For more Analysis Posts on Long COVID and ME/CFS click here.
Back Story
I’m male, 5’ 10”, currently 145 lbs, 60 years old. I first became ill suddenly in 1987, with what at the time seemed to be food poisoning or a stomach bug. The nausea, stomach upset and loss of appetite lasted months after, I became bedridden. Dozens of tests, doctors, revealed nothing.
Gradually over time, the symptoms subsided and I began to eat and gain weight again. After about a year and a half, I became functional, but never recovered to my previous state. This has been the course of life since. The symptoms would reoccur, last several months, then subside. With no definitive cause for beginning, nor treatment for ending.
The ongoing fatigue over the years was relentless. I somehow managed to complete a 30 year carrier, and took retirement at first opportunity. Doctors speculated that my work was a stress factor responsible for my condition, and retirement would solve it. It didn’t.
For the past several years, I’m mostly housebound, able to go outside and do minor tasks on occasion. Currently, my worst of symptoms are LPR/ reflux related. Not in the traditional sense, mine is a gas/ aero, that I believe is being caused by severe dysbiosis/ imbalance.
I cite this study as an example,
Accompanied with voice loss, throat and chest pain, severe at times.
A recent endoscopy showed “mild gastritis”. Doctors offer me benzodiazepines and antidepressants, stating my symptoms do not correlate with their findings.
Previous endoscopes/ colonoscopies were unremarkable. Gastric empty test normal.
I have tested negative for SIBO several times. IBS Smart test, h pylori, celiac, mast cell (MCAS), all negative.
Numerous diets, eliminations, supplements, herbs, prescribed medications have brought no help or relief. Most have made symptoms worse.
I did manage to have a biopsy taken and sent to Dr John Chia, to test for entero virus. It came back highly positive, however, I am somewhat skeptical that it could be a red herring. My vague attempts with pre/ probiotics resulted with increased gas and/ or diarrhea.
One clue, on two occasions (1995, 2014) after having colonoscopy, I mysteriously had remissions afterwards, that lasted several months. The speculation, is that the prep somehow created a reset of bacteria/ flora. I recently tried to replicate, by doing a prep cleanse. However, despite drinking a full gallon plus, I ran out of solution before being completely cleared out. I felt a brief improvement, but have suffered with horrid lower gas/ flatulence since.
Not the result I was after.
Initial Comments on Back Story
For myself, stress was the trigger of each of my ME/CFS episode so the speculation by his MDs was reasonable. The 1987 event, and the resulting cascade of the microbiome is the root concern. The microbiome evolves, just like society evolves. In 1987, most homes had a VCR and a few lucky people had digital pagers. Today, very few have VCRs (in use) and almost every one has a smart cellular phone. In 2023, arguing whether the right choice should be BetaMax or VHS has become irrelevant. Similarly, focusing on the cause in 1987 is really irrelevant. It may have been a virus, Lyme disease or a dozen other culprits – it is very unlikely to be relevant to addressing today’s microbiome.
Analysis
Looking at the distribution by frequency, we see an over-population of bacteria with low levels.
The Bacteria over 90% and Bacteria under 10% are a simple statistic to understand. If you have 188 different genus and true randomness then you would expect around 19 in each group. We has 12 over 90%, close, but a whopping 61 under 10% — that 32% of all bacteria, not 10%!!! In other words, we have a massive number of different bacteria at low levels. It is not a problem of a few bacteria being too high.
| Percentile | Genus | Species |
|---|---|---|
| 0 – 9 | 61 | 76 |
| 10 – 19 | 20 | 16 |
| 20 – 29 | 14 | 16 |
| 30 – 39 | 9 | 8 |
| 40 – 49 | 15 | 20 |
| 50 – 59 | 14 | 14 |
| 60 – 69 | 16 | 20 |
| 70 – 79 | 10 | 22 |
| 80 – 89 | 17 | 22 |
| 90 – 100 | 12 | 21 |
Looking at Dr. Jason Hawrelak Recommendations for levels, he was at the 99.7%ile and the very few misses for being ideal.. they were border line.. (i.e. 15.1 versus 15; 0 versus 0.0001). In short, almost an ideal microbiome by that criteria.
Going Forward
Doing the usual 3 suggestions sets, we
- Standard Lab Ranges (+/- 2 Std Dev) – 9 bacteria
- Box Plot Whisker – 43 bacteria
- Kaltoft-Moltrup Normal Ranges – 85 bacteria
The list of top suggestions look very close to what I was taking for my own remission (pre-microbiome analysis days).
- rosmarinus officinalis (rosemary)
- thyme (thymol, thyme oil)
- peppermint (spice, oil)
- lactobacillus paracasei (probiotics)
- lemongrass oil
- Human milk oligosaccharides (prebiotic, Holigos, Stachyose)
- neem
- syzygium aromaticum (clove)
- Sumac(Rhus coriaria)
- cinnamon (oil. spice)
- Ajwain (trachyspermum ammi)
- Curcumin
- lactobacillus casei (probiotics)
- thiamine hydrochloride (vitamin B1)
- aloe vera
- ashwagandha (withania somnifera)
- garlic (allium sativum)
- olea europaea (olive leaf)
Looking at the to-avoid
- vsl#3 (probiotics)
- walnuts
- lactulose
- amaranth
- barley, oat
- arabinoxylan oligosaccharides (prebiotic)
- fish oil
- saccharomyces cerevisiae (probiotics)
- low protein diet : typically seen when B-vitamins are wanted.
The full details are below
Going over to the Food Site we see:
- Chicken and Turkey Liver being at the top of the list
| mg per 100 grams | Significant amount | Nutrient |
|---|---|---|
| 25800 | Significant | Protein |
| 13.925 | Significant | Niacin |
| 12.9 | Significant | Iron, Fe |
| 4.293 | Significant | Retinol |
| 2.313 | Significant | Riboflavin |
| 0.84 | Significant | Pyridoxine (Vitamin B6 |
| 0.56 | Significant | Folic acid |
| 0.02113 | Significant | Vitamin B-12 |
Pass 2 — Looking at Prescription items
One non-prescription showed up near the top, an item that I have used with good effect: monolaurin. The top antibiotics list include:
- piperacillin-tazobactam (antibiotic)s [Penicillin]
- benzylpenicillin sodium (antibiotic) [Penicillin G]
- hyoscyamine (l),(prescription) – “It can treat muscle cramps in the bowels or bladder. it can treat symptoms of irritable bowel syndrome (IBS), colitis, and other digestive problems.” [Src]
- minocycline (antibiotic)s [Tetracycline] – used by many ME/CFS physician, and also by me. It has many good characteristics (neuroprotective, cross body-brain barrier, etc)
- tobramycin (antibiotic)s – usually only used for eye infections
- ampicillin (antibiotic)s [Penicillin]
The above have various risks, and should be review carefully. My own preferences would be minocycline first, then hyoscyamine [because IBS is a factor for this patient]. I should note that using a different algorithm without consensus (Special Reports for your MDs) reports contrary results.
Feedback on Antibiotics
Another freak incident that resulted in a five month remission. In 2011, I had one tonsil that became huge. The other remained completely normal. Doctors were suspect of cancer, and both were removed. Thankfully, it was not cancer. So they didn’t look any further to determine the cause.
But at 49 year old, this was no picnic. Rough surgery and recovery, but it followed with probably the most significant remission of all. It was an amazing turn around, all symptoms backed off, energy returned to nearly normal. After 5 months though, symptoms began to return, and within the year I was back to my previous state
I was on amoxicillin for several weeks after the surgery. When the symptoms began to return, we became suspect that it was the amoxicillin that had done something. My doctor put me back on it, but there was no improvement. Whatever had taken place, was a random-chance occurrence. Maybe the amoxicillin was responsible, by creating a shift in bacteria balance.
I found that Cecil Jadin’s protocol is what I tend to advocate. One of the key reason is that it was it was tuned from many years of clinical experience at the Pasteur Institute for Tropical Medicine for what they termed as an “Occult Rickettsia” infection. The basis of it is rotating different families of antibiotics. The mathematics are simple — first round may eliminate 90% of the issues with 10% being resistant. A different antibiotic usually require a different type of resistance, so 90% of the remaining 10% is eliminated.. leaving just 1%. Doing a third round, takes us down to 0.1%
I speculate that the few survivors from your first round of amoxicillin slowly rebuild . Because these bacteria were the survivors, those with resistance genes. The repopulated gut was largely resistant, hence no effect from this antibiotic later. Think of it as a boxing match. You landed a good punch — but instead of landing more punches, the opponent was able to recover and block the same punch later.
Later, discussion of this story with a well-meaning gastrologist, he had me do a week of xifaxan. He felt certain, based on my story, it would get me back to the previous gains. It made me horrid sick, lasting for weeks after stopping it. There was no improvement.
My preference is not to pick antibiotics by symptoms (or what worked for the prior patient), but from the bacteria results that are desired. Results are not guaranteed — rather, IMHO this approach has higher probability of being successful.
Looking at Probiotics
First, using KEGG data: as is typical for most ME/CFS people (and consistent with the ME/CFS conference reports from 1998): Escherichia coli (Symbioflor-2 or Mutaflor). The next common one is Bacillus subtilis (natto), Clostridium butyricum, Lacticaseibacillus casei, Enterococcus faecalis.
From the consensus list we see a good overlap and have in order:
- lactobacillus paracasei (probiotics)
- lactobacillus casei (probiotics)
- lactobacillus casei shirota (probiotics) – Yakult
- bacillus subtilis natto (probiotics)
- symbioflor 2 e.coli probiotics
bacillus subtilis natto is the source for a supplement called nattokinase, which dissolves fibrin deposits and also an anti-inflammatory [2021]. It is also available not as a probiotic, but in a Japanese Dessert Food called Natto. Natto is an acquired taste.

My probiotic suggestions would be the following (at sufficient dosage, see this page):
- 2 weeks of Bacillus subtilis (perhaps 10 BCFU daily)
- 2 weeks of lactobacillus casei (perhaps 48 BCFU daily)
- 2 weeks of one of the E.Coli probiotics (Mutaflor: 4 capsules per day, starting at 1 and slowly increasing)
Then repeat. Note that some probiotics are strong avoid, for example: saccharomyces cerevisiae / saccharomyces boulardii.
Taking Herbs
There are a large number of herbs cited above. In keeping with my philosophy of avoiding resistance, take some of herbs for 2 weeks and then change to others herbs for the next two weeks. The question is how to take it? I know that some will claim that tinctures are more effective; IMHO, tinctures are very effective for reducing back accounts!
My personal practice is to take herbs in one of two ways:
- Buying them in bulk, organic and making our own 000 capsules. Most store purchased herb capsules do not appear to be organic, often with additional ingredients “to make them better” – which is often marketing hype.
- We take them immediately prior to meals so that the stomach acid produced to handle the meal, also dissolves the active ingredients from the herbs.
- Taking them as a hot tea. Some herbs are horrible tasting… those tend to end up as capsules.
Many, but not all, herbs have documented dosages with links to studies (which can be informative for how to take). For example: Neem: 120 mg/day, Olive Leaf: 700 mg/day, Curcumin: 3 gm/day. My general rule of thumb is one 000 capsule with each meal.
Questions
Q: Curious to know, do you think there may be an advantage of using this method with probiotics, to deliver past the stomach, farther down the gut?
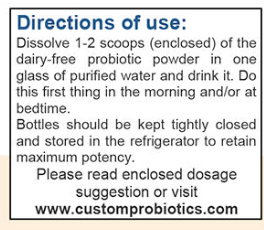
A: I know this common belief, but have not seen any clinical studies demonstrating it. What I have seen is probiotics delivered as a liquid in water, are documented to persist for weeks after a single dose. That is, the specific strain delivered was not detected before but was detected in subsequent weeks. This indicates that this belief is very questionable. Personally, I tend to use single documented strains of probiotics from Custom Probiotics and follow their directions. I do keep food at least a hour away from taking probiotics so stomach acid production will be quiet.
On a related issue, remember that the gut is downstream from the mouth and nasal passages. The source of bad bacteria may be there and may account for repopulation over time. One probiotic that has been shown effective for the nasal passages etc is Symbioflor-1. There are a few hard tablet probiotics out there (for example, Miyarisan — Clostridium butyricum). I have often just put them in my mouth and let them dissolve there.

NOTE: I will be doing a follow up post on The oral microbiome, coming soon!
I have crohns/ colitis please can you recommend which probiotic?
Thank you
The best one is Mutaflor (E.Coli Nissle 1917) which has been used for over a century. I know people who have not needed to take any prescription drugs by using it, with their GI shaking their head over the stabilization from
it. I would expect similar benefits from the lower dosage sister, Sympbioflor-2
For other items see this researched list/ #2 choice would be Lactobacillus rhamnosus GG (Culturelle)
Interesting article. I have no health issues and take no meds. A few random observations from my perspective. I saw fish oil as an “avoid”. Fish oil is poorly handled in the marketing chain and readily oxidized to become somewhat toxic/disruptive. I have come to a conclusion that just about all of society consumes too many processed small seed oils as poly unsaturated fatty acids (PUFA’s) and this skews omega 6:3 fatty acid ratios way out of whack from an optimum ratio of 2.5:1. Most people would be more than 15:1! Answer is reduce consumption of PUFAs usually in processed and restaurant foods and increase omega 3 FAs by eating regeneratively grown animal products and well-handled pure algae-based supplements. As every cell in our body has a fatty acid cell wall and omega 6 overload here slows nutrient uptake and waste removal as well as downregulate mitochondria activity, I suspect this is the most influential process in human health outcomes today. The next thing is plant foods high in lectins and oxalates (gut irritants) often need strategic processing for long term health. We were never meant to try to digest plant cellulose. Food for thought! My name is René.
Many thanks for your feedback. The analysis was not done from a general holistic health perspective but with a specific goal of altering the outliers in his microbiome sample towards more normal value.
it is very VERY person specific and not a ‘general health’ analysis. All based on published studies on the US National Library of Medicine.
When I look at my percentiles, I have a group 100-109. Could you help me to understand this?
0 – 9 19 23
10 – 19 24 21
20 – 29 28 30
30 – 39 15 18
40 – 49 17 19
50 – 59 17 23
60 – 69 15 12
70 – 79 8 14
80 – 89 7 6
90 – 99 11 8
100-109 3 3
The 100-109 actually means just 100, three items were higher then any numbers seen before. I need to fixe that.
The issue has been fixed. Thank you for reporting it