A reader request a review of his results:
I am a 26 year old male living in Germany. I have a M. Sc. iIn 2018, I did a semester abroad in St. Petersburg, Russia, and during the exam period got IBS. I think stress and/ or vegan diet, which I only tried for a few months, played a role. Extremely low Vitamin D was found, but nothing else.
I developed a lot of food intolerances since then.
In April 2021 I got a Biontech vaccination, and in the following days, noticed that I was tired all the time. It did not get better. I was barely able to finish my Masters Thesis as it was almost finished, but could not start working. Long story short, I now have a lot of the common CFS symptoms, additionally my hair fell out and low testosterone was found.
From a reader
Some technical notes: It cannot be diagnosed as CFS because it has not lasted long enough. It can be viewed as post-immune reaction syndrome. Second, I too have concerns about post-immune reaction syndrome this year, to explain why:
- Three COVID 19 vaccinations
- Tetanus vaccination
- Pneumonia vaccination
- Two Singles vaccinations
After each, I saw my system “act up”, Some measurable — such as a jump in blood pressure that took a couple of weeks to calm down. More often, i was dragging for a couple of weeks. Night Sweats. skin inflammation, etc.
To Vac or Not to Vac — that is really not the question. It is equivalent to saying “I will not wear a seat belt in case the car plunges into a lake and traps me in the car” The risk of that happening is very low compare to the risk of not wearing a seat belt. There is no rationality that can supported by rational analysis.
Some studies showing that vaccination does alter the microbiome.
- Oral Vaccination against Lawsonia intracellularis Changes the Intestinal Microbiome in Weaned Piglets. [2021]
- Links between fecal microbiota and the response to vaccination against influenza A virus in pigs. [2021]
- Vaccination against the brown stomach worm, Teladorsagia circumcincta, followed by parasite challenge, induces inconsistent modifications in gut microbiota composition of lambs.[2021]
- Changes in the ceca microbiota of broilers vaccinated for coccidiosis or supplemented with salinomycin. [2021]
Human studies have likely not been done because they will be misused by “anti-vaccination” people. We can be confident that changes will happen. The nature of the change will depend on the prior state of the microbiome – an unstudied area. The change from each vaccine will likely be different.
I should mention that I have read several personal reports of major improvement of microbiome conditions as a result of vaccination. A percentage may go either way.
Where do we go from here?
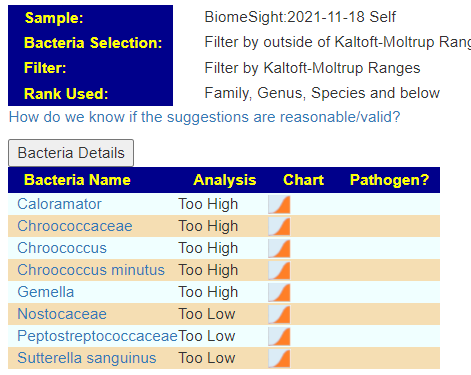
We have 3 sets of microbiome changers – stress, IBS and vaccination. Food intolerance was something of interest — alas, I could not find anything on PubMed that identifies bacteria associated with it. Doing a quick scan of my Biome View, nothing really stood out.
- Holophagae class high
- Deinococci class high
- Deinococcus-Thermus phylum
- Chroococcaceae family high
- Gemella family high
- Caloramator genus high (in terms of count — this was by far the highest of these)
Doing Due Diligence
- Quick ME/CFS choice returned not a single bacteria to be selected
- Advance Option IBS returned nothing with Kaltoft Moltrup,
- At 3%ile — two items were too low: Akkermansia muciniphila and Enterobacteriaceae
- At 6% — we added some highs: Lachnospira, Ruminococcaceae ( Ruminococcus)
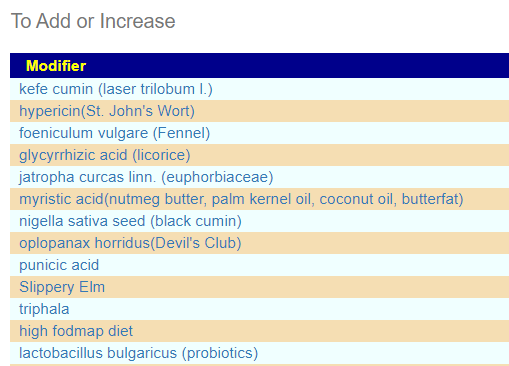
Kaltoft-Moltrup Ranges
This produces a list FULL of unusual supplements… and a few familar. This is the first time that I have ever seen lactobacillus bulgaricus appear in the to add list. Some of my personal preferences (from experience with ME/CFS) are there: glycyrrhizic acid (licorice), Slippery Elm,triphala and quercetin,resveratrol
My general impression is that our list of usual suspects is really not there,
Time to Beat the Bushes
KEGG Generated Suggestions
The Weights were all below 20 — i.e. marginal, with Sun Wave Pharma/Bio Sun Instant, being the best of the short list
Similarly the supplement list was short at 10%ile and none at 5%ile
- beta-alanine
- D-Ribose
- L-Histidine
- Molybdenum
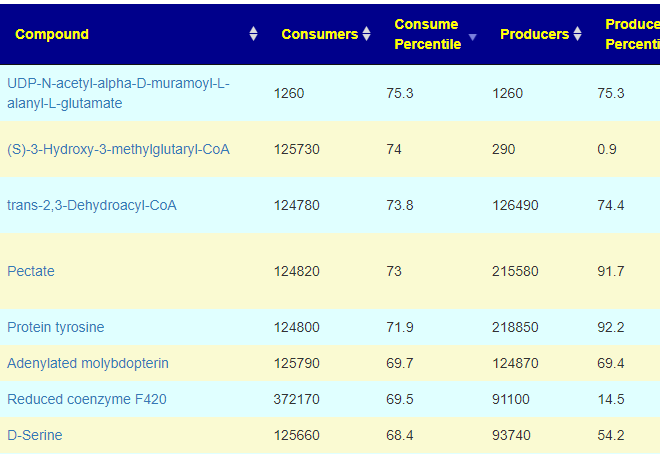
Compounds Produced and Consumed Page
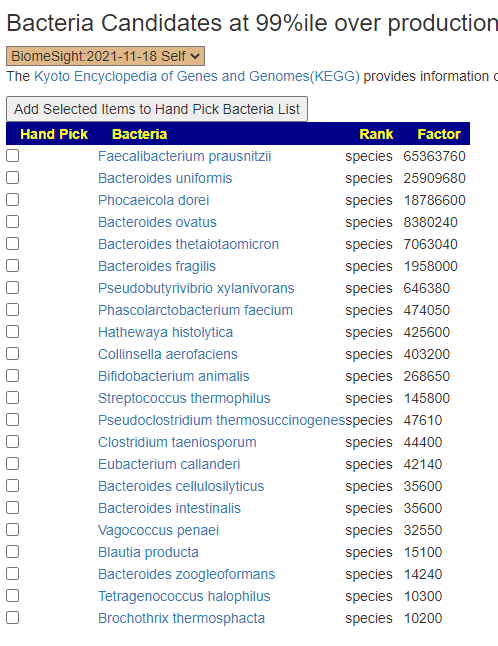
Looking at the new Compounds Produced and Consumed, there were a number of items that had high ( > 99%ile) production – with 600 items listed, we would have expected just 6 (1%) not 41!!:
- ADP
- all-trans-Heptaprenyl diphosphate
- 5′-Deoxyadenosine
- 5-Phospho-alpha-D-ribose 1-diphosphate
- Acetaldehyde
- AMP
- CO2
- Diphosphate
- Fumarate
- Menaquinol
- NADH
- NADPH
- S-Adenosyl-L-homocysteine
- UDP
- Uracil
- Arsenite
- H+
- N-Acylsphingosine
- Xanthine
- Acetoacetyl-CoA
- Acyl-carrier protein
- D-Amino acid
- Protein lysine
- Protein-L-arginine
- (3S)-3,6-Diaminohexanoate
- 5-Methylthio-D-ribose
- Acetyl phosphate
- Alcohol
- D-Xylulose 5-phosphate
- Glycyl-tRNA(Gly)
- N-Formimino-L-glutamate
- Orthophosphate
- (S)-4,5-Dihydroxypentane-2,3-dione
- L-Sorbose
- N-Acetyl-beta-D-mannosaminyl-1,4-N-acetyl-D-glucosaminyldiphosphoundecaprenol
- 6-Deoxy-L-galactose
- Protoporphyrin
- tRNA
- D-Mannose 1-phosphate
- Spermidine
- Glycolate
In terms of consumers, the highest percentile was 75.3%ile, In fact most of the consumed items appear ‘balanced’
Proposed Model
Because events were recent, we have high volatility in the microbiome’s bacteria. I saw similar at the start of my relapse… the various clans of bacteria are fighting each other with short term victors of one group and then a reversal.
The apparent issue is massive overproduction of compounds!!! How to address that may mean that I need to add more code to identify the key bacteria responsible and thus the page changed as shown below. This is a logical but experimental novel approach.
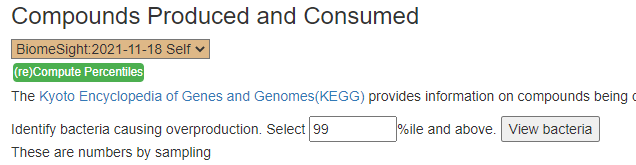
The result is shown below:
The result is show below. None were very high by themselves, Five were around 75%ile
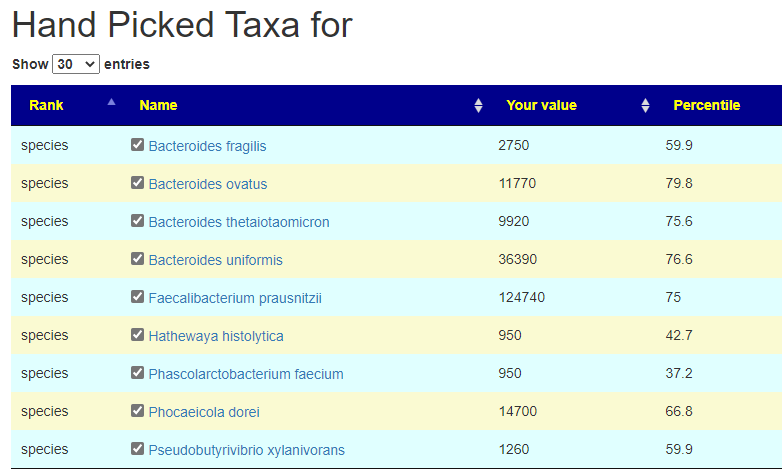
From this hand pick selection, we proceed to get suggestions. The results are shown below
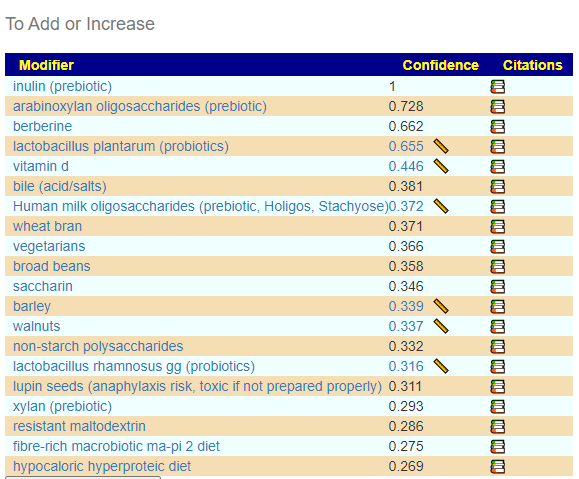
and the to-avoid
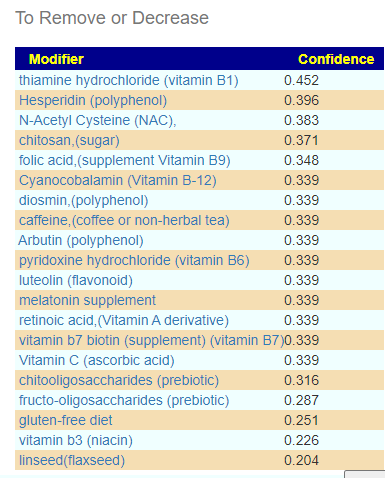
This looks similar to what I often see with ME/CFS people. That is, breakfast porridge made from barley with inulin and wheat bran with walnuts (which is my own regular breakfast!) with yogurt containing lactobacillus plantarum. There are some interesting studies in this area:
- Ingesting Yogurt Containing Lactobacillus plantarum OLL2712 Reduces Abdominal Fat Accumulation and Chronic Inflammation in Overweight Adults in a Randomized Placebo-Controlled Trial
- GABA enhancement by simple carbohydrates in yoghurt fermented using novel, self-cloned Lactobacillus plantarum Taj-Apis362 and metabolomics profiling
- Influence of Lactobacillus plantarum on yogurt fermentation properties and subsequent changes during postfermentation storage
- Probiotic yogurt containing heat-treated Lactobacillus plantarum enhances immune function in the elderly
Additional Lab Results from User
After getting to this point, the reader reported some recent lab results. Some are of interest:
- Vitamin D was just 28% into the normal range, so the vitamin D suggestion above is reasonable
- His coagulation factor II (G20210A/G) was at the high end of normal — I have the same coagulation issue and found that turmeric with black pepper or piracetam helps greatly — especially with brain fog and slowness.
- Protein S was low (barely in normal range), See Protein S deficiency
Issues causing hypercoagulation (thick blood) was shown to be common with ME/CFS by David Berg back in 1999, for articles and townhall transcripts (hosted by me!) see this page. This appears of part of this person’s causality.
Neither G20210A nor Protein S are likely to be deemed clinically significant, thus my personal preference (regular heparin taken sublingual, held for 1 minute and then spitted out) is unlikely to be prescribed.
For ways of addressing these, see my CFS Remission blog.
The COVID Vaccine Overtones
Prior to my getting my first COVID vaccine, I had concerns about it triggering coagulation – an ongoing ME/CFS risk. The reason was simple, vaccines triggers an immune reaction — milder than having COVID — but still an immune reaction. COVID was at that time, well known to produce coagulation issues (Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia April 2020) so they was a risk. The severity would likely be far less than that of COVID, but still enough to push someone with borderline coagulation issue across into ME/CFS. This appears to be correct as shown by some studies, a few are:
- First diagnosis of thrombotic thrombocytopenic purpura after SARS-CoV-2 vaccine – case report, Dec 2021
- Acquired thrombotic thrombocytopenic purpura: A rare disease associated with BNT162b2 vaccine Sep 2021
- Thrombotic thrombocytopenic purpura: a new menace after COVID bnt162b2 vaccine Jul, 2021
- Systematic Review of Antiphospholipid Antibodies in COVID-19 Patients: Culprits or Bystanders? [2021]
- Antiphospholipid antibodies in patients with COVID-19: A relevant observation? [2020]
This also is suspected with Long COVID,
- Persistent clotting protein pathology in Long COVID/Post-Acute Sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin Aug 2021
- Late-onset hematological complications post COVID-19: An emerging medical problem for the hematologist, Jan 2022
- and in The Guardian’s edition of today, “Could microclots help explain the mystery of long Covid?” Jan 5, 2022
Bottom Line
The microbiome is just a part of a health analysis, a significant part but far from being complete. We have a model for the tiredness. IMHO, non-prescription anti-coagulation treatments may eliminate it over a few months.
We are going to do two approaches that are connected.
- Coagulation — which appears to be caused by the bacteria of concern (a topic that I cover on CFS Remission)
- Bacteria — the ones that appear to be causing over production of many compounds
Reducing some of the bacteria cited above will likely also help, since many are known to cause coagulation:
- “These results indicated that Bacteroides sp. and F. mortiferum can accelerate blood coagulation in vivo ” [1973]
- “Bacteroides fragilis, Bacteroides vulgatus, and Fusobacterium mortiferum …. demonstrate that LPS of selected gram-negative anaerobes activate HF and thereby initiate the intrinsic pathway of coagulation.” [1984]
- Interaction of Bacteroides fragilis and Bacteroides thetaiotaomicron with the kallikrein-kinin system [2011]
- “Bacteroides fragilis and Bacteroides thetaiotaomicron, were found to bind HK and fibrinogen, the major clotting protein, “
- Unhappy Triad: Infection with Leptospira spp. Escherichia coli and Bacteroides uniformis Associated with an Unusual Manifestation of Portal Vein Thrombosis [2021]
Some questions from reader:
- “The only probiotic I will add is lactobacillus plantarum. (Or also lactobacillus rhamnosus gg?) I will have to rotate that. Here is the question: I would also like to address IBS. I read on cfsremission that some probiotics, like Prescript Assist, could lead to IBS remission. Prescript Assist was also 2nd place on the KEGG recommendations, although you said the weights were marginal. Would it be not unreasonable to try Prescript Assist at some point, to address IBS?“
- Yes, I would suggest two-four weeks on a probiotic and then rotate to the other
- “Does this plan sound reasonable?:
- Continue to take: D-Ribose, Vitamin D, Coenzyme Q10, Multi-Minerals, Magnesiummalate, L-Carnitine
- Discontinue: VSL3, Citrullinmalate, Vitamin C, Vitamin B12
- Add: As many of the recommendations as possible from the Kaltoft-Moltrup suggestions, the KEGG recommended supplements, and the novel approach. Add anticoagulants.
- After 2 months test again.
- Yes, if sound very reasonable – track objective measurements as much as possible
- New results IgA 1 is at 4500 with normal range 500-2000. This may be related to the vaccination but IgA is associated with a lot of things.
- Abrupt worsening of occult IgA nephropathy after the first dose of SARS-CoV-2 vaccination [2022]
- Need for symptom monitoring in IgA nephropathy patients post COVID-19 vaccination [2021]
- “Results in the naïve-vaccinated group, the mRNA-1273 vaccine induced significantly higher levels .. of IgA (2.1-fold, P < 0.001) as compared with the BNT162b2 vaccine.” [2021]
Is it good to take the recommended herbs (triphala, licorice, slippery elm) in parallel with the probiotics, or first only the probiotics in rotation and after that only the herbs in rotation?
There is no universal rule. Usually, I do herbs first and then probiotics. In terms of a war metaphor, the herbs are the artillery’s softening up the enemy, the probiotics are the troops charging in at the disorganized enemy.