Backstory:
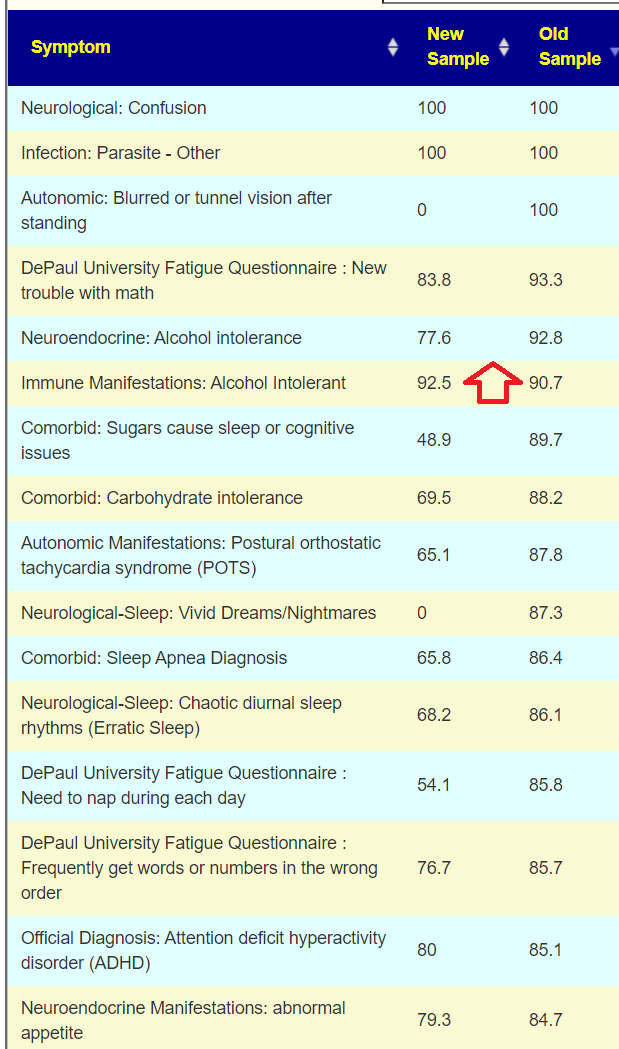
Hello, I’m a 21-year-old with a moderate case of CFS. Currently, I’m having serious problems with concentration, reading, memory, and executive function to the extent of needing a caregiver. I react to any food with neurological symptoms and gas, and my energy production is so impaired that I get hungry just two hours after a large meal. I would like to hear your analysis of the sample, especially your opinion about the sky-high amounts of Bilophila wadsworthia.
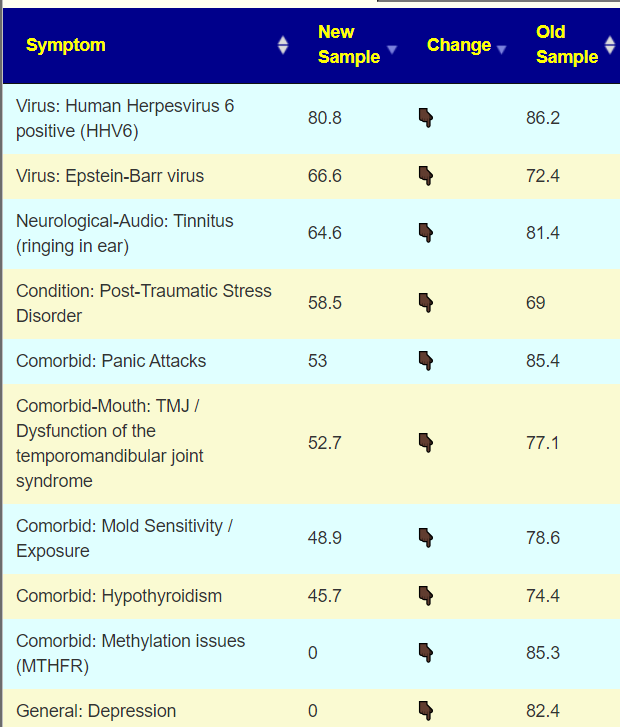
At 13 years old, I started having hemiplegic migraines with aura, including paralysis, speech, vision, and orientation loss due to an ATP1A2 mutation. These were thought to be incurable until I randomly found an off-label local medicine, metamizole, which is prohibited in the US, Canada, and the EU but is available in my home country, Ukraine. This medication was effective in mitigating the aura. I started taking it every day for four years starting at age 16. Recently, I learned that it increases prostaglandins and has an immunosuppressant effect like NSAIDs in general. I suspect that my daily use of this medication may have contributed to developing CFS and hypersomnia through unchecked mucosal infections.I was also diagnosed with 160,000 copies of HHV6 in my blood via PCR, which persisted for years (I stopped testing for it). I tried valganciclovir, artesunate and IFN-a, which did nothing but further worsened my baseline. A year and a half ago, I started Joshua Leisk’s Born Free protocol (https://bornfree.life/download/BF_Protocol.pdf), which improved my metabolic situation significantly. However, I coincidentally started living in an unhygienic, mold-infested environment, and subsequently had GI and Eustachian tube infections. After taking nifuroxazide, amoxicillin, and metronidazole a year ago, my condition worsened to a moderate level, and I haven’t recovered since.
I suspect that gut issues are the cornerstone of my problems, but I am quite lost lost regarding how to handle them. I am eager for any new information.
The model that I use for ME/CFS is some event (stress, food poisoning, virus, inoculation or dozen of other possible events) cause the microbiome to shift in response. The shifts can result in a feedback loop that keeps this “evil microbiome” shift going. A percentage recover naturally over time, and we have a longitudal study from Bergen Norway to illustrate this. The trigger was giardiasis for a large number of people. A medicine like metamizole on a continuous basis can easy cause this to happen.
Analysis
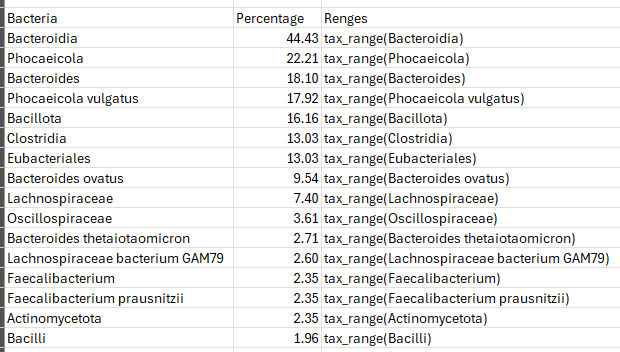
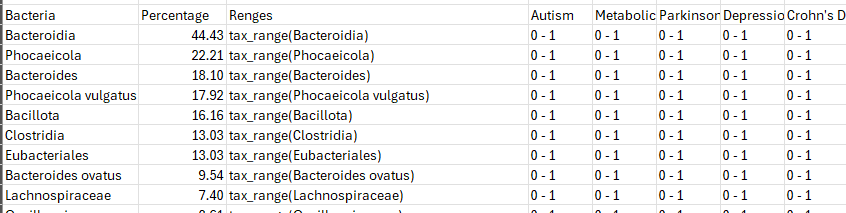
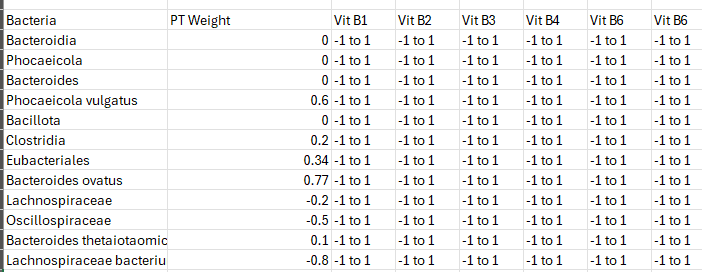
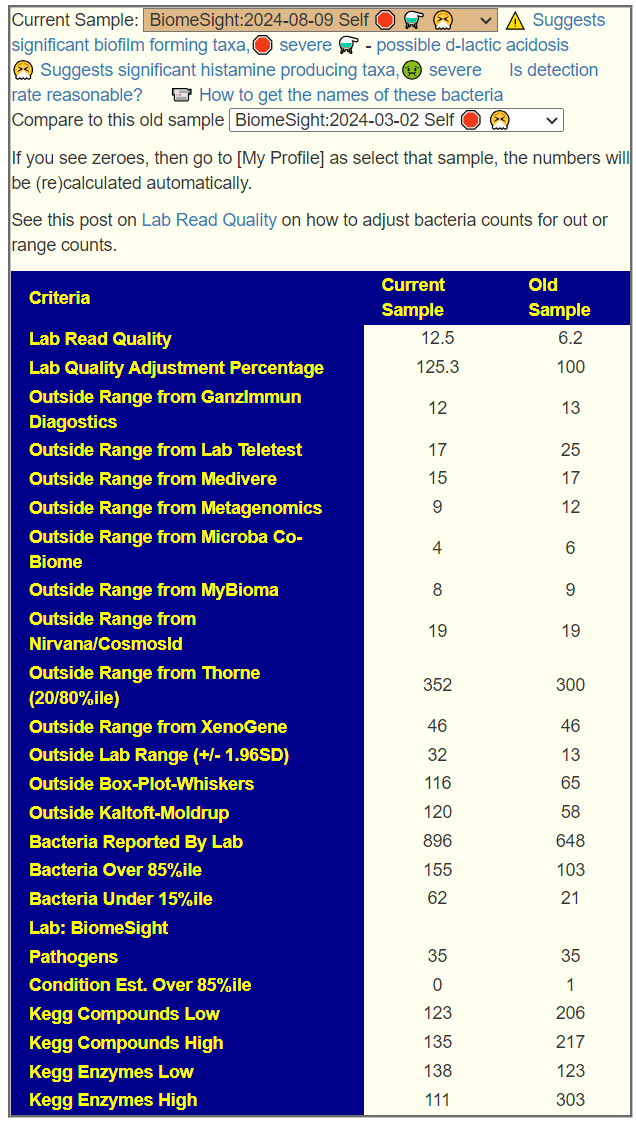
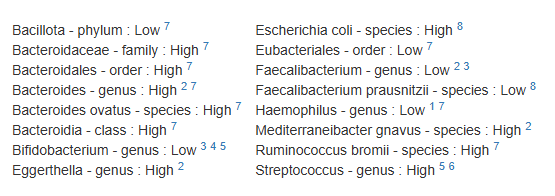
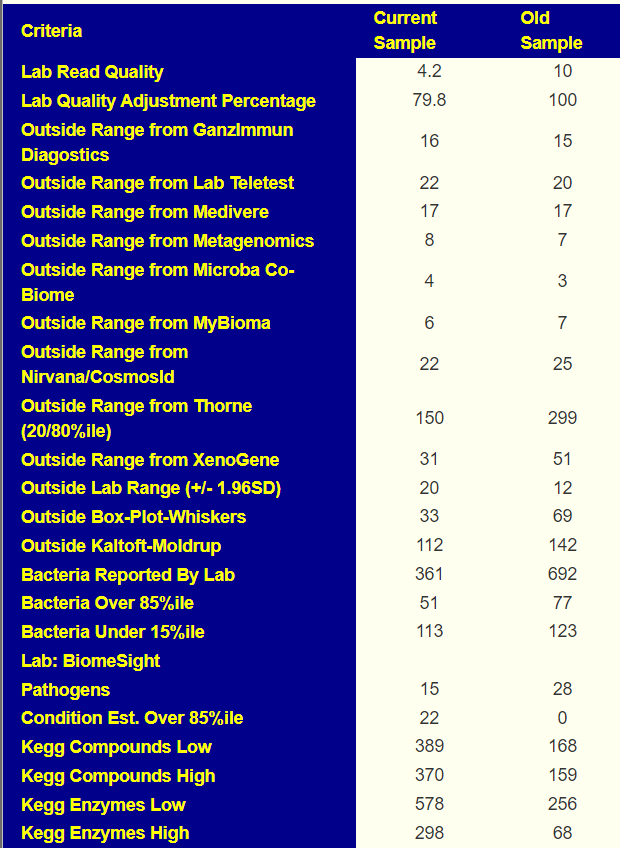
We have two samples available, so let us look at the before and after antibiotics comparison. My impression is that the antibiotic made things worse. The latest sample has more items out of range despite having ~20% less bacteria reported
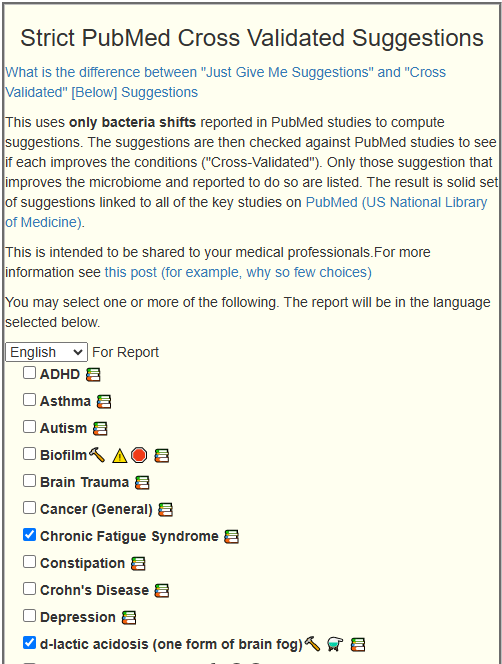
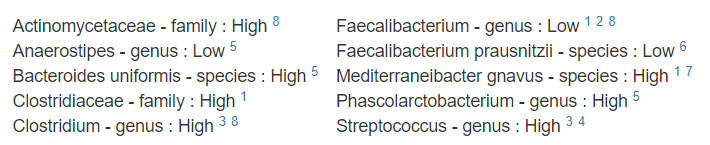
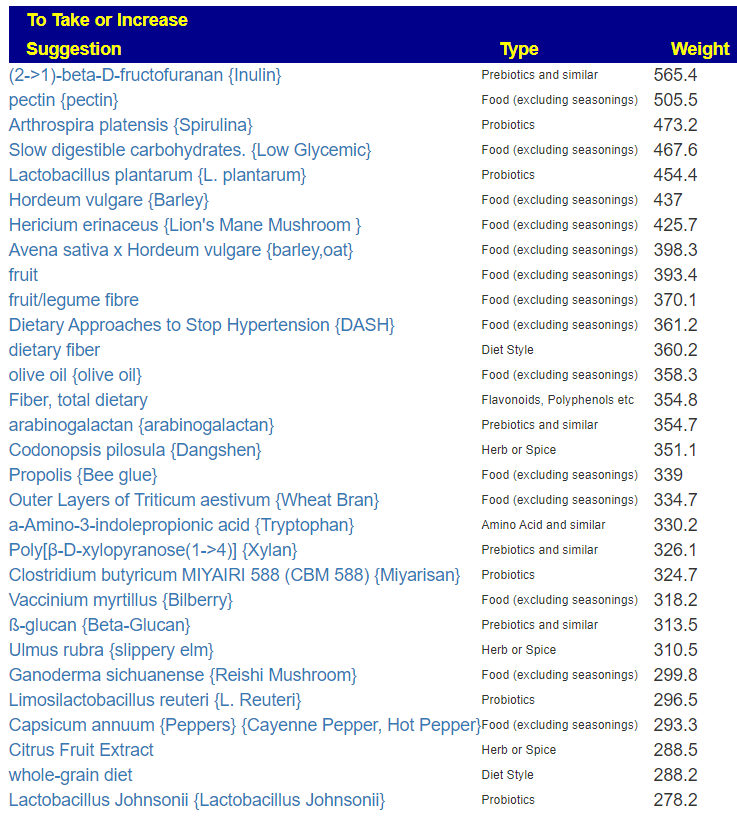
Since we are nominally dealing with ME/CFS, we can use the cross validated suggestions to get conservative suggestions of what may help
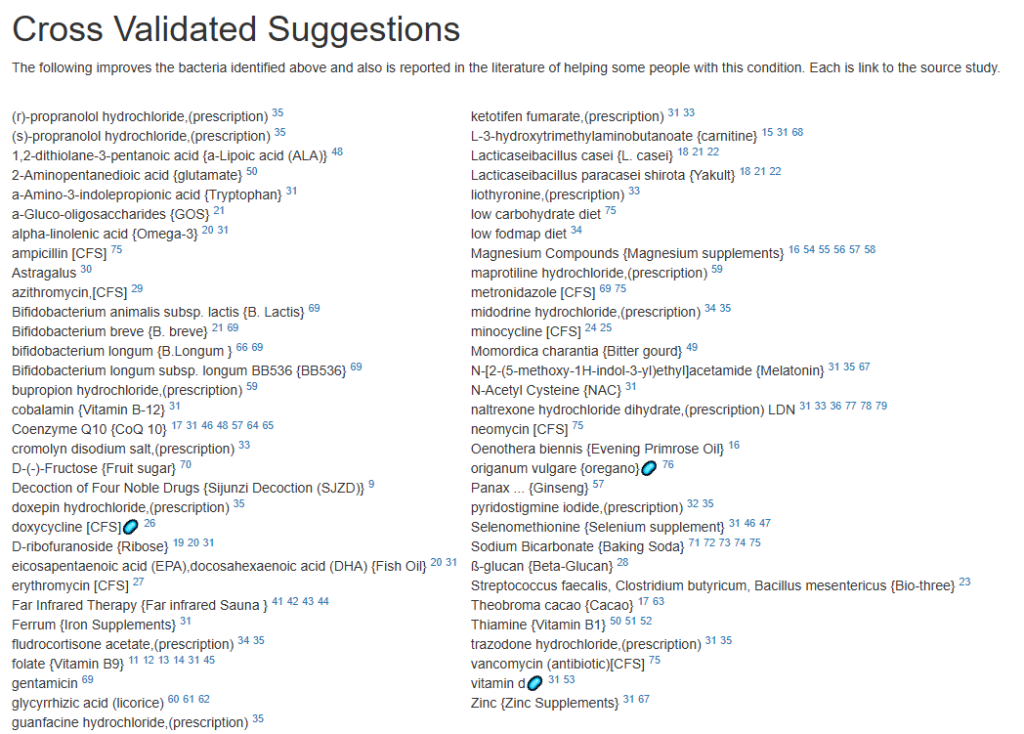
The result is a massive list!

We will backtrack to “Just Give Me Suggestion Including Symptoms” so we can rank order these suggestions.
The top items are antibiotics, with 60% being those used to treat ME/CFS (i.e. on the above cross validated list). I tend to follow Jadin’s approach so, do one of those marked [CFS] for a course (7-10 days) and the next month(3 weeks off), move to a different one. After the 3rd one, get a new microbiome test to see the next course adjustment.
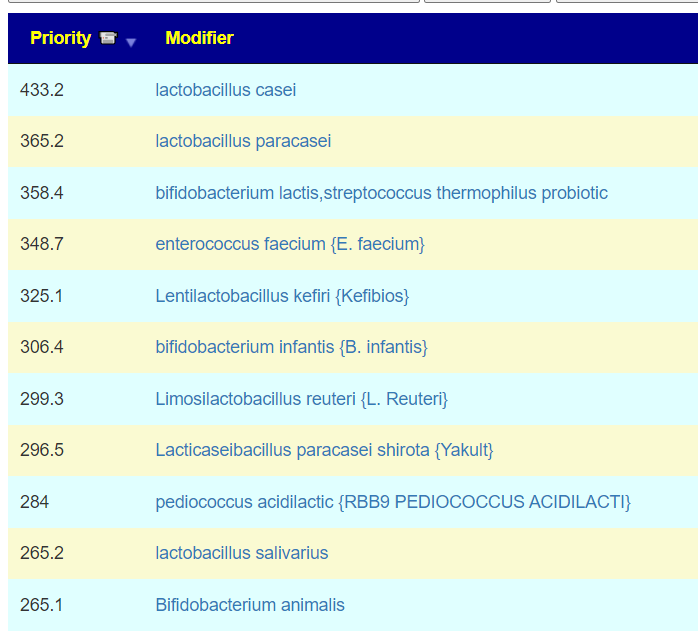
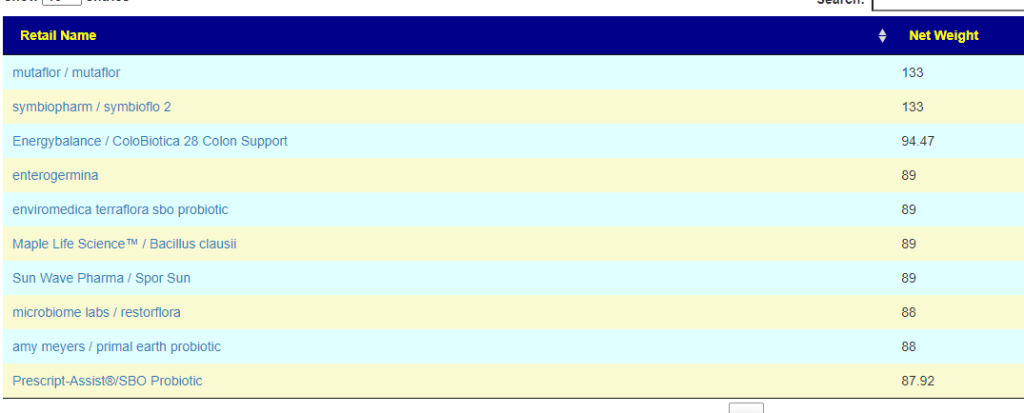
Probiotics are dominated with Bifidobacterium species. I would tend to do 3 weeks on one strain between antibiotics, working up to a dosage of 50 BFU. At present, my favorite source is Maple Life Science™: they ship worldwide, typically the packages arrive with manufacture dates 4-6 weeks before (thus LIVING probiotics), and very reasonable cost. Yakult and Kefibios can be difficult to obtain in some countries.
Going over to KEGG suggested probiotics and although we are approaching it from a totally different path, we have consensus.
- Top was L. Casei Probiotic Powder (aka Yakult above) [5.5]
- Maple Life Science™ / Bifidobacterium lactis [5.2]
- Maple Life Science™ / Bifidobacterium infantis [4.57]
- Maple Life Science™ / Lactobacillus reuteri [3.91]
- PIANETA FARMA/KefiBios [3.68]
For prebiotics, just three stand out, take them with the above probiotics
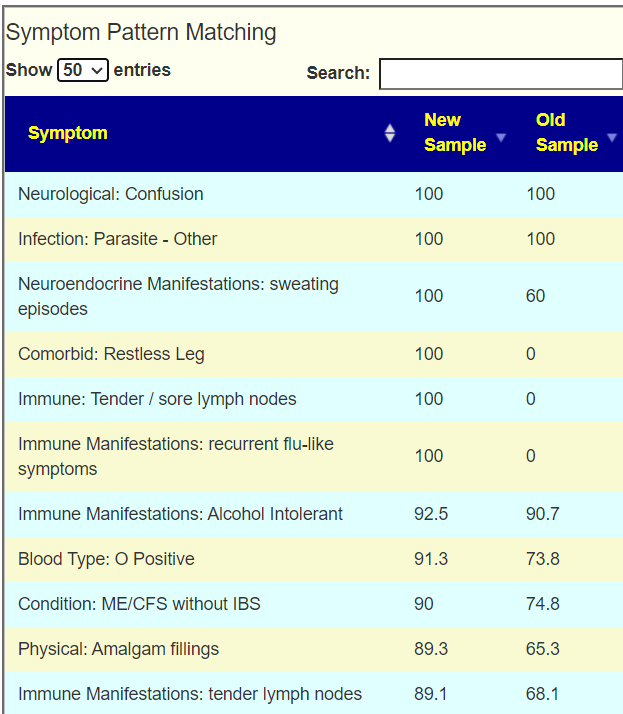
For vitamins (can be taken continuously), I would suggest adding them one at a time (every 3-4 days) in case some create significant (good or bad) reactions.
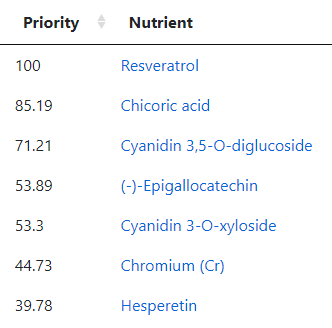
For flavonoids, the list is very ME/CFS typical.
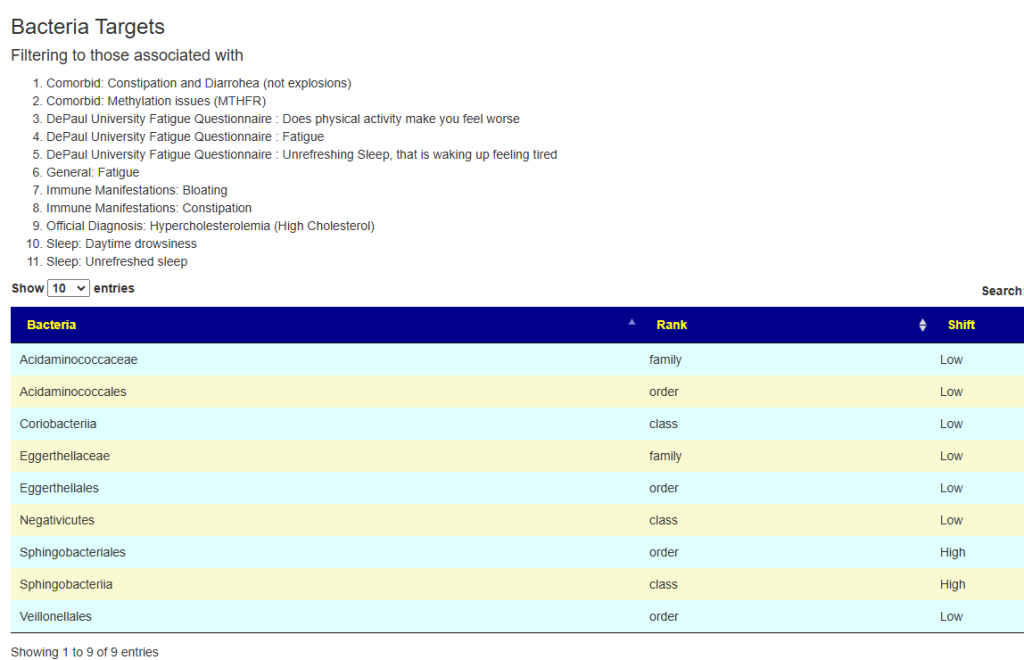
Second Pass – Cross Validated Suggestions
I picked these from the short list of options in the old UI.
The number of bacteria matches were relatively few.
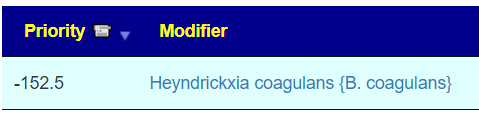
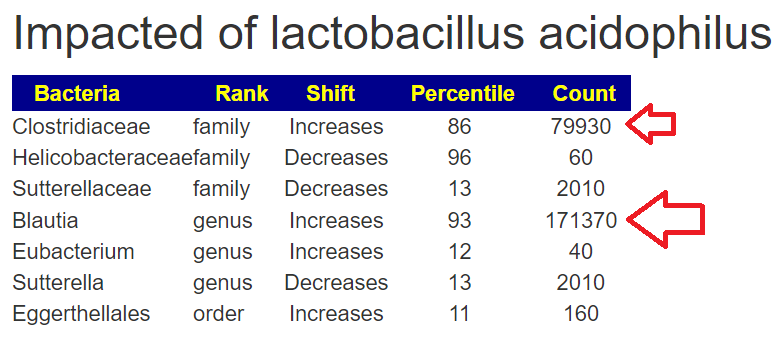
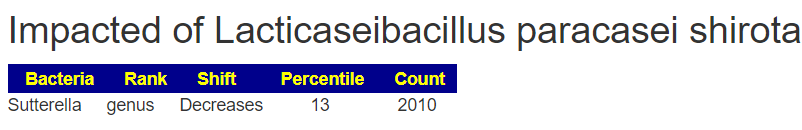
The suggestions are shown below. Note that Lacticaseibacillus casei and Lacticaseibacillus paracasei shirota. Are on this list, just as they were above. Avoid other lactobacillus probiotics.
Questions and Answers
Some questions:
— what are your thoughts on the sky-high levels of Bilophila (any specific advice on managing that?) and the very low overall species diversity. I did some troubleshooting with a CGM, and every time I eat some animal fat—and to a lesser extent, animal protein—after carbs, I experience a hyperglycemic spike. I attribute that and my brainfog to a Bilophila overgrowth (H2S & acetaldehyde). When I’m on a vegan diet, my blood sugar is generally perfect, except for one hypoglycemic event at night but it’s really problematic to sustain this diet long-term.
— also, which advice here is aimed at increasing lactobacillus abundance as the recommended probiotics are mostly bifido?
Response
Here we hit a philosophy crossroad.
- The road most travelled is focusing on the bacteria most heard about and trying to address them one by one.
- The road that I take is to ignore this chatter, and aim to adjust everything in one pass using mathematical models.
- Often I have read that something like Lactobacillus increases for a subset of people if other bacteria are present, (or absence).
- I view this approach is most likely to cause desired changes and not chasing this bacteria or that bacteria.
Microbial Interdependence
Microbial interdependence occurs when different bacterial species rely on each other for growth or survival. This can happen through various mechanisms:
- Metabolic cross-feeding: One species produces metabolites that another species uses for growth.
- Signaling interactions: Chemical signals from one species trigger responses in another.
- Modification of the environment: One species alters the local environment in ways that benefit another species.
Given that concentration is an issue, there is a high probability that high d-lactic acid is involved. This would cause me to suggest avoiding lactobacillus probiotics entirely. It is impossible to determine which retail brands produce d-lactic acid.
Bottom Line
Go slow, slowly increase dosages, keep track of your reactions on paper (or electronically). Some suggestions will have no effect, others may have dramatic effects.
Postscript and Reminder
As a statistician with relevant degrees and professional memberships, I present data and statistical models for evaluation by medical professionals. I am not a licensed medical practitioner and must adhere to strict laws regarding the appearance of practicing medicine. My work focuses on academic models and scientific language, particularly statistics. I cannot provide direct medical advice or tell individuals what to take or avoid.My analyses aim to inform about items that statistically show better odds of improving the microbiome. All suggestions should be reviewed by a qualified medical professional before implementation. The information provided describes my logic and thinking and is not intended as personal medical advice. Always consult with your knowledgeable healthcare provider.
Implementation Strategies
- Rotate bacteria inhibitors (antibiotics, herbs, probiotics) every 1-2 weeks
- Some herbs/spices are compatible with probiotics (e.g., Wormwood with Bifidobacteria)
- Verify dosages against reliable sources or research studies, not commercial product labels. This Dosages page may help.
- There are 3 suppliers of probiotics that I prefer: Custom Probiotics , Maple Life Science™, Bulk Probiotics: see Probiotics post for why
Professional Medical Review Recommended
Individual health conditions may make some suggestions inappropriate. Mind Mood Microbes outlines some of what her consultation service considers:
A comprehensive medical assessment should consider:
- Terrain-related data
- Signs of low stomach acid, pancreatic function, bile production, etc.
- Detailed health history
- Specific symptom characteristics (e.g., type and location of bloating)
- Potential underlying conditions (e.g., H-pylori, carbohydrate digestion issues)
- Individual susceptibility to specific probiotics
- Nature of symptoms (e.g., headache type – pressure, cluster, or migraine)
- Possible histamine issues
- Colon acidity levels
- SCFA production and acidification needs
A knowledgeable medical professional can help tailor recommendations to your specific health needs and conditions.



Recent Comments