This email arrived and contributed in two changes:
- Warning on using Special Studies — suggestions can be erratic and should not be used if they conflict with the usual consensus building algorithms.
- Adding Modelled Food Suggestions — this should also partially address some challenges doing suggestions in Japan
Back Story
Love your work, I have read many of your posts on CFSremission, and based on that and my own research I think your microbiome-based view of ME/CFS is generally correct.
I have been suffering from cfs since 2009, I did a study abroad in South Korea and had a weird fever there, after that I got tired easily, often felt light-headed, head felt hot, but I was able to mostly live a normal life and actually spent a lot of time in the gym. (I think this supports the microbiome theory, my diet changed radically when I went to Korea)
I dealt with the fatigue with regular consumption of coffee/tea throughout the day, often going out drinking at night. I also used to lift weights in the gym almost every day. Full body lifts like squats, deadlifts, etc. During this time I drank about a quart of milk a day as part of my bodybuilding routine. My sleep always seemed unrefreshing.
Then in late 2019 I got sick with a EBV/Mono-type illness, swollen lymph nodes and tonsils, crushing fatigue, sore throat, that lasted a month. Sore throat resolved, but the tonsils were still a bit swollen and the lymph nodes got smaller but seemed to be permanently hard. I thought I might have thyroid issues or cancer, but multiple screenings ruled that out.
I tried multiple times to go back to the gym, but my workouts were poor and I got hit with what I now understand to be PEM the next day. Eventually I had to stop trying to exercise. I’ve tried various supplements such as methyl-b12, doses of tumeric or curcumin, too many to count, then I discovered your website. I think it lines up with my experience and is a good model to explain the so-called “anomalous” way that some treatments work for some CFS sufferers and not for others.
So I am writing this email to you now hoping I can get some insight. I have read your blog posts about other CFS sufferers analyzing their samples, so I hope you could take a look at mine as well. Feel free to use this or parts of it as a blog post, but don’t use my name or email address obviously.
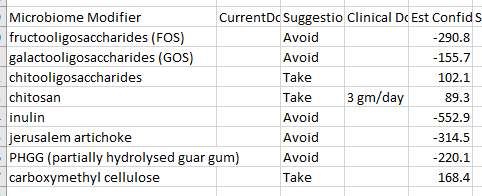
Some background, I had to get a sample manually added from a lab here in japan, based on those suggestions I took two rounds of miyarisan, (I live in Japan, so it was the most easily obtained of the probiotics suggested) as well as added lots of inulin, oats, whole grains etc. to my diet. Similar to some of your other posts, including the suggestions to avoid Vitamin B supplements (the greedy bacteria taking the B-vitamins!) But, I feel like it made me worse. These days my legs are very heavy and tired.
I had another sample taken between the two rounds of miyarisan which i sent to Biomesight (a much better choice.) It took over a month for the results to get back. When they came back, it suggested a totally different course, putting miyarisan and inulin into the strong-avoid category! With the inulin+oats+miyarisan diet, I am more tired and my libido dropped a lot.
So I made a new analysis based on the national and special studies for unrefreshing sleep, ME/CFS without IBS, cold intolerance, general fatigue, etc.
1. As attached, it suggests “alcoholic beverages” pretty high. How should I interpret this? Beer? Wine? Vodka shots every evening? Is there more context for this?
2. Not many foods with any strong suggestions, what can I eat realistically (here in Japan) off this list of suggestions? It suggests a milk diet, but whole milk is not suggested? Seems to have a lot of contradictory suggestions.
3. I decided to go with national + special studies, but the “general consensus” is totally different. I assume the studies are better for my condition?
Feel free to look at the data of both of my samples, or offer a different way of getting a consensus, I really need some guidance here!
Regards,
From a reader (with permission to post)
Initial Impressions
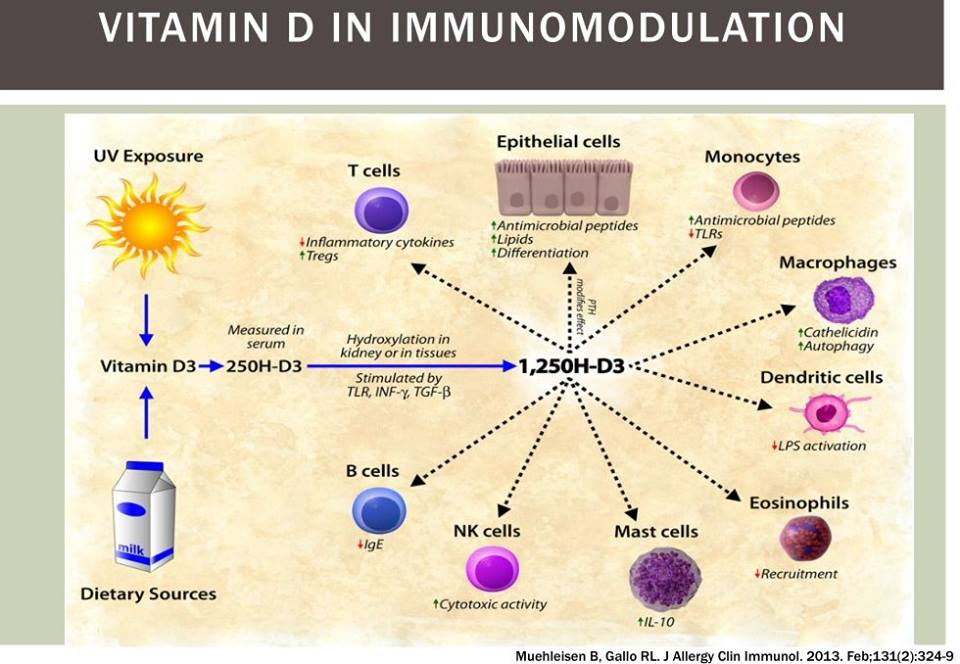
- “EBV/Mono-type illness” — EBV, HHV5 and other virus in CFS gives context, but this post, Viral Reactivation and the Microbiome gives context and cites “For EBV, viral load was significantly higher when 25(OH)D levels were low, demonstrating an inverse correlation between 25(OH)D levels and EBV load. ” [2018]. My first step would be to get 25D levels measures (likely low) and 1,25D levels (likely very high). It’s an easy issue to address with Vitamin D3 supplements (likely 20,000 IU/Day may be needed. See the following for more information
- Vitamin 25D and 1,25D measure – one reduces symptoms and one indicates CFS state
- In the past I cited Cholecalciferol loading dose guideline for vitamin D-deficient adults [2010], Vitamin D oral intermittent treatment (DO IT) study, a randomized clinical trial with individual loading regimen [2021] .. but there is an online calculator: NEW Loading Dose Vitamin D*Calculator!
- My suggestion [2016] for target level is: 90-100 ng/mL (200-250 nmol/L). (of course, to be discussed with your medical professional)
The Key Problem with Suggestions is the picking of bacteria
Suggestions are based on several main factors:
- The bacteria you decide to alter (i.e. increase or decrease)
- The importance of each (sometimes called weight) when there is a trade off
- What substances has had any research. This is a nightmare – between contradictory results, small sample sizes, study done in the context of a specific diseases, etc. This is why I use fuzzy logic.
With the above stated, I walked thru this sample trying to first improve the bacteria selected (using my experience and statistical understanding), and then looking at the suggestions they generate.
This issue can be compounded with the depth of bacteria reported. “The disease is in the small details”. This is why more detailed and comprehensive (i.e. number of bacteria types reported) tests are a better starting point.
Contradictory Suggestions root issue
Facts in the database are based on what is specified in the study. A simple example: one study may use turmeric and a different study used curcumin. Curcumin(diferuloylmethane) is a main component of turmeric, but it also contains two other compounds demethoxycurcumin, and bisdemethoxycurcumin. In addition, volatile oils (tumerone, atlantone, and zingiberene) [Antiinflammatory Herbal Supplements, 2019]. The studies may result in a bacteria increasing in one and decreasing in the other. Both are right! It is the additional components that are significant. The worst case of “fuzziness” is with anything that has the word “diet”. Many people offering advice will deem them to be the same to simplify the facts that they need to remember; Dr. A.I. does not need to simplify — but that comes at a cost of confusion when things seem similar at a high level to the user. Another example: lactate, lactose, versus milk.
Analysis
Going to the My Profile / Health Analysis page, we see the two items that where he is at highest percentile (98%ile and 99%ile) are related and would agree with unrefreshing sleep.
- Sleep Apnea
- Insomnia
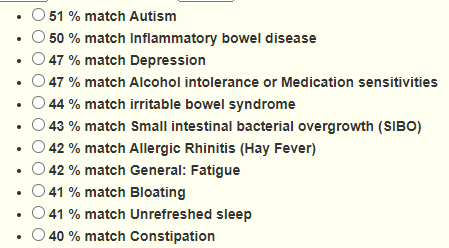
ADHD is high, but that seems common with ME/CFS. Dr. Jason Hawrelak Recommendations come in at the 89%ile. Going over to special studies, we see a lot of matches. The matches are not predictive — there are other factors (like DNA/SNP) before symptoms appear. They indicate simply increased risk.
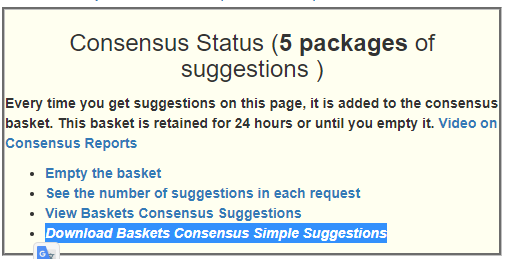
Strategy to build Consensus
The two PubMed profiles above, Standard Lab Ranges (+/- 2 Std Dev), Box Plot Whisker, and Kaltoft-Moltrup Normal Ranges gives 5 sets of suggestions. This will be my base set. I will also look at some special studies results (comparing those suggestions to
Simplified Suggestions
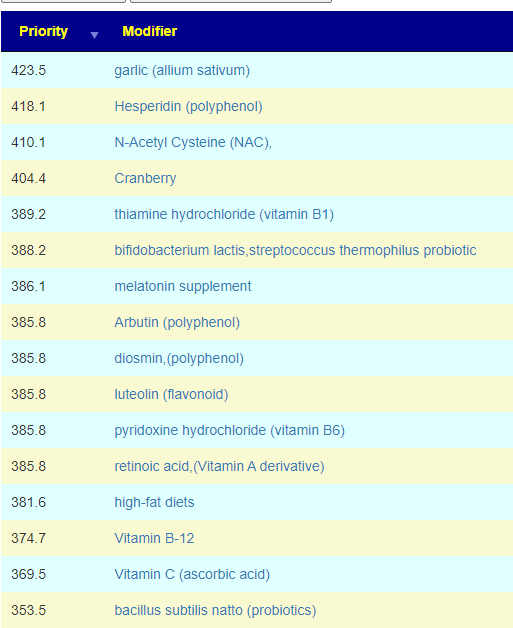
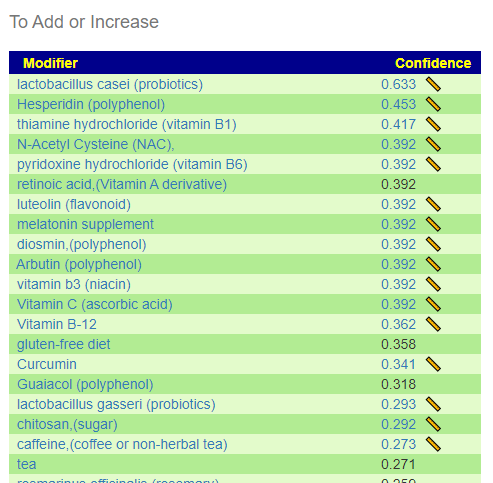
The majority of probiotics are to be avoided (not unusual for ME/CFS). The top suggestion was lactobacillus casei which is an easy one to get in Japan. The well studied one is sold as Yakult. The next ones are: lactobacillus gasseri, bifidobacterium breve. With most of the probiotics being negatives, you do not want to get them in probiotic mixtures.
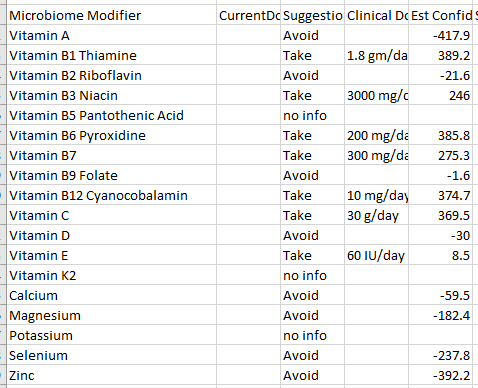
In terms of vitamins, we see most of the B-vitamins are suggested (this is seen in one subset of ME/CFS patients, a different subset has it as an avoid). Vitamin D is a very mild avoid — but given the EBV issue above, I would ignore it and make that judgement call based on blood tests.
This also may apply to B-vitamins — none of the B vitamins are strong avoid, so a B-Complex is fine.
I have filtered the rest of the list to only the to take, coffee is sitting high in the list which appears to agree with “I dealt with the fatigue with regular consumption of coffee/tea throughout the day“. It helps in additional ways on shifting the microbiome.
| Garlic | Take | 4 gm/day | 423.5 | |
| Hesperidin | Take | 1.5 gm/day | 418.1 | |
| NAC | Take | 2400 mg/day | 410.1 | |
| Melatonin | Take | 10 mg/day | 386.1 | |
| Luteolin | Take | 400 mg/day | 385.8 | |
| Coffee or non-herbal tea | Take | 4+ Cups/day | 313.4 | |
| Curcumin | Take | 3 gm/day | 239.2 | |
| Baicalin | Take | 123 | ||
| Glycine | Take | 15 gm/day | 119 | |
| Echinacea | Take | 4 gm/day | 109.5 | |
| Bilberry fruit extract | Take | 40 g/day Vaccinium myrtillus powder | 109.5 | |
| Piperine | Take | 109.5 | ||
| Tea Tree oil | Take | 109.5 | ||
| Fisetin | Take | 20 mg/day | 99 | |
| Polyphenols | Take | 3 gm/day | 95.3 | |
| Raspberry fruit (black raspberry) | Take | 50 gm/day | 61.5 | |
| Walnut | Take | 75 gm/day | 30.5 | |
| Olive leaf extract | Take | 700 mg/day | 24 |
Looking at the details of the Consensus Report
There are a few items not in the simplified list that are worth calling out:
- bacillus subtilis natto (probiotics) – is in the Japanese desert food called Natto. (it is a bit of an acquired taste [I have acquired that taste] and usually found only in some Asian markets in the US). Nattokinease is an extract from it.
- melatonin supplement – which goes with the sleep issues cited above.
- ascophyllum nodosum (sea weed) — various sea weeds are used in traditional Japanese cuisine.
Comparing Suggestions from PubMed Studies
- Insomnia — only 3 bacteria matched
- Sleep Apnea – only 3 bacteria matched
- ME/CFS without IBS – 7 bacteria matched – We get good agreement with the above
Comparing Suggestions from Special Studies
As a result of this email (and several others received this week), I looked at Special Studies suggestions for some specific people. My expectation when I did special studies was that the suggestions would converge tighter — so some people that is true. For other people, like this person is it false. For more information read the blog post: Caution: Special Studies Suggestions
I noticed that most of the results had inulin, etc – which are to avoid above and appears to make the person worse.
- Chronic Fatigue Syndrome (CFS/ME) – 52 bacteria some agreements and some disagreements
- Unrefreshed Sleep — 62 bacteria matched
- ME/CFS without IBS – 94 bacteria matched
I will be using this person sample to experiment with revised algorithms for Special Studies.
Probiotics
The top probiotic from KEGG data are E.Coli probiotics. Both Mutaflor and Symbioflor-2 (commercial E.Coli probiotics) are on the to take consensus list.
The next usually available item on the KEGG list is Bacillus subtilis, followed by Bacillus subtilis subsp. natto. As cited above, Natto is easily available in Japan.
Looking at Modelled Food Suggestions
Looking at the Flavonoids, we see just two things: Bananas and Barley. Rice is on the slight avoid (which may be a challenge for Japan).
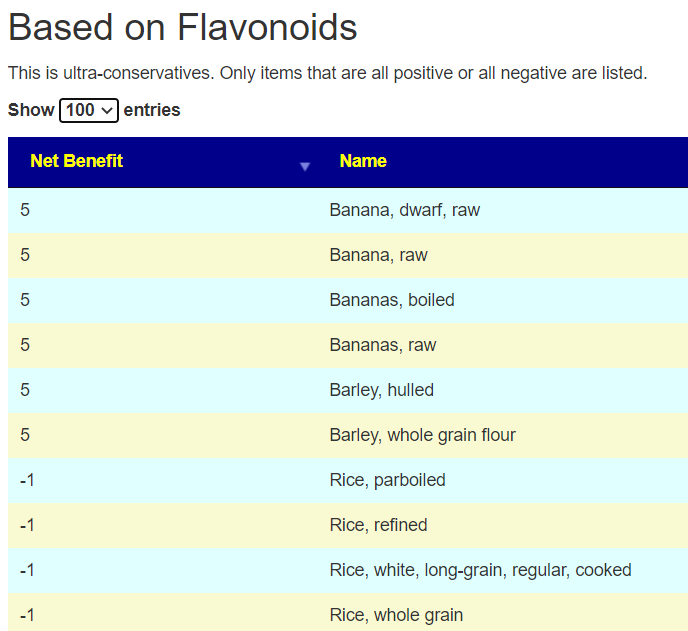
We do not fair much better with Food Contents 🙁 A Guide to the Different Types of Tofu in Japanese Cuisine
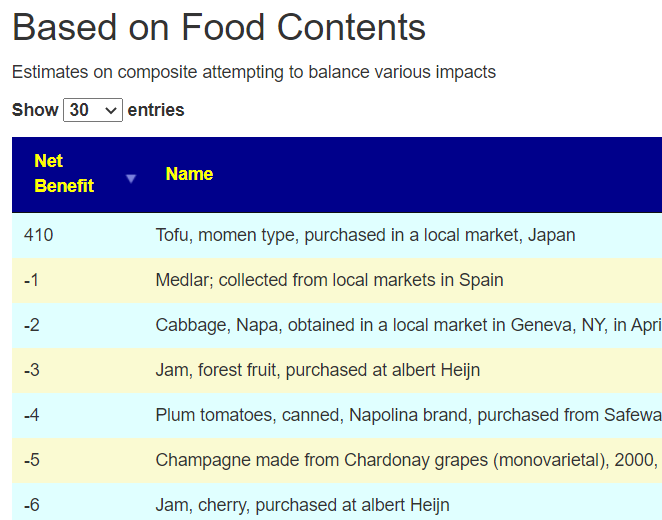
This was an unexpected frustration. I wait back to the algorithm and made it less conservative. By this I mean, not eliminating items where there are contradictory results from studies. This resulted in in more suggestions, some Japan specific [there are 50 items acquired in Japan on the list]
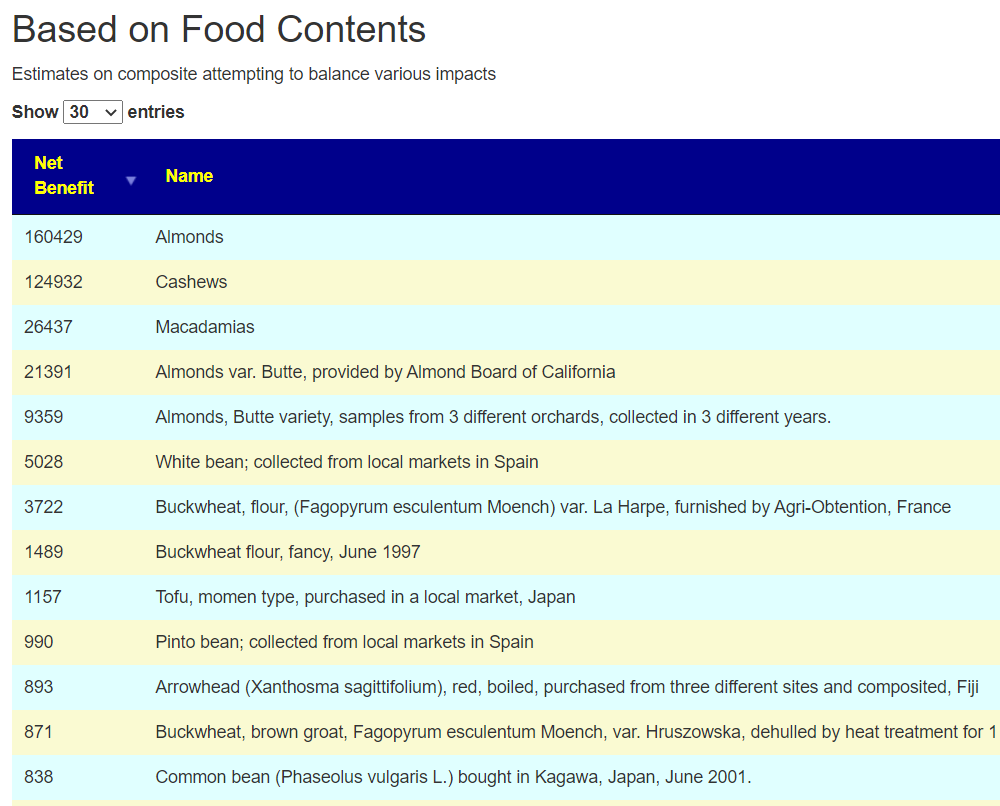
I was going to leave the algorithm with the more relaxed condition. I then did cross-validation with the consensus and found that most of the items appearing as take using the relaxed filter were on the avoid list of the consensus. Tofu, which showed up with the strict criteria, is on the consensus to take list (as in Soy).
Why do we have any disagreements? The root problem is not sufficient studies – often with contradictory results — one may be on people with diabetes and another people with asthma. Existing conditions (and in some cases severity) can result in difference response. The microbiome is not a machine but a complex society that interacts with a lot of things
The Hail Mary Exploration
I redid the consensus and included prescription items. For many people, the pharmaceuticals are way down the to take list. Herbs and probiotic having a higher positive weight often. For this person, this was not the case. What was also unusual was none of the antibiotics that are recommended in other ME/CFS analysis (and which are used for ME/CFS – i.e. cross validation) are anywhere near the top of the list. What I found listed near the top of the pharmaceuticals were:
- atorvastatin (prescription) – treats treat high cholesterol and triglyceride levels.
- clemizole hydrochloride,(prescription) – used for treating Hepatitis
- sertaconazole nitrate,(prescription) – an antifungal
My immediate, due diligence, suggestion is to get testing for cholesterol, hepatitis and fungal infections. Was the “EBV/Mono-type illness” perhaps hepatitis? Two of these can result in chronic fatigue. In terms of special studies, ME/CFS (three variations) were poor matches (one was the bottom of the list). Using US National Library of Medicine studies, he is at the 29%ile.
What I find interesting is that soy is a recommendation, and we find these studies..
- Effect of soy protein supplementation in patients with chronic hepatitis C: a randomized clinical trial [2012] – positive effect
- Inhibitory effect of Japanese rice-koji miso extracts on hepatitis A virus replication … 2018
In terms of having the typical microbiome for someone that has a ME/CFS diagnosis — he does not match. He is also at the 0%ile for hypercholesterolemia (High Cholesterol), 8%ile for GERDs (usually common for a subset of ME/CFS).
My gut feeling is that he was not sufficiently tested before the ME/CFS label was slapped on him. His microbiome is not a match. Nothing match his symptoms to the microbiome associated conditions that I have data on.
FEEDBACK FROM READER AFTER READING
Those are very interesting points. Since my initial symptoms in Korea, I was diagnosed with Gilbert’s syndrome, an excess of Bilburin. I did get my liver checked (due to slight yellowing of the eyes) out but they don’t seem to have found anything (Over a decade ago so my memory is pretty spotty.) I think over the years in college I got MRI’s and various bloodtests with obviously no real diagnosis. Even so, my life was very active over that decade. I lived in China for a few years, frequently attended the gym, also did a fair share of partying, have always had a big appetite. Minimal impairment throughout my life overall.
Since getting sick a few years ago in Japan, I got a lot of different tests, including thyroid and diabeties. If I rifle through all the different result sheets (I have quite a few), a few things of note:
Dec. 2020 I was positive for EBVVCA-IgG which my doctor told me meant that I had had EBV in fairly recent past. No treatment was suggested.
Feb.. 2020 I had slightly elevated liver enzymes (ALT, GTP) (Not surprising given my frequent social drinking in my 20s) which persisted until April 2021 and seemed to have resolved. This was explained by lowered alcohol consumption. Never received a suggestion for follow-up or differential diagnosis.
Persistently higher tryclycerides (I have gained some weight since my illness, matches with the atorvastatin suggestion!) and CRP indicating inflammation. Suggested to lose weight and exercise (The latter being somewhat problematic for me.) Back in my weight-lifting days, I drank lots of milk and overall had a high-fat/protein diet. Since I recently stopped drinking so much whole milk, I wonder if that will resolve it or not.
Before I moved recently I had been going to a cfs clinic which conducted sleep studies (of which I have had several over the years, indicating that I do not have sleep apnea, although that was my thought for years.) and did some other tests indicating I had high stress/inflammation. He gave me vitamins, CoQ10 (which I ordered myself) and anti-depressants for sleep. (Interesting I score high for Depression (47%) but up until the last few years I had a very active lifestyle, I don’t think depression fits my physical symptoms at all. I’ve always been very social and generally on the adventurous side. Still am, just don’t have the physical stamina I used to. I requested a prescription for Piracetam (all of the -tams were recently regulated in Japan) and he refused.
I haven’t gone back there since as I felt like the approach he had was very symptoms based and surface level. Reading your recovery stories, I pretty much ruled out getting any kind of prescription anti-biotics or being able to utilize those out here. I don’t know how the legal system works here in Japan, but my own and other anecdotal experience tells me that doctors here don’t enjoy doing things off-label, it’s an extremely by-the-book conservative approach to medicine. Fortunately, if you have a specific, known medical problem, you can get extremely professional and competent care here.
It is very interesting that I do not fit in the ME/CFS microbiome profile. An infection with Hepatitis or a fungus at some point could fit, especially given that I’ve spent time in a variety of different environments. I think I could easily get tested for Hepatitis here, it will just have to wait until next month (Currently very busy as a **** .) As far as fungus goes, usually I hear about “Candida,” any suggestions of what kind of fungus I should perhaps be looking out for would be helpful.
I will have to think about how I will go about getting tested for fungal infections here, it is somewhat difficult to explain my issues to doctors and get them to take it seriously. Definitely a good idea to also pursue a potential alternative diagnosis though, the data certainly doesn’t rule it out.
You have given me a lot to think about, thanks again for all of your consideration!
Postscript – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I cannot tell people what they should take or not take. I can inform people items that appears to have better odds of improving their microbiome as a results on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting.
I use modelling and various mathematical technique to estimate forecasts when there is no hard data available.
Recent Comments