The reader describes their situation below:
I am living with LongCOVID following infection in March / April 2020. I contracted COVID-19 in the workplace, employed as a pharmacist at an NHS hospital in South Wales, U.K.I shared my story with WalesOnline at the latter stages of 2020 due to the lack of awareness around LongCOVID, and I share with you below for your interest.
📺 ‘Super-fit pharmacist who has ‘long Covid’ now left breathless by short walks’
📺 ‘30-year-old fitness fanatic with long Covid details his horrendous list of symptoms’
Unfortunately, I am still troubled by GI symptoms and despite improving over the past few months, I’m still having difficulty with bowel urgency / diarrhoea and mild abdominal pain. I lost 10kg in 10 weeks between July – Sept. 2020 (72kg at my lowest); thankfully this has recovered and I have gained weight, albeit chubbiness, weighing 88kg last week. I was diagnosed at the start of 2021 with ‘post-viral IBS’ and ‘leaky gut syndrome’, but GI clinicians are at a loss of how to proceed with my symptoms, hence my purchase of the BiomeSight kit. I have tried numerous diets (FODMAP, dairy-, gluten-free), again, to no avail.
I approach my 20th month since first being infected and I am still quite a distance from where I was pre-COVID doing all I possibly can to recover, so I would be extremely grateful for your insight, not only to help myself, but others in a similar situation.
Approach #1
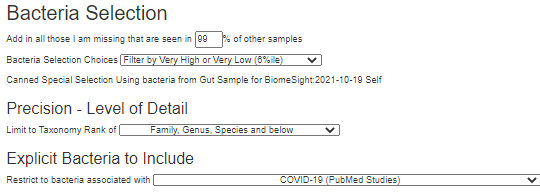
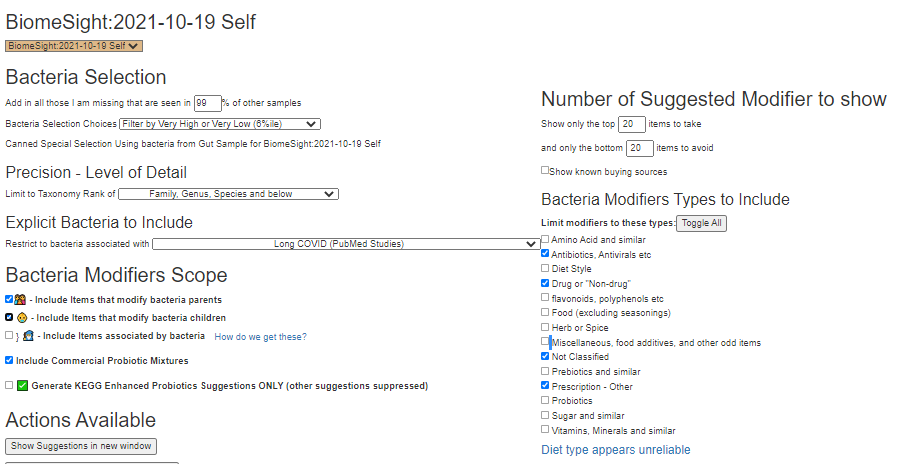
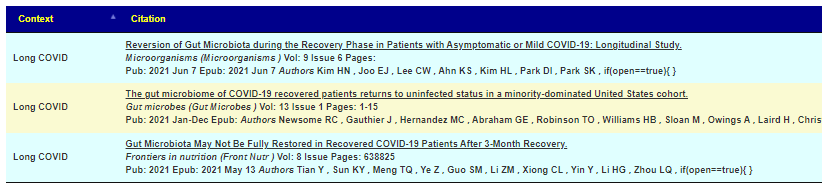
As we have two microbiome profiles for COVID from the US Nation Library of Medicine, I will apply each one using 6%ile filter (values in the top or bottom 6%ile) to get a feel for the ground work. Then I will apply the ME/CFS for a third one (because of the similarity of Long COVID and ME/CFS).
We end up with a short lists of bacteria (the titles links to the bacteria and studies reporting these shifts)
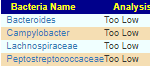
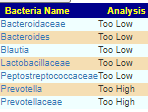
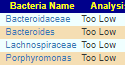
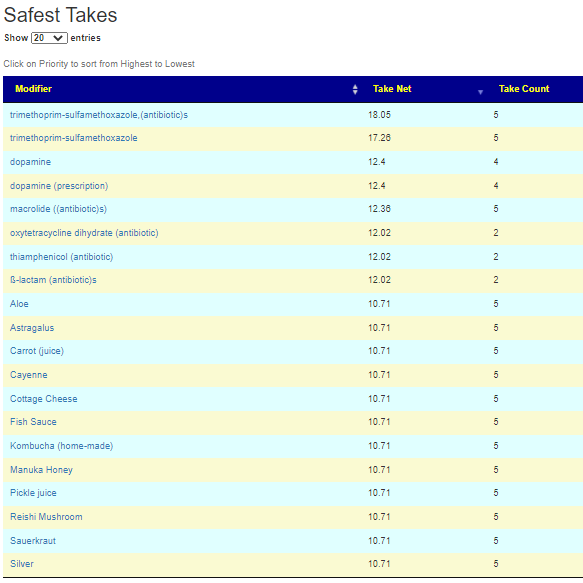
Almost everything is too low. Rather than examining suggestions from each of them, I will go directly to the consensus report. We hit a surprising 108 items on the safest take (items that will not shift any of the above in the wrong direction). Most are recommended in each case (Take Count = 3)
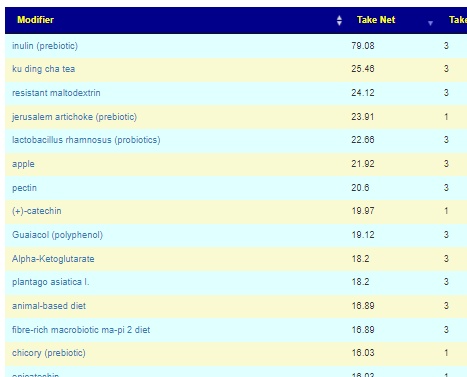
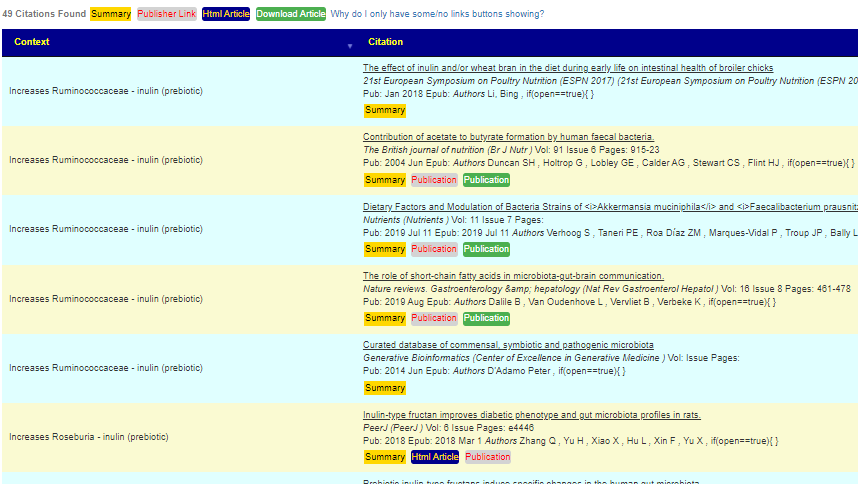
A few quick notes: Apples are very rich in pectin (some studies used apples and other pectin — I always try to keep data as reported and not do ‘well it’s just like…’ simplification). Similar with inulin and chicory.
The Safer text (some pro and some con) list was short and a bit of a mixed bag. With 108 items on safest, I would tend to ignore these. No need to include them.
On the avoid list we have “magnesium deficient diet” — which usually translates to magnesium rich or supplements.
I attach the complete list below of 304 different items.
Approach #2
This person is a pharmacist and thus looking at off-label drugs may be interesting for him to review. There are no accepted drugs for Long COVID, however, for ME/CFS often the top off-label drugs have often been used (with good results) by ME/CFS specialist (often at risk of professional censure). I have also added in CFS/ME with IBS (only Bacteroides Low was a match), and IBS to the consensus report.

The number of drugs that could influence these bacteria (good or bad) was almost 1300. I included some non prescription items to serve as a reference point (i.e. do drugs do better than some alternatives). In the small list of antibiotics at the top, I see several of the works for ME/CFS antibiotics — especially, those used by Cecile Jadin, MD: Tetracyclines, macrolides. Jadin does antibiotic rotation: 10 days on and 20 days off, then change to the next antibiotic. I have seen a few PubMed studies finding rotation was superior.
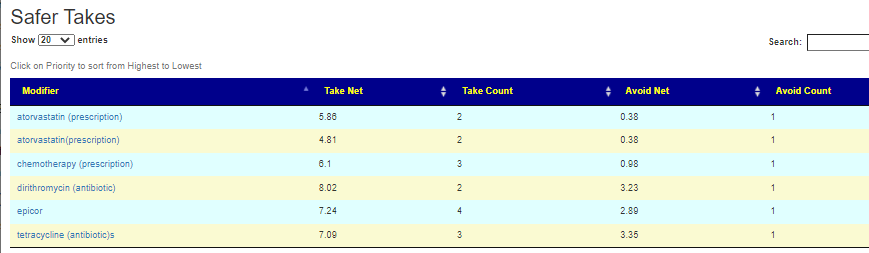
I noticed that several antibiotics often used for ME/CFS and IBS was on the avoid list: rifaximin (antibiotic)s, azithromycin,(antibiotic)s
The full list is attached
Approach #3
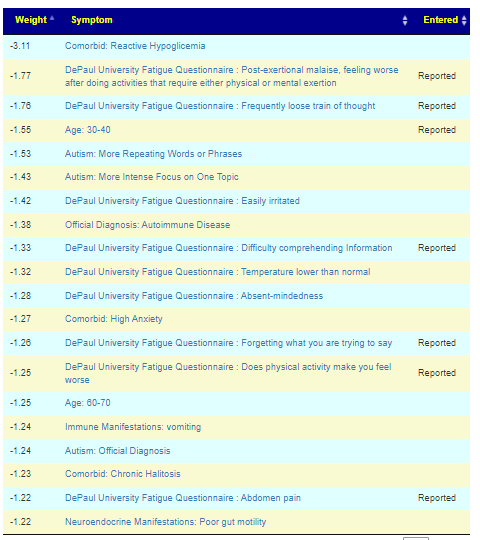
Above we worked on diagnosis, we are now going to switch to symptoms. My experience is that symptom-to-bacteria associations are much stronger than diagnosis to bacteria. Mileage will vary.
Oh have I mentioned that the symptom prediction from bacteria matches my symptoms almost completely? I think it’s 17 out of 20. Pretty incredible.
From a user in Europe by email on 11/11/2021
Below are his reported symptoms against predicted symptoms. It is interesting that many several predicted symptoms are autism related (which he does not have). This approach uses the bacteria that citizen science has associated to the symptoms (instead of clinical studies to the diagnosis). In theory, it will often be more sensitive for identifying the bacteria of concern.
See the video for how we do this. The final suggestions in Excel/csv format is below
Bottom Line
The intent of Microbiome Prescription site is to improve the odds of helping by working off studies on the US National Library of Medicines (at present, there are almost 6000 articles that we were able to harvest information from). We are very open on the where we get data, for example – for where we get the list of bacteria associated with a condition
And sources for how we know that something changes bacteria populations. In this case because of the high number of studies on inulin it will receive a high weight if certain bacteria are being targeted.
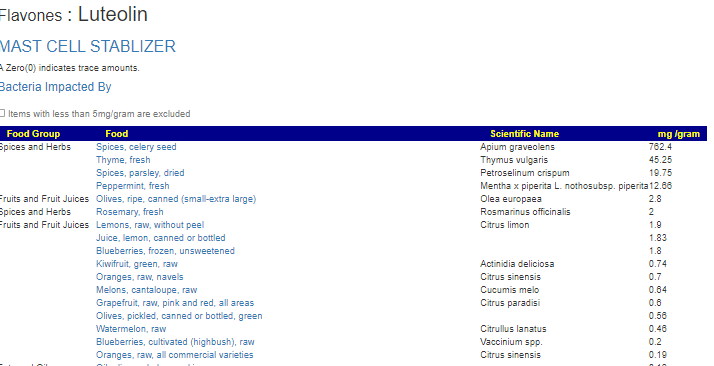
We also try keeping faithful to the term used in the studies — apple contains large amounts of pectin, while some would just combined these to pectin (or apples), we attempt to keep the fine details. One related area that needs calling out is studies using items like luteolin (flavonoid). If you click on these, you will go to a summary page with a link to foods containing it
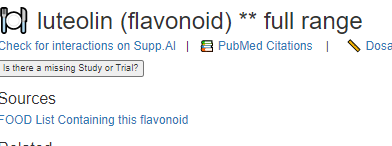
We have a list of foods and amounts that contain it. It’s an extra step, but since these foods were not cited in the study, we “keep religion” and only cite what was used.
I am not licensed medically, and thus there is no clinical experience (or bias) for the suggestions. It is an uber-logical model.
With that said, this person needs to sit down with his significant other, look thru the lists and decide which options they wish to try. Being a trained pharmacist means that he can also evaluate the prescription options for risk and in some cases, try to game the system… for example: Atorvastatin … he may want to test for the conditions where it would be prescribed, if he is a little high — he may wish to use that as a “standard of care” rationale for getting a prescription — it’s an off label use (like Viagra was not intended for what it is prescribed for today).
As always, any planned action should be reviewed by their knowledgeable medical professional before starting.
EU/JRC Technical Report related
Caution for other Long COVID Patients
Before COVID, you had a unique microbiome, COVID “infection formed” it to suit its needs. These changes caused symptoms, made it easier for secondary infection and allow “alternative community of bacteria” to become established. How it changed depends on what it was like before and which variant of the virus. While the above suggestions are likely similar to what your suggestions could be, it is really important to get your own microbiome sample to work from. There will be large differences between people. With this approach, we can be single person specific for a treatment plan.
P.S. This sample was done via Biomesight, a UK based firm
Recent Comments