Allergies are often tossed into a big box of “all allergies are the same”. I have learnt from studies that often different items are clustered together to avoid needing to learn and detail with the details. I know people that have very specific allergies — i.e. to birch but not grass or other tree pollens. Most MDs will toss such people in the seasonal allergic rhinitis bucket; treating them proforma.
This appears borne out by some studies:
- ” A delayed correlation between the birch pollen concentration and the symptom scores was seen up to two days after the pollen measurement. For grass pollen this effect lasted up to three days after the pollen measurement.”[2023]
- “the most effective treatments for allergic rhinitis were in order as follows: sublingual immunotherapy_dust mite, subcutaneous immunotherapy_dust mite, sublingual immunotherapy_ grass mix plus pollen extract, placebo, and pharmacotherapy. ” [2023] – note that placebo was more effective that traditional medicine!
The goal of this exercise is see if there are any new options or approaches for addressing this issue.
Environment May Be a Factor
Some of my university professors refused to believe that allergic rhinitis existed. They were born and raised in a part of the middle east and never encountered people with it before moving to North America. This saying from the prophet recorded by Salamah b. al-Akwa, implies that allergies may have been unknown in that part of the world:
“When a man sneezed beside the prophet (May peace be upon him), he said to him : Allah have mercy on you, but when he sneezed again, he said : The man has a cold in the head.“
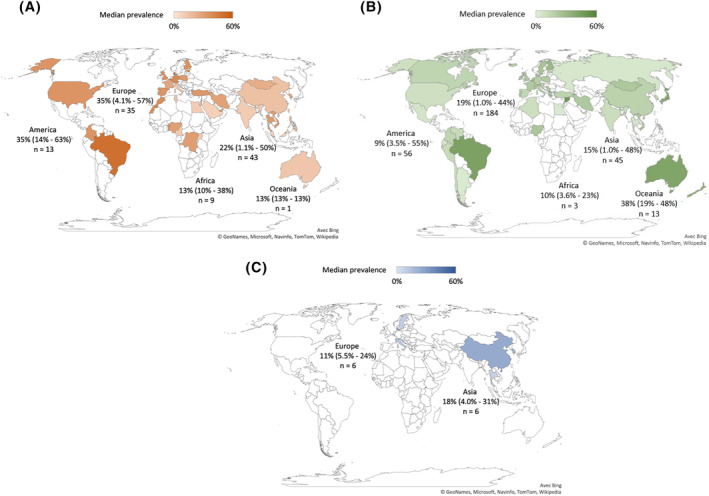
This seen in the following charts: (A) Unspecified rhinitis; (B) allergic rhinitis; (C) non‐allergic rhinitis.
- “A family history of allergic rhinitis, asthma, or atopic dermatitis increases a patient’s risk of being diagnosed with allergic rhinitis. People in the United States are commonly sensitized to grass, dust mites, and ragweed allergens.” [2023]
- “Asthmatic patients from Madrid(urban) have a worse clinical evolution than those from Ciudad Real (rural)because of higher levels of urban pollution,” Clinical impact and immunological alterations in asthmatic patients allergic to grass pollen subjected to high urban pollution in Madrid [2022]
- “Subjects with persistent rhinitis and asthma had higher levels of total IgE at baseline and after 10 years, and exhaled nitric oxide and eosinophil cationic protein at baseline compared with those that remained healthy. ” [2023]
- Exhaled nitric oxide implies a breath test and thus we have 1135 bacteria the produces this chemical, hence a potential overgrowth as a contributing factor.
- Eosinophil cationic protein in also in the gastro-intestinal tract[2011]
Treatment Trends
Things here gets a little complex…
B cells are key players in the mechanisms underlying allergic sensitization, allergic reactions, and tolerance to allergens. Allergen-specific immune responses are initiated when peptide:MHCII complexes on dendritic cells are recognized by antigen-specific receptors on T cells followed by interactions between costimulatory molecules on the surfaces of B and T cells. In the presence of IL-4, such T-B cell interactions result in clonal expansion and isotype class-switching to IgE in B cells, which will further differentiate into either memory B cells or PCs. Allergic reactions are then triggered upon cross-linking of IgE-FcɛRI complexes on basophils and mast cells, leading to cell degranulation and the release of pro-inflammatory mediators.Mechanisms underlying effective allergen-specific immunotherapy (AIT) involve the induction of Tregs and the secretion of blocking IgG4 antibodies, which together mediate the onset and maintenance of immune tolerance towards non-hazardous environmental antigens.
B Cell Functions in the Development of Type I Allergy and Induction of Immune Tolerance [2022]
- Oralair, a biologic, has grown in use in Europe (approved in 2008 from 8% to 29% by 2012 [2015]) and is approved in the USA (2013) Link to FDA documents. It is prescription with a base cost of $5 or more per tablet — hence, antihistamines are more likely to be recommended in the US due to cost, not effectivity.
- Similar items are also available, (2800 BAU grass SLIT-T) [Relative to placebo, grass AIT treatment improved total combined scores by 20% 2011], Grazax [The active group demonstrated a 31% reduction in median rhinoconjunctivitis symptom [2011]], MK-7243. There are not cures, rather reduces severity for a percentage of people.
“The only treatment available to treat grass allergy is immunotherapy treatment. This is when you are exposed to small but increasing doses of allergens over a long period of time to help stop your allergic reaction. It takes a long time to work and needs to be prescribed by an allergy specialist.” Australian Department of Health
Treatment via Microbiome
For grass allergy we have the following available retail with studies which boils down to 2 probiotic species worth considering.
| Lactobacillus casei Shirota | Yakult | Oral delivery of Lactobacillus casei Shirota modifies allergen-induced immune responses in allergic rhinitis. [“ Volunteers treated with LcS showed a significant reduction in levels of antigen-induced IL-5, IL-6 and IFN-gamma production compared with volunteers supplemented with placebo. Meanwhile, levels of specific IgG increased and IgE decreased in the probiotic group.”] |
| Lactobacillus rhamnosus GG | Culturelle® | Effect of Lactobacillus rhamnosus GG and vitamin D supplementation on the immunologic effectiveness of grass-specific sublingual immunotherapy in children with allergy. [“Reduction in the symptom-medication score and improvement in lung function as well as a significant increase in the percentage of ….in all the groups were observed compared with control group”] |
| Lactobacillus rhamnosus GR-1 | RepHresh™ Pro-B™ Probiotic | Development and pilot evaluation of a novel probiotic mixture for the management of seasonal allergic rhinitis. [“provided few clinical benefits.”] |
| Mutaflor (Escherichia coli strain Nissle 1917) | Mutaflor (Canada, Australia, Findland, Germany) | Tolerability and clinical outcome of coseasonal treatment with Escherichia coli strain Nissle 1917 in grass pollen-allergic subjects. [“not sufficient to achieve clinical efficacy in grass pollen”] |
Non-Strain probiotic candidates:
- Bifidobacterium longum [2023], lowers IgE (see below)
- Lacticaseibacillus paracasei [2023] ” 2 billion CFU/day for 3 months ameliorated sneezing”
And this delightful title “Role of Probiotics in Patients with Allergic Rhinitis: A Systematic Review of Systematic Reviews” [2022] found no hard evidence for any specific probiotics.
Bottom Line for Probiotics: It seems that they need to be taken well in advance of allergy season with sufficiently large dosages.
Explorations
I took the list of 1135 bacteria that produces nitric oxide and then looked at the 40 bacteria reported on National Library of Medicine Citations for Allergic Rhinitis (Hay Fever). I was disappointed not to find many matches. What I found were matches for:
- Bacteroides (NCBI:816 )
- Clostridium (NCBI:1485 )
- Acidaminococcus intestini (NCBI:187327 )
Next, I went to samples that are annotated with Official Diagnosis: Allergic Rhinitis (Hay Fever) – about 200 samples, and then cross apply them to the above 1135 bacteria. There are no strong statistical significance found.
| Tax_name | Average | Samples |
| Haemophilus parainfluenzae | 56.1 | 41 |
| Tax_name | Average | Samples |
| Pelosinus fermentans | 60.1 | 22 |
| Limosilactobacillus fermentum a.k.a. Lactobacillus fermentum | 57.7 | 34 |
| Veillonella atypica | 52.9 | 22 |
| Veillonella dispar | 52.7 | 49 |
How to do this experiment
- Go to your samples
- Look at Microbiome Tree
- Search for the items above
- Hand pick (if you have any matches)
This exploration failed to produce any significant finding or insights. 🙁
Exploring Immunoglobulin (IgE etc)
As a starting point, Immediate Hypersensitivity Reactions [2023] is of special interest for those who have reactions within 24 hours. “Antibodies including IgE, IgM, and IgG mediate them… Allergic rhinitis is another atopic disease where histamine and leukotrienes are responsible for rhinorrhea, sneezing, and nasal obstruction. ” Typically only IgE is involved. IgE increase in response to grass pollen exposure and are responsible for the allergic symptoms.
- “Patients with pollen allergy but not control donors have a population of circulating allergen-specific B cells with the phenotype and functional properties of adaptive memory B-cell responses. These cells could provide precursors for allergen-specific IgE production upon allergen re-exposure.” [2015] – which implies repeat exposure may increase severity.
- Omalizumab: reduced significant clinical exacerbation within 24 weeks [2023]
FYI On Other Allergies
Mast Cells Issues can be moderated by some Bifidobacterium bacteria (Click for studies).
Bottom Line
Symptom relief via antihistamines or DAO for a subset for immediate response, or months of preparation for allergy season by probiotics and biologics.
DAO levels were lower in AR patients compared with the controls. The DAO level did not significantly correlate with the severity of AR according to the Allergic Rhinitis and its Impact on Asthma (ARIA) score, though it was lower in patients with persistent or moderate to severe symptoms. The total IgE, eosinophil percentage, and SNOT-22 score all had an inverse relationship with DAO.
Predictive Value of the Serum Diamine Oxidase Level in the Diagnosis of Seasonal Allergic Rhinitis [2022]”
Avoidance of Grass Pollen
This is really what the Asthma and Allergy Foundation of America strongly advocates.
Above memory B-cell responses were cited in research which I translate that repeated exposure will make it worse, hence one approach is aggressive avoidance.
- Wearing a N95 or better mask when outside from the start of pollen season onwards. In some cases a full face mask may be better. When you arrive home, do a complete change of clothes as soon as possible (ideally outside) and take a shower.
- Aggressively reduce pollen in your living place (i.e. pollen leaking into the house via windows and open doors)
Our Approach
This household’s solution for grass allergy has been HEPA air filters oversized for the room size. For example, this $90 unit is rated for 183 sq ft. We would use it for 90 sq ft only — the size of a small bathroom (8′ x 10′). A 10x more expensive unit (Austin HEALTHMATE PLUS ) is rated for 1500 sq ft, so we will use it to cover only 750 sq feet. This means that a 2,000 sq ft house would need at least three operating. Note that this intentional oversizing is to reduce the time to remove grass pollen that comes in.
Time to Reduce Pollen from opening a door
The Austin does 400 cubic feet per minute and we can assume that for one complete room exchange that the pollen level will drop by 50%. It will not remove all in one room exchange. You remove 400 cf in a minute and shoves the clean air back into the room — diluting the air that is there. A little calculus finds that after one cycle, we are down 50% only.
Sample Calculation: 750 sq ft x 8 ft ceiling = 6000 cu feet … thus 15 minutes for one exchange with a 400 cfm unit (i.e. the Austin). If we go with manufacture specifications of 1500 sq feet, than 30 minutes to remove half of the pollen.
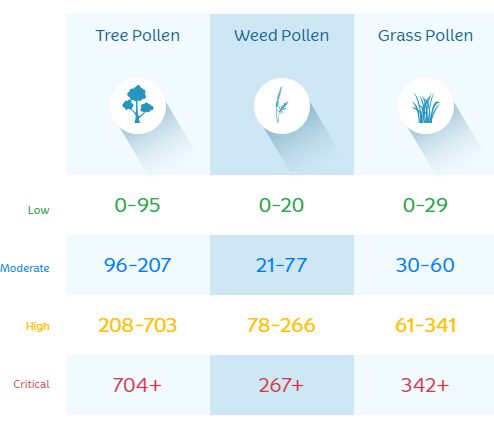
PPM, or pollen per cubic meter.
Consider a High Grass level at 340. After one room exchange, it would be 170 (still high), after two room exchanges it would be at 85 (still high), after three exchanges down to 43 – moderate, and at 4 exchanges we are at 20 — into the low range at last. In short, after opening a door for a short while, it may take 2 hours for the pollen level to get reduced to acceptable levels.
Conclusion: Keep the doors open for the least amount of time possible. Consider adding automatic door closers to all doors. Windows should not be open and they should be tight seals. A furnace that brings air in from the outside as part of normal operation should have HEPA filters installed on the intake.
We went one step further, we added to our house an air pump that takes air thru a HEPA filter and creates a positive air pressure in the house. This is one way to address leaky doors and windows — instead of pollen leaking in, the positive pressure pushes it away. We originally installed it to address wild fire smoke (works nicely), but this pollen season it has made a noticeable difference.

Recent Comments