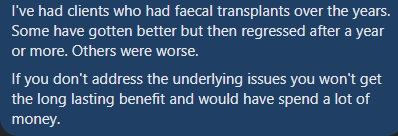
A reader sent me an email shown below:
…did a NirvanaBiome test before and 4 weeks after finishing the FMT. As far we can see her gut condition only got worse.”
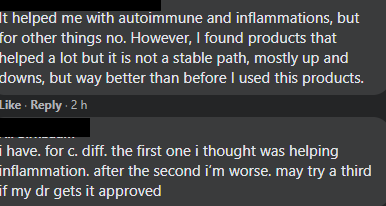
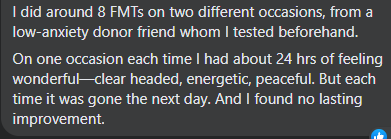
On The Gut Club: Stool Test Discussion Group Facebook group, some other comments were shared
My first goal is to try to understand what went wrong and how. Then looking at “where do we go from here”. Ending with a reading list on FMT.
Additional Personal Experience with FMT shared
Analysis of Changes
I started with comparing Bacteria/Taxonomy Out of Range Over Time which showed 63 items. The most interesting are below. Percentile means where in a collection of 2000+ samples that the reading is. For example 97%ile means that 60 samples had more than this and 1940 samples has less – most people would deem that to be an excessive overgrowth. Prior means before the FMT, After means weeks after the FMT.
| Bacteroa | Prior Percentile | After Percentile |
| (class) Clostridia | 97.8 | 99.3 |
| (class) Gammaproteobacteria | 95.4 | none |
| (family) Lachnospiraceae | 95.8 | none |
| (family) Ruminococcaceae | none | 100 |
| (genus) Ruminococcus | 99,8 | 100 |
| (order) Enterobacterales | 97 | none |
| (species) Ruminococcus bicirculans | none | 100% |
My initial thought on seeing these results was – are we using the same lab? We are.
The mechanism of getting names is finding patterns in the raw data. Lachnospiraceae and Ruminococcaceae are both children of Clostridiales, so we may have
- Clostridiales requires 100 matches
- Lachnospiraceae requires these matches and 20 more
- Ruminococcaceae requires these matches and 15 more
- There may be 8 matches in common with these two
This dramatic shift may be (1) a defect in the classification algorithm or (2) a bug in my specific import routine for CosmosId [which I am looking at) or (3) sibling families taking over [siblings tend to like the same environments] , I am inclined to the first cause(1) since the data is pushed through the same code(2) but (3) is almost as probable as (1). See my 2019 The taxonomy nightmare before Christmas… post for background.
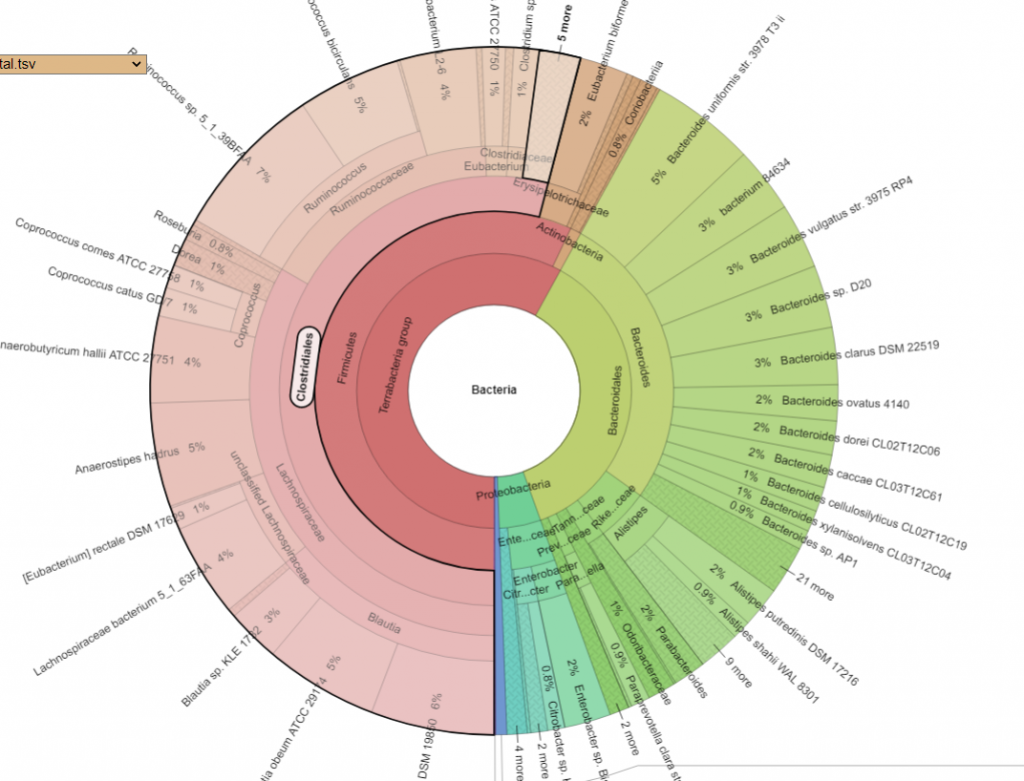
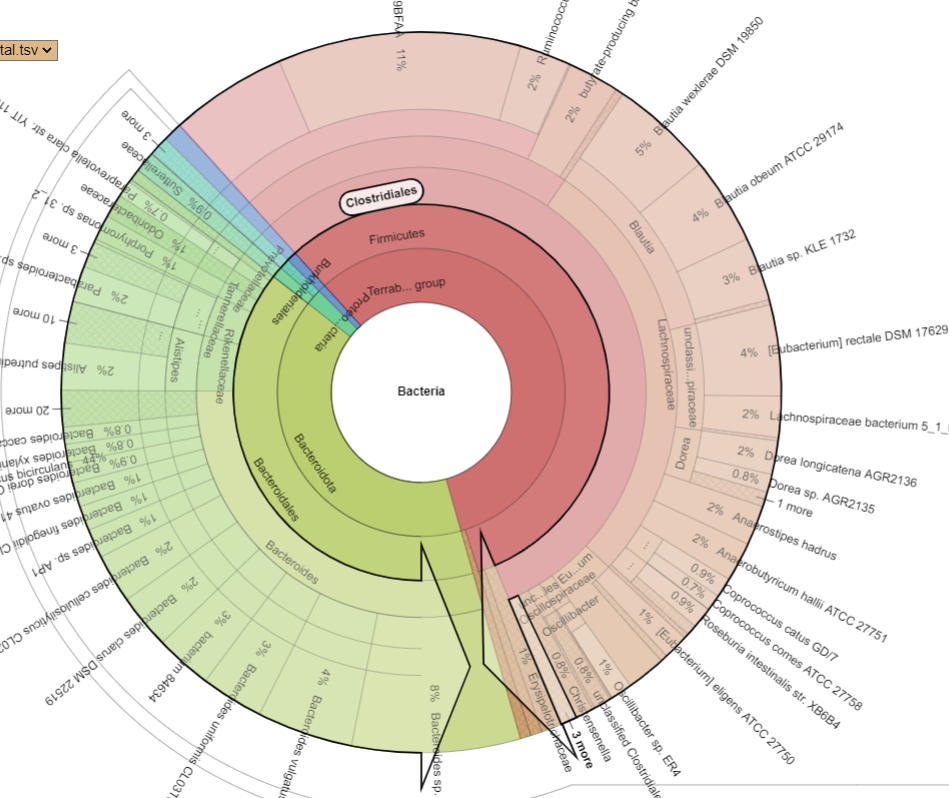
Pie Charts
The two charts below show the growth of Clostridiales and the reduction of every other order. I have often described Fecal Matter Transplants as equivalent to an Organ Transplant (or Blood Transfusions) with the same issues of rejection being significant. We do not know yet now to “type” or test the new item for compatibility.
I speculate that there may have been warfare with several orders weakened, Clostridiales was already near an extreme value — my gut feeling is that bacteria with strong overgrowth are dominated by strains that have the following characteristics
- They are more robust (i.e. more resistant to bacteriocins (natural antibiotic) produced by other bacteria
- They produce significantly more strong bacteriocins
The diagram below helps to explain bacteriocins. It show different strains of Lactobacillus Reuteri. Reuterin is the bacteriocins(natural antibiotics) produced. Some produce a high amount, some a low amount and others none.

Drilling down into Clostridiales we see major shifts. CosmosId report by strains, so these numbers are reliable
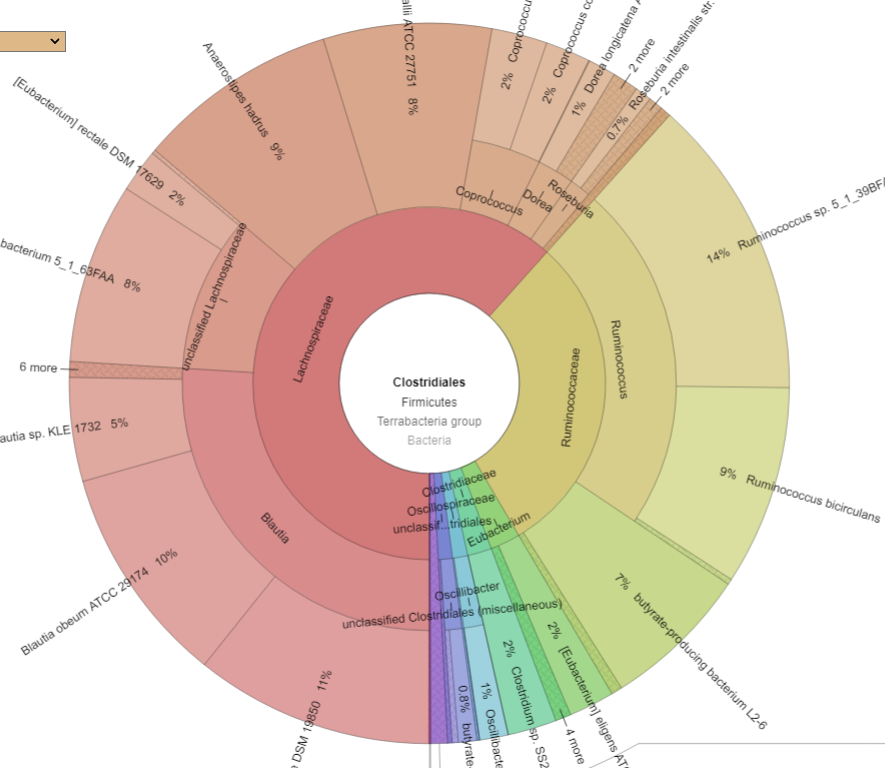
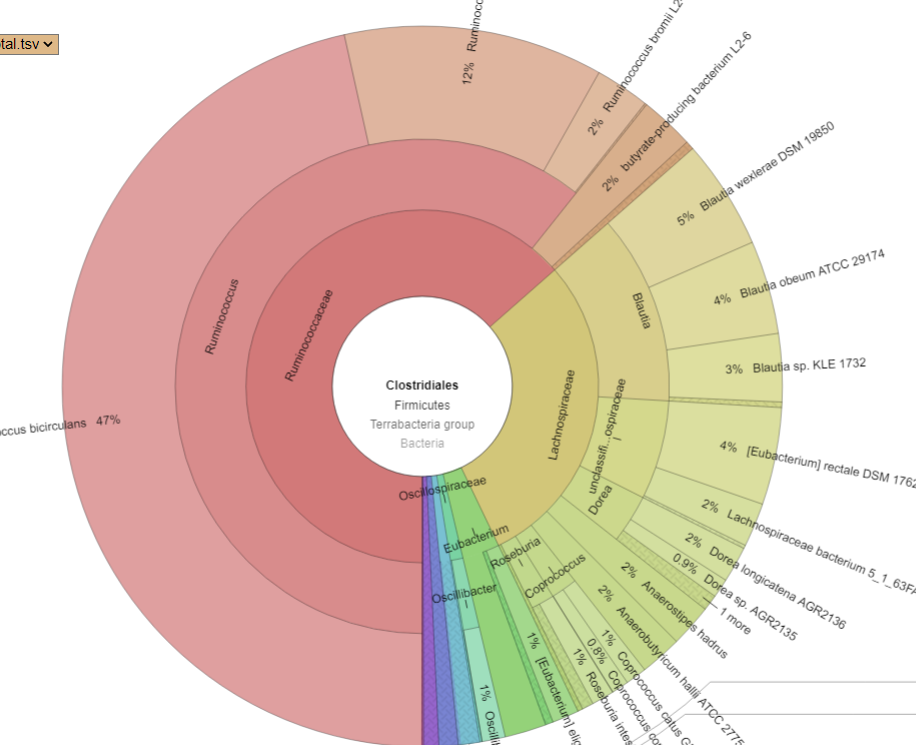
What we see ins that one species EXPLODED, Ruminococcus bicirculans. Prior to the FMT, it’s count was 47,810 or 0.5%, after it jumped to 444,900 (44.5%!!!) – a 10x increase. Whether it was a new strain that was introduced by the FMT that the existing microbiome could not handled as well as the donor (I deem more likely) or an existing strain that filled the vacuum resulting from the FMT bacteria and native bacteria wiping each other out (less likely) is speculation.
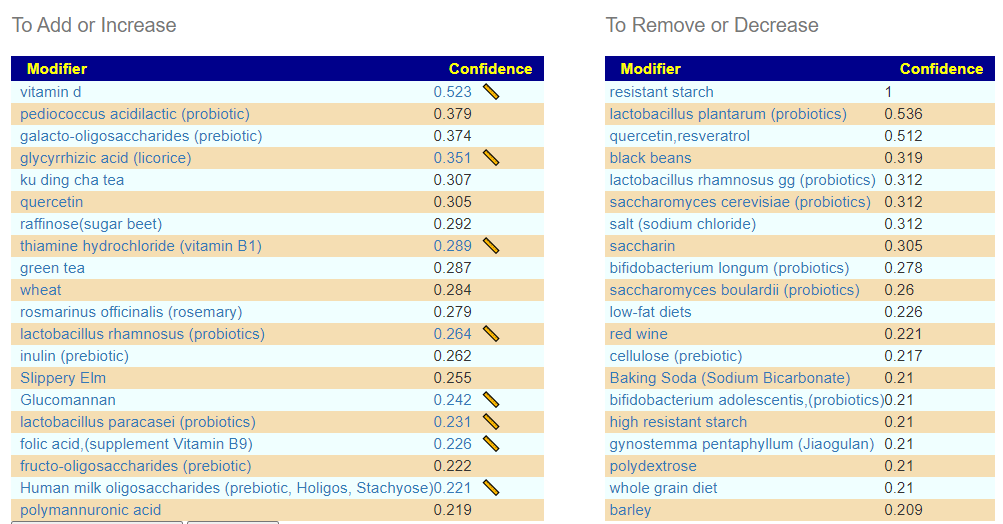
Suggestions
We have an idea of what may happen, apart from being a visual warning in the above diagrams to people considering FMT. The key question for this person is how to undo it. For this troublesome strain, we know some things that will increase or decrease it. I would focus on this strain alone and do a deep “spring cleaning” of supplements.
- Items to increase
- camelina seed
- ginger
- ginko
- glycyrrhizic acid (licorice)
- nigella sativa seed (black cumin)
- rosmarinus officinalis (rosemary)
- Slippery Elm
- caffeine,(coffee or non-herbal tea)
- melatonin supplement
- quercetin
- berberine
- mediterranean diet
- thiamine hydrochloride (vitamin B1)
- vitamin b7 biotin (supplement) (vitamin B7)
- folic acid,(supplement Vitamin B9)
- Cyanocobalamin (Vitamin B-12)
- Vitamin C (ascorbic acid)
- lactobacillus paracasei (probiotics)
- lactobacillus reuteri (probiotics)
- lactobacillus salivarius (probiotics)
- bacillus amyloliquefaciens (probiotic)
- Items to stop (if taking)
- Dendrobium officinale
- Ginseng
- gynostemma pentaphyllum (Jiaogulan)
- noni
- triphala
- bile (acid/salts)
- fish oil
- polymannuronic acid
- ,resveratrol
- iron
- zinc
- high fiber diet
- whole grain diet
- wheat
- lactobacillus acidophilus (probiotics)
- lactobacillus plantarum (probiotics)
- bifidobacterium adolescentis,(probiotics)
- bifidobacterium longum (probiotics)
- lactobacillus rhamnosus gg (probiotics)
- bacillus subtilis (probiotics)
- saccharomyces boulardii (probiotics)
- Prebiotics
- resistant maltodextrin
- high resistant starch
- resistant starch
- gum arabic (prebiotic)
- fructo-oligosaccharides (prebiotic)
- oligosaccharides (prebiotic)
- partially hydrolysed guar gum,fructo-oligosaccharides (prebiotic)
- sialyllactose (oligosaccharide ) (prebiotic)
- cellulose (prebiotic)
- Human milk oligosaccharides (prebiotic, Holigos, Stachyose)
- ß-glucan
Looking at the Kaltoft-Moltrup Range based suggestions, we see a lot of bacteria selected as abnormal
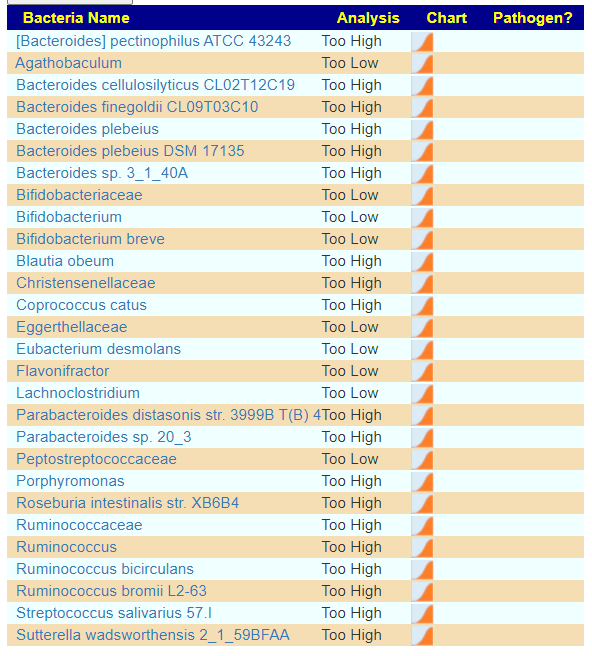
And we see most of the above items are on the suggestions for this combination:
Bottom Line
I would suggest (after reviewing with your medical professional) the above changes and then do another Nirvana sample after 6-12 weeks to see what has changed. I would expect this Ruminococcus bicirculans. to be significantly reduced, the question is what will replace the 44% of the microbiome it currently occupies.
I was curious if we could infer something about the donor by looking at these changes. I looked at life style that could impact Ruminococcus bicirculans. etc and found that
A common sense (A priori) definition of what would be a healthy donor will often be someone that fits these two features, i.e. an athlete. ” Recent trends show more athletes trying a low-carbohydrate, high-fat (LCHF) diet for endurance performance. ” [Low vs. High Carbohydrate Diets for Endurance Performance] IMHO, this a priori common sense healthy donor is wrong — athletes have abnormal microbiomes. A priori is defined as “denoting reasoning or knowledge which proceeds from theoretical deduction rather than from observation or experience.“
The compatibility issue is not only at the microbiome but diet and exercise style. If the recipient does not consume the same diet as the donor, the transfer may go in odd directions. Similarly, we know exercise impacts the microbiome. A “desk jockey” getting the microbiome of someone that cycles for 4 hours a day will likely fade quickly.
Prior Posts on FMT
My interest in trying to understand different FMT responses go back at least 5 years. The following posts are likely worth reviewing. My feeling continues to be that the downside risk for the upside benefit is still too low to be a desirable course of action. Typically, it is an improvement that does not persist for extended periods. I believe a committed microbiome manipulation with regular retests and adjustment has considerably less downside and equivalent upside benefit that will likely persist longer — especially, if at least two samples and adjustments are done a year once sufficient benefit has been obtained.
- Fecal Transplants – not for the herx adverse!, 2016
- uBiomes before and after a Fecal Microbiota Transplant, 2017
- A Healthy FMT Donor Microbiome and response to FMT, 2017
- Theortical Protocol for Fecal Transplants for CFS/IBS etc , 2017
- A case study of a fecal transplant for CFS, 2018
- Current State of Fecal Matter Transplants, 2018
- Fecal Matter Transplants and Phages [2020]
Different ways of Doing FMT
I am tossing some technical information for those that are interested in how FMT can be done. There are many ways, including “the turkey baster” aka “Turd Burglars“. IMHO, it should be done under medical supervision with adequate testing (including comparing the donor’s microbiome, and life style to the recipient)
By Enema
This was used by the above
FMT with Enema – 6 doses, 1 every other day (11 days)
No antibiotics are used!
Pre- and probiotics (phgg, bifido)
Prior
- Do not stop medication
- follow a liquid diet the night before the first administration (and not the other 5!!!)
- cleansing water enema in the morning before FMT
- place the dose from the freezer in the refrigerator the night before. allow the dose to reach room temperature in the morning.
- swallow 1 imodium after awakening (only) for the first dose
- limit yourself to a light (liquid) meal
During
- do not eat or drink anything during and immediately after the enema.
- work in stages with a limited dose (but within 10 minutes on the left side)
- use gravity to keep everything inside, e.g. a pillow under the hip
- take a few deep breaths regularly
- alternate position (left side, back, stomach, right side), every ten minutes (left is best for keeping inside)
- regularly massage the dose upwards gently
- try to keep the dose for ideally more than 6 hours
- rest, relaxation and sleep are the best activities during the therapy days
After
- do not immediately make major changes to your daily diet
- not drinking and being (somewhat) thirsty helps to withdraw fluid from the injected dose
- fibers help the new bacteria to settle. gradually introduce fiber into your diet. fiber rather through food than supplements.
Centre for Digestive Diseases – Doctor Thomas Borody
” Dr Borody has overseen over 12,000 FMTs, creating a wealth of proprietary clinical data and insights.” Antibiotics are frequently used prior to FMT. He is likely the leading Australian MD that does FMT.
- Faecal Microbiota Transplantation
- ” published response rates in some studies using FMT to treat UC greater than 50%1.”
- “In our experience FMT may help symptoms of Irritable Bowel Syndrome (IBS) however, this not guaranteed. “
Selected publications
- Faecal microbiota transplantation alleviates symptoms of depression in individuals with irritable bowel syndrome: A case series
- Response to article “A retrospective outcome study of 42 patients with chronic fatigue syndrome, 30 of whom has irritable bowel syndrome. Half were treated with oral approaches, and half were treated with faecal microbiome transplantation”
- Evolution of fecal microbiota transplantation in methodology and ethical issues
- Fecal microbiota transplantation as a new therapy: from Clostridioides difficile infection to inflammatory bowel disease, irritable bowel syndrome, and colon cancer
- Specific Bacteria and Metabolites Associated With Response to Fecal Microbiota Transplantation in Patients With Ulcerative Colitis
- Microbiota Transfer Therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: An open-label study
- Fecal microbiota transplantation: A ‘How-To’ guide for nurses
- “Mild and transient side effects reported with the procedure include abdominal cramping, dis-comfort and bloating, belching, diarrhea, constipation, nausea and flatulence, which can occur while the infused bacteria are establishing themselves. A case of worsening inflammatory bowel disease, two cases of norovirus gastroenteritis and one case of E. coli bacteremia have also been reported, however FMT could not be established as the cause of these events” — NOTE The defensive “could not be established as the cause of these events” interpretation
There are more publications on his website.
Recent Comments