Back Story
I have been suffering from fatigue for about 8 months now and would like your advice. I have seen multiple doctors now and they have not been able to figure anything out despite running multiple labs. My fatigue started around August of 2022 when I was put on antibiotics. I had an infected wound from a martial art that got infected. After that, I got c diff from a friend I had been taking care of, so in late August I was put on another course of antibiotics. Then in September I got c diff again and was put on another course of antibiotics. My fatigue became very severe at this point. I could barely make it out of bed, etc. I still have fatigue now. I can walk around but I get tired pretty easily. I still cannot go to the gym or exercise. Just the thought alone of pushing my body seems tiring. Please assist.
Antibiotics can be good or bad. Each type alters the microbiome in different manners. Recently I added a new tool to help people negotiate with their MD to find the best candidate antibiotics that will address the MDs concern while looking at their microbiome impact (which is not an area they are knowledgeable). See this video for more information. What has happened, happened — let us move forward.
The antibiotic given were:
- Cephalexin (Keflex, Daxbia) for the wound – which I lack any significant information on
- Dificid (A Macrolide, fidaxomicin) for c diff
Analysis
First, we see the type of distribution often seen with Chronic Fatigue Syndrome and Long COVID — two conditions with fatigue being a signature symptom. Many many token genus and species.
| Percentile | Genus | Species |
|---|---|---|
| 0 – 9 | 77 | 99 |
| 10 – 19 | 22 | 27 |
| 20 – 29 | 8 | 8 |
| 30 – 39 | 13 | 12 |
| 40 – 49 | 5 | 10 |
| 50 – 59 | 9 | 15 |
| 60 – 69 | 6 | 13 |
| 70 – 79 | 5 | 15 |
| 80 – 89 | 7 | 7 |
| 90 – 99 | 3 | 5 |
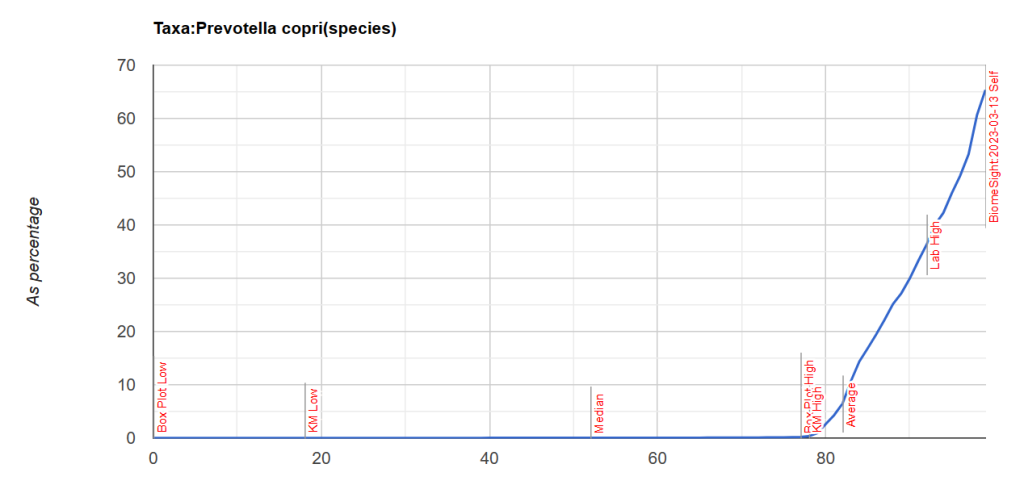
This tool also flags the bacteria that may be causing it. What was flagged is shown below — through the roof on these one bacteria (parent-child), This is known to be a very pro-inflammatory bacteria. It is 61% of the microbiome!! It is strongly associated with rheumatoid arthritis [2013] [2023] [2019]. High levels also may indicate mycotoxin (fungi) is present in the environment (house, places he goes) or person [Citation]. For more information see this excellent summary.
| Rank | Name | Your value | Percentile |
|---|---|---|---|
| genus | Prevotella | 618680 | 99 |
| species | Prevotella copri | 617760 | 100 |
The chart below shows how extreme it is.
Looking at Potential Medical Conditions Detected, we had 12 items – which is to be expected with this type of shifts, and we will ignore. It is interesting to note that Dr. Jason Hawrelak Recommendations are at the 99.7%ile — with all of the ones with issues being too low which is expected from one bacteria over-whelming the microbiome.
Antibiotics
There is a lovely study from [2013] that reports on antibiotic resistance of Prevotella copri [Table 1]. It states “suggesting that resistance to these antibiotics amongst Prevotella … microbiota is not intrinsic, but selected by previous antibiotic treatment”. Which suggests that the multiple courses in a short period of time contributed. I have no data on the two antibiotics that he took.
This hints that taking additional antibiotics may be ineffectual.
If blood tests for fungi has not been done, it should be suggested to the treating physicians.
We have an elephant in the Igloo! Let us address this item first. Then retest after a few weeks. I asked for suggestions including antibiotics, shown below.
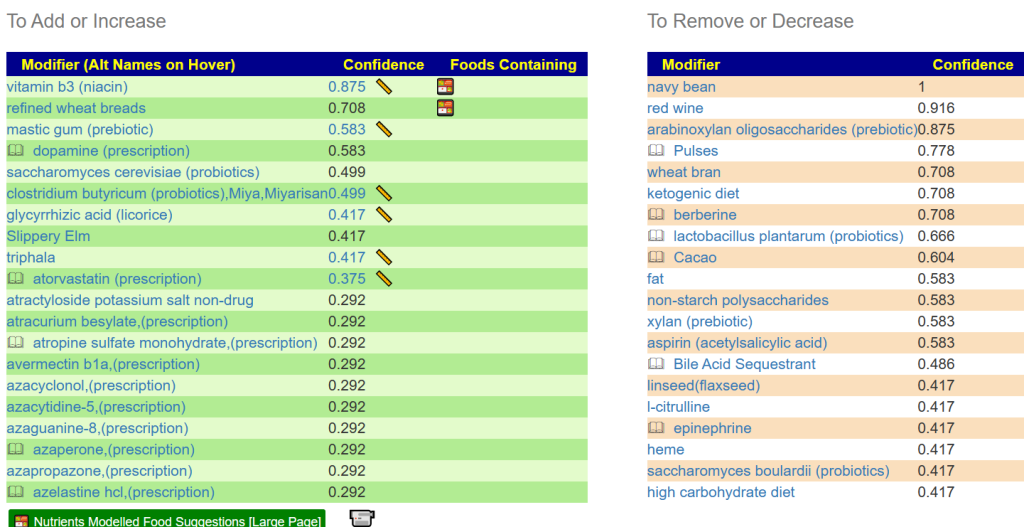
A good start would be Vitamin B3 (niacin). Which can cause flushing (i.e. white skin going lobster red), so a low dosage of 100 mg/day and increasing slowly. The other non-prescription items of note are:
- mastic gum (prebiotic)
- clostridium butyricum (probiotics),Miya,Miyarisan
- Possible: saccharomyces cerevisiae (probiotics) BUT saccharomyces boulardii (probiotics) is an avoid.
- Often this is mislabeled by retail product — so I would suggest skipping it.
- glycyrrhizic acid (licorice) – I prefer Spezzatina by Amarelli – available on Amazon and other stores
- Slippery Elm
- Triphala – an Indian herb mixture that we usually make into capsules. You could also make tea of it (if you can stomach it’s taste. It’s on Amazon.
- lactobacillus reuteri (probiotics) — not mixed with other species. Most lactobacillus and bifidobacterium are to be avoided.
Second Pass
.Should I do anything other than add b3, mastic gum, licorice, etc to my diet? Do I need to alter my diet in any way to lower the prevotella copri count? My diet right now is pretty bad. Burgers, pizza, etc. I went keto for a couple weeks a few months back to see if it made a difference and it didn’t so I figured if I was going to be miserable, I might as well enjoy what I eat.
From reader after reviewing above.
First the BAD NEWS, Keto is known to increase Prevotella copri, so the no positive impact is not unexpected. More BAD NEWS – what you are eating (high fat foods) will likely have adverse effects.
Above I focused on the Elephant, let us look at the ants and mice in the igloo. This is very easy to do and I made a video of it below.
Bottom line, cut out beef that are high fat content — lean beef only. Burgers and Pizza both use cheap high fat beef. Shift to rice for your source for starch (There are rice based pizza available). No soft drinks or sweets (cut sugar way down – sugar withdrawal can be rough).
Follow up: I would suggest doing a retest after 6 weeks of trying to alter your microbiome with the above suggestions. This will give us data to do your next “diet correction”. It is usually a multi-leg journey back to health.
Postscript – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I cannot tell people what they should take or not take. I can inform people items that have better odds of improving their microbiome as a results on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting.
The answers above describe my logic and thinking and is not intended to give advice to this person or any one. Always review with your knowledgeable medical professional.
Recent Comments