Backstory
I think my case is unique and interesting. I have had CFS/ME for 37 years since age 15, but I have been very functional for the most part. I had been worsening over the past 8-10 years and discovered high mold levels 3 years ago in my house. I developed MCAS and related symptoms from the mold. But with treatment I was improving ( See Pre-COVID Thryve sample which is quite good.)
Then contracted COVID in Nov 2021. I had a moderately severe acute COVID illness and did not recover fully, developed Long COVID. Shortness of breath, low o2 sat, palpitations, dysautonomia, insomnia, irritable bladder, cognitive issues much worse than CFS/ME. My GI issues were not too bad though. Diarrhea on and off for several weeks. Gas and bloating that aligned with my MCAS fluctuations. I did have a GI Effects test done during this time (Feb 2022) and it wasn’t too bad (5 score on dysbiosis 0 or 1 on other markers, 2 on inflammation. I know the limitations of that test.
My health steadily improved and as of 2 months ago I was 85% from my pre-COVID health. But contracted respiratory illness, most likely COVID again. Sore throat, congestion, GI issues. Took 3 weeks to resolve sore throat and congestion but GI issues have worsened over the last 5 weeks. Alternate between diarrhea and constipation, gas, cramping, MCAS worse. Passed out earlier this week when experiencing cramping. Had strange derealization experience at that time, kind of like a flashback or deja vu. Fatigue and cognitive issues are getting worse as well.
Analysis
My tell-tale test for ME/CFS and Long COVID is massive over-representation of the 0-9%ile. The number in each percentile range should be around the same in a normal microbiome. These are often different from patient to patient. For other ME/CFS or Long COVID analysis, see this page.
| Percentile | Genus | Species |
|---|---|---|
| 0 – 9 | 51 | 72 |
| 10 – 19 | 12 | 18 |
| 20 – 29 | 18 | 18 |
| 30 – 39 | 14 | 18 |
| 40 – 49 | 16 | 20 |
| 50 – 59 | 19 | 20 |
| 60 – 69 | 13 | 19 |
| 70 – 79 | 26 | 18 |
| 80 – 89 | 17 | 18 |
| 90 – 99 | 17 | 22 |
Looking at Dr. Jason Hawrelak Recommendations, we see a lot of items out of position.
| Taxonomy | Rank | Low | High | Your Value | Status | Hand Pick |
|---|---|---|---|---|---|---|
| Bacteroidia | class | 0 | 35 | 37.085 | Not Ideal | |
| Akkermansia | genus | 1 | 3 | 0.354 | Not Ideal | |
| Bacteroides | genus | 0 | 20 | 31.372 | Not Ideal | |
| Bifidobacterium | genus | 2.5 | 5 | 0.005 | Not Ideal | |
| Blautia | genus | 5 | 10 | 11.271 | Not Ideal | |
| Desulfovibrio | genus | 0 | 0.25 | 0.028 | Ideal | |
| Eubacterium | genus | 0 | 15 | 0.177 | Ideal | |
| Lactobacillus | genus | 0.01 | 1 | 0.006 | Not Ideal | |
| Methanobrevibacter | genus | 0.0001 | 0.02 | 0 | Not Ideal | |
| Roseburia | genus | 5 | 10 | 0.472 | Not Ideal | |
| Ruminococcus | genus | 0 | 15 | 5.567 | Ideal | |
| Proteobacteria | phylum | 0 | 4 | 8.94 | Not Ideal | |
| Bilophila wadsworthia | species | 0 | 0.25 | 0.093 | Ideal | |
| Escherichia coli | species | 0 | 0.01 | 0 | Ideal | |
| Faecalibacterium prausnitzii | species | 10 | 15 | 2.902 | Not Ideal | |
| Overall Percentile Ranking | 56.5% | |||||
One item to note is Bifidobacterium which appears to be associated to allergies and potentially MCS (see Mast Cells and Bifidobacteria)
The Bacteria deemed Unhealthy list had some interesting items:
- Rickettsia at 99%ile and Ehrlichia at 96%ile — this genus was the focus of Dr. Cecile Jadin work with ME/CFS over the last 3 decades. I recently did another post on these High Tick-borne Bacteria Counts (P.S. Dr. Jadin is working on a draft of her current protocol for this site — stay tune)
- Faecalibacterium prausnitzii species at 17%ile, Reduced Ability to handle inflammation
As with another person who had ME/CFS and then Long COVID, let us look at the matches to published literature:
- Long COVID (62 %ile) 14 of 204
- COVID-19 (59 %ile) 11 of 118
- Chronic Fatigue Syndrome (60 %ile) 4 of 64
- Irritable Bowel Syndrome (80 %ile) 10 of 68
- Allergic Rhinitis (Hay Fever) (98 %ile) 6 of 39
Other matches were interesting, Insomnia (0 %ile) 0 of 26, which implies that sleep issues are likely atypical. These are very rough estimates (the studies were done with different lab processes, so the data is fuzzy).
Going Forward
I started with the “Just give me Suggestions” and then manually did the 5 items above. Why? To give emphasis to the likely bacteria that may be of main concerns. So we see:
The highest (and lowest) priority were 466 and -453. So our emphasis would be items over 233 and below 227 to give us the best odds. Yes, odds — everything is done by fuzzy logic and probability.
The top easy to do items are:
- bacillus subtilis (probiotics)
- high fiber diet
- Cacao
- green tea
- walnuts
- Nicotine (not smoking, but a nicotine patch — I got an email from a user that had a major recovery using it)
- rifaximin (antibiotic)s — which is often used by ME/CFS specialists [Src] and Rifaximin and CFS and often for Irritable Bowel Syndrome (297 citations on PubMed). My suggestion is to read up on how MDs diagnosis IBS and emphasis those symptoms. Then suggest this antibiotic (if the MD does not). My experience is that you want to craft your meeting with MD, so they will go where you want to go. Do not just do verbal diarrhea of symptoms, you will randomize (and perhaps frustrate) the MD. When you want the MD to go down a particular path, tune your story to their thinking.
- Other probiotics:
Flipping over to the other side, items to reduce or avoid if possible:
I have often suggested barley or oats porridge with walnuts for breakfast each day — that provides lots of fiber. As for milk with it– Yakult — which contains lactobacillus casei (probiotics). And cacoa / chocolate — see Honestly! Chocolate!!! [2012], Bifidobacterium, Chocolate and CFS [2014] and Chocolate & Blueberries– Good Medicine for Bifidobacteria [2017]. All of the following are positives: blueberry, whole-grain barley, oats and barley,oat.
Going over to Retail probiotics, see several safe(no adverse impact detected) one including: symbiopharm / symbioflo 2, enterogermina and Filmjölk (SE) / Filmjölk (hard to get outside of Sweden).
Flipping over to Food Menu Planner we see a short list of high priority items. The top one: inulin and fiber cited above are a convergence… but what about the other oddities?
| 👍 | 100 | Inulin |
| 👍 | 61.11 | 1,4-Naphtoquinone — in Walnuts Liquor |
| 👍 | 53.01 | Isoferulic acid — vinegar |
| 👍 | 43.39 | Raffinose — in Artichoke, jerusalem, peeled, boiled, drained (which is also used for inulin) |
| 👍 | 34.13 | 02 mers — Chocolate, dark |
| 👍 | 31.71 | Oligosaccharides — Pea, split, dried (or supplements) |
| 👍 | 31.25 | Naringin — Grapefruit |
| 👍 | 30.22 | Apigenin 7-O-glucuronide — Globe artichoke, heads, raw |
As a reminder, many studies use the above nutrients (and the food it comes from may not have been studied). The Food Menu attempt to resolve this disconnect. So Artichokes of different types should be regularly on your supper menu — perhaps with pea soup or just boiled peas.
Questions
My current diet (low carb, higher saturated fat, high red meat) is a poor choice according to these results. The low carb approach works well for my blood sugar and for keeping my weight down, but I do crave good carbs. I eat a lot of vegetables but it is impossible to get enough fiber that way. I had been supplementing with a rotation of psyllium, flax and chia. I will slowly adjust my diet to a higher carb, lower fat one and see how I respond. I have done well with oats in the past. I think as long as I combine the starches with lean protein I will do fine.
I used inulin during my first Covid infection and seemed to do well with it.
With regard to probiotics, bacillus subtilis looks to be a great choice, but different strains are used in the studies and most are not available commercially. The one commercially available microbiome labs /hu58 is marginally “likely safe”.
I am going to try Yakult. What would be your second choice?
Nicotine is interesting. This was talked about early on as being protected for Covid. Now it is gaining popularity as many are trying for Long Covid.
It is disappointing there are no strong consensus herbs or spices.
Feedback.
A: Concerning Probiotics, there is a second approach — looking at the genes you have in your bacteria and what they are not producing enough of.
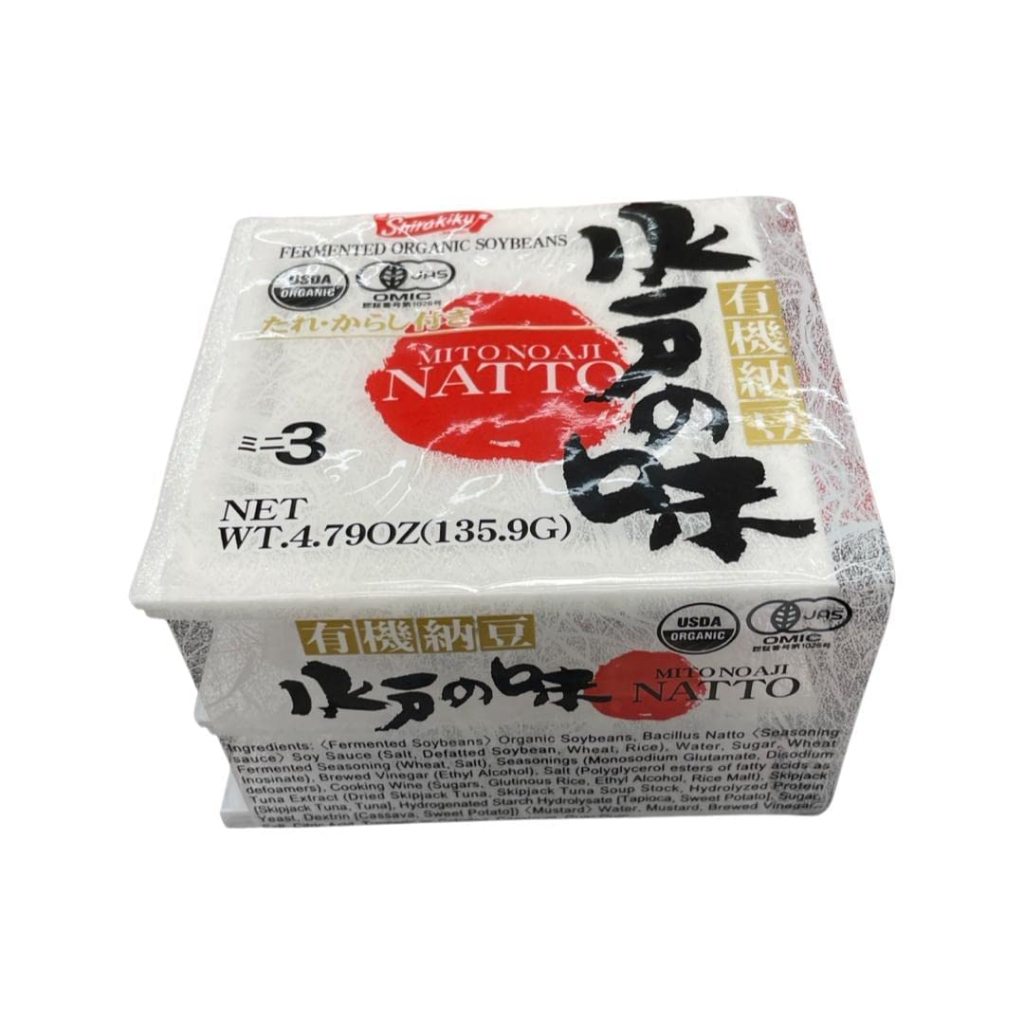
The top 1 is Escherichia coli — available in two products: Mutaflor and Symbioflor-2. The next ones that are relatively easy to obtain are Bacillus subtilis and a specific species: Bacillus subtilis subsp. natto. This later item is available in many Japanese food sections of some grocery stores. It is just called Natto. It is made using soy which is also on your positive list. It also is a fibrinolytic (unthickens thick blood).
Q: “Should I consider rosemary stronger because of ursolic acid?”
A: No, the numbers indicated confidence of the item having a positive or negative effect. They are not “better” or “stronger” numbers, just more likely to have some effect (may be minor). We are using fuzzy logic, hence odds and the odds are on causing shifts and NOT the amount of shift. That is all that we can get from the studies usually.
Bacillus subtilis subsp. natto
Bottom Line
This microbiome matches the pattern for ME/CFS and Long COVID. Most of the suggests have been studied with ME/CFS with positive results. Now it is just a matter of doing. After 6-10 weeks do another microbiome sample so you may make the next course adjustment. Most people cascade into ME/CFS, getting out is a dog-legged journey.
Addendum Exploration
I decided to look how the indices change with age. As you can see below, in general they decrease or increase significantly with age as I would expect. For more information see this earlier post.
.
| Symptom Name | Shannon | Simpson | Chao | Shannon Rank | Simpson Rank | Chao Rank | Obs |
| Age: 0-10 | 1.576 | 0.118 | 8788 | 33.1 | 65.2 | 44.8 | 21 |
| Age: 20-30 | 1.599 | 0.065 | 11592 | 32.2 | 49.7 | 52.6 | 57 |
| Age: 30-40 | 1.579 | 0.06 | 11119 | 31.9 | 43.5 | 52.9 | 153 |
| Age: 40-50 | 1.62 | 0.067 | 10433 | 34.8 | 47.1 | 50.5 | 106 |
| Age: 50-60 | 1.605 | 0.045 | 11728 | 32.8 | 34.1 | 55.3 | 47 |
| Age: 60-70 | 1.488 | 0.033 | 13580 | 28 | 26 | 60.7 | 22 |
Alpha Diversity Indices:
For a general introduction.. Personally, they are unlikely to be useful in an individual context and are complex to fully understand. I include this as an exploration
- Shannon Diversity Index: 1.39 / 16.3%ile
- Closest to: Comorbid: Salicylate sensitive;Other: Sensitivity to vibrations;Neurological-Vision: Blurred Vision;DePaul University Fatigue Questionnaire : Tingling feeling;DePaul University Fatigue Questionnaire : Blurred Vision;Immune Manifestations: Thick blood / Hypercoagulation
- Simpson Diversity Index: 0.04 / 31.2%ile
- Closest to: Age: 60-70; Neurological: fasciculations; Other: Sensitivity to vibrations
- Chao1 Index :16371 / 76.6%ile
- Closest to: DePaul University Fatigue Questionnaire : Does physical activity make you feel better; Age: 60-70; Comorbid: Restless Leg; Onset: less than 08 years since onset; DePaul University Fatigue Questionnaire : Chemical sensitivity
Recent Comments