looking at AI computer probiotics, nothing stood out strongly. Enterogermina (Bacillus Clausii) is the strongest suggestion.
Analysis of What Is Currently Being Taken
The following times were listed above, I did the “just give me suggestions” and the looked at the full detail via the consensus report. Usually the consensus report highest value is around 400; her report went up to 753 and down to -1064. This is far more variation than I usually see!
- Low Dose Naltrexone 3mg – GOOD, 496.4 (max was 753.
- Nadolol 40mg – GOOD, 496.4
- Multivitamin
- Vitamin D 2000iu – so so, -15
- Vitamin C 500g – positive: 400
- Naproxen as needed for menstrual and joint pain — Good 496.4
- Magnesium Glycinate 90mg TID (total 270mg) – negative -355
- Inulin 1tsp – BAD, -732.4
- Align Probiotic 1 capsule – bacillus coagulans – so so, -14
- AOR Probiotic 3 – 1 capsule TID (total 3 capsules)
- Enterococcus Faecium – so so (-22, -172), to negative
- Clostridium Butyricum – negative – 306
- Bacillus Subtilis – so so (-19,-48, -315) to negative
- Tributyrin-x 3 capsules – so so -12
- D-Ribose 5mg – negative -200
Remember: these are fuzzy logic computation based on fragmentary data available from existing studies. In general, readers have reported improvement from the suggestions – but the suggestions are plotting courses in a fog bank… so do not become dogmatic about doing or not doing.
So what is suggested instead?
Well, all of the prescription items above are big thumbs up! 🙂
- Probiotics:
- 481 – lactobacillus kefiri (NOT KEFIR) – available only in Italy 🙁
- 345 – bifidobacterium breve (probiotic)
- 496 – Acetaminophen, Paracetamol in UK one with each meal for a week and then one a day? Discuss with your MD. The purpose is altering the microbiome, not headache (i.e. off label use)
- Supplements
- 463 – melatonin supplement
- High dosage of B-Complex or individually:
- 336 – Taxifolin
- 640 – Hesperidin (polyphenol) a.k.a. Grapefruit. If you cannot tolerate Grapefruit, then try the supplement only.
- 496 – Arbutin (polyphenol)
- 496 – Diosmin,(polyphenol)
- 472 – luteolin (flavonoid)
- 594 – Caffeine (Coffee or Tea)
- 437 – lauric acid(fatty acid in coconut oil,in palm kernel oil,) A.K.A. Monolaurin
- 652 – thyme (thymol, thyme oil)
- 596 – garlic (allium sativum)
- 540 – peppermint (spice, oil) there are a lot more herbs and spices that are over 300
- 433 – mastic gum (prebiotic) – most prebiotics are negative
- 584 – sucralose – most other sugars are low or negative value
Questions and Answers
Q: It seems that my microbiome is very well balanced, but has many unhealthy bacteria and a much more varied consensus report than usual. With other similar results from others, do you see a common reason or cause for this being the case?
- A: I would not call it well balanced. Several measuring sticks show no strong pattern, but given the large number of microbiome affecting things that have happened to you, those events have likely added a lot of noise. The abnormally large number of bacteria deemed unhealthy is the signature thru this noise. This is not a common situation. Most people have just one microbiome affecting thing.
Q: Being in the 0% percentile for POTS seems interesting for me, given that my POTS is still not quite stable. What are the usual reasons for a microbiome not matching the symptoms and diagnosis of a particular condition (especially that I’m only a 12% match for MECFS with/out IBS)?
- A: Similar to above, compounding conditions and treatments that alters the microbiome is a multitude of ways. Ideally, we want to see patterns but patterns usually arise from “pure cases”, you are not a pure case, but a highly compounded case.
Q: Given I have the highest association to Colorectal Cancer, how important is this? Is this something I should be looking to screen for or is it of low enough significance to ignore somewhat?
- A: In the abundance of caution, I would ask for screening, you have one recognized risk factor with a hint also from your microbiome. Per CDC guidelines (helps persuade MDs) “However, you may need to be tested earlier than 45, or more often than other people, if you have— Inflammatory bowel disease such as Crohn’s disease or ulcerative colitis.” [CDC]
Q. I’m currently taking magnesium mainly as a tool to manage muscle spasms and twitches. Is there a supplement with similar effects that has a better consensus value?
- A: What I did was search the US National Library of Medicine for possible alternatives.
- Lactobacillus paracasei is cited [2004] “Lactobacillus paracasei, but not Lactobacillus johnsonii, Bifidobacterium lactis, or Bifidobacterium longum, attenuated muscle hypercontractility.”
Unfortunately a negative.
- Streptococcus thermophilus and Lactococcus lactis [2022] “Spasm reductions were accompanied by specific gut microbial alterations, including increases in Streptococcus thermophilus and Lactococcus lactis. Mimicking the fecal microbial alterations in a targeted probiotic, we administered these species in a 5:1 ratio. Targeted probiotic administration reduced seizures and improved locomotor activities in control diet-fed animal”
– No information, so these two would be my first preference. - From other articles, there appear to be associations of spasm and twitches with mineral imbalances. For example, hypokalemia(low potassium) [2023]
– I would suggest explicit testing for mineral balances
- Lactobacillus paracasei is cited [2004] “Lactobacillus paracasei, but not Lactobacillus johnsonii, Bifidobacterium lactis, or Bifidobacterium longum, attenuated muscle hypercontractility.”
If you have a willing MD, I would ask for amoxicillin which is a common antibiotics and has the second highest confidence of having an impact. The top one, Imipenem, is an intravenous β-lactam antibiotic and it’s impact on the microbiome is less certain. Remember, most MDs will only prescribe for acute active infection and a microbiome dysfunction/issues may not be sufficient for them.
My next choice would be thyme oil and hesperidin supplements. With the thyme oil — definitely start with a low dosage and expect bacteria to be protesting strongly (often they protest by massive dumping of toxins into the body… they do not go out quietly).
If you try these suggestions and notice changes, I would suggest another test in 8-10 weeks to see what changed and what your next course correction will be.
Postscript – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I cannot tell people what they should take or not take. I can inform people items that have better odds of improving their microbiome as a results on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting.
The answers above describe my logic and thinking and is not intended to give advice to this person or any one. Always review with your knowledgeable medical professional.
Recent Comments