A reader emails as shown below. The deep vein thrombosis (DVT) aspect interest me because it is typically associated with inherited coagulation defects (an interest that I have), although actual DVT has not been an interest (when I flew regularly, I was prescribed heparin and took it with piracetam (good for my specific defect).
On 15 July 2021 I uploaded my first Thryve sample to your website. Prior to that sample I had a few Ubiome samples from a few years ago. Thryve seems to detect many more bacteria than Ubiome.
My results seem particularly unusual with numerous rare bacteria unfortunately. My main symptoms have always been constipation, food allergies and 2 episodes of DVT whereby I remain on anticoag therapy to avoid further recurrences.
Bacteroides Vulgatus seems to be significantly high in all of my test results, both Ubiome and Thryve. I wonder whether this could be the ‘root cause’ given that the numbers of it are so much higher than any other bacteria.
What is known about DVT and Microbiome?
After a while searching PubMed, I finally found a 2020 article. Of special interest is Staphylococcus aureus which appears to have a significant role with ME/CFS [2016 Post] and may account for the high percentage of hypercoagulation seen there.
” Many known bacteria, such as Helicobacter pylori, Chlamydia pneumoniae, Mycoplasma pneumoniae, Haemophilus influenzae, Streptococcus pneumoniae, Staphylococcus aureus, and Escherichia coli, causing infections may increase the risk of thrombotic complications through platelet activation or may lead to an inflammatory reaction involving the fibrinolytic system.” Microbial Modulation of Coagulation Disorders in Venous Thromboembolism [2020]
A fuller list from the full article (Citing 2019) is, below
- Staphylococcus aureus,
- Streptococcus pyogenes
- Pseudomonas aeruginosa,
- Escherichia coli,
- Klebsiella pneumoniae,
- Chlamydia pneumoniae,
- Helicobacter pylori,
- Haemophilus influenzae
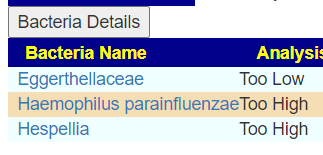
Looking at samples over three year, we have a strong candidate for causing DVT, Haemophilus parainfluenzae. It is consistently very high. Blank indicated no reported value.
| Bacteria | 21-07-15 | 19-06-15 | 18-12-19 | 18-08-13 |
| Staphylococcus aureus | ||||
| Streptococcus pyogenes | 71% for Streptococcus (most not classified) | |||
| Pseudomonas aeruginosa | ||||
| Escherichia coli | ||||
| Klebsiella pneumoniae | ||||
| Chlamydia pneumoniae | ||||
| Helicobacter pylori | ||||
| Haemophilus influenzae/ Haemophilus parainfluenzae | 94.6%ile | 89%ile | 91.2%ile | 95.8%ile |
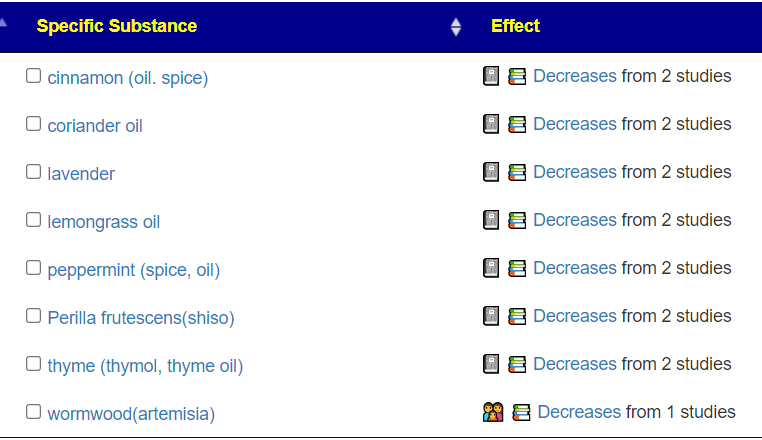
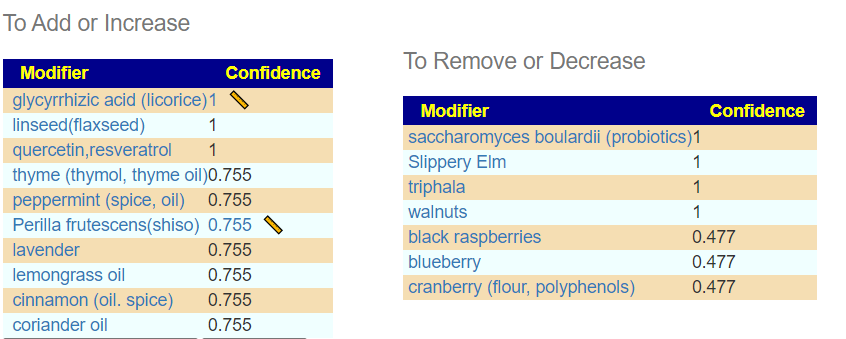
Checking the microbiome prescription summary for this bacteria, we see a short list of herbs impacting it (there is bigger list of antibiotics)
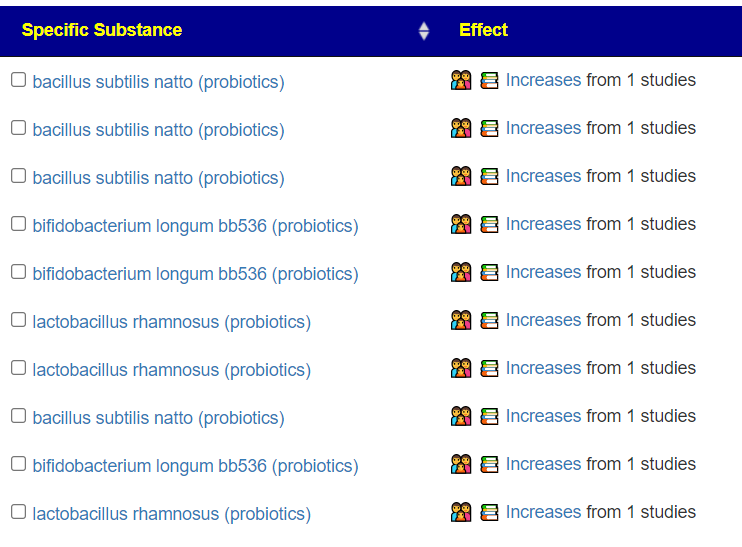
Almost every probiotics encourages it. PPI, ku ding cha tea also increases t.
Other items reported to decrease it are:
Personally, I would address this as #1 item.
Constipation
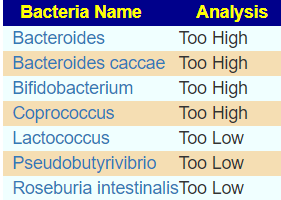
Using the Nat.Library of Medicine filter for constipation and relaxing to include high and low 12%, we came up with only a very short list of candidates. Using Kaltoft-Møldrup bounds, nothing was selected.
As for allergies, “Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis are often involved in respiratory infections associated with wheezing, but there is no evidence for their active role in asthma pathogenesis or exacerbation. ” [2009]
Running Advance Suggestions “as Is”
The key items selected reflects our analysis above:
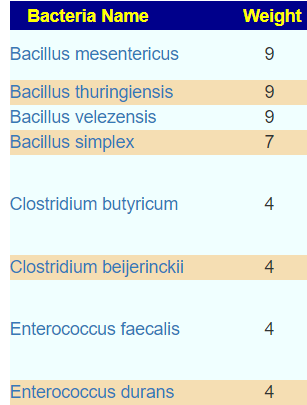
KEGG Suggested Probiotics
The numbers are low, indicating no major issues. None of the suggestions are known to increase (or decrease) our focus. For supplements, it is similar
- beta-alanine
- NADH
Bottom Line
The primary question from the user appears to be answered. I would suggest fixing the Haemophilus parainfluenzae in isolation from the other two issues. Those two issues resolution will likely tend towards the use of probiotics — which are counter indicated with Haemophilus parainfluenzae. You have to prioritize issues and be careful not to send mix messages to the microbiome.
As always, review and consult with your medical professional before implementing
Recent Comments