We have a varied history with some storms blowing us off courses. Here’s a list of the tests and prior blog posts:
- 2018: Irritable Bowel Syndrome (IBS) diagnosis
- 2021-11-18 – IBS + BioNTech COVID Vaccine -> ME/CFS? [Jan 6,2022]
- 2022-05-20 – Follow up Analysis for ME/CFS (After COVID) [Jun 16,2022]
- 2023-06-22 – Repeat IBS + Vaccine + COVID [Jul 22,2022]
- 2023-09-04
His comments are short:
- I would say some small subjective improvements since last time, but no major changes. Reminder: I have a friendly MD in terms of antibiotics.
- Metronidazole was on top in the last samples, I did it back then.
- Comment: Metronidazole is no longer at the top but dropped down to 16% of the highest value. It appears to have done its magic in reducing the bacteria pointing to it as a tool..
Base Analysis
When people have multiple samples, I like to do side-by-side comparisons, especially when someone has been doing some of the suggestions suggested. The suggestions are computed and may not always work. Expert Systems and AI are not perfect; they typically do better than a person with only a few years of experience that has training in the discipline (better consistency, remember more facts, etc). How are we doing objectively?
Scores
We see two positive shifts in the latest sample: Increase of Anti inflammatory Bacteria Score and decrease of Histamine Producers.
| Sample | 2021-11-18 | 2022-05-20 | 2023-06-22 | 2023-09-04 |
| Anti inflammatory Bacteria Score | 54%ile | 43%ile | 63%ile | 87%ile 🥰 |
| Butyrate Bacteria Score | 57%ile | 56%ile | 57%ile | 54%ile |
| Histamine Producers | 78%ile | 82%ile | 81%ile | 67%ile 🥰 |
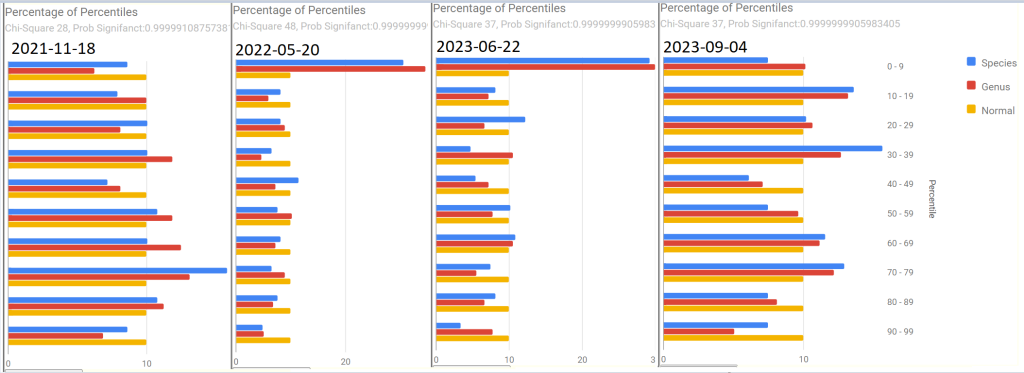
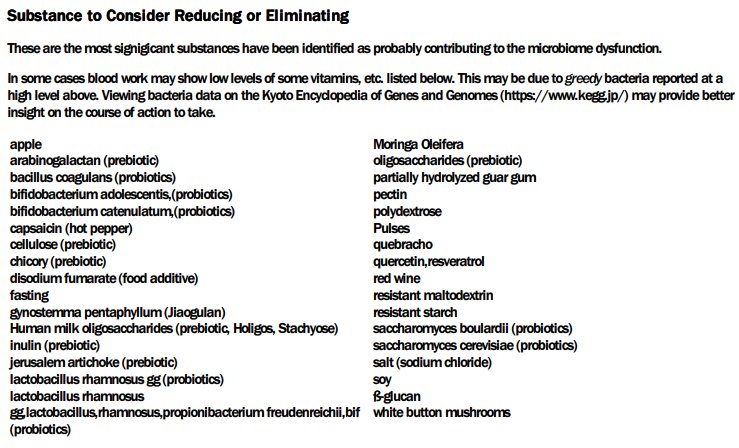
Percentages of Percentiles
We see a lot of bouncing around between samples. The middle two images matches the typical pattern seen with ME/CFS and Long COVID. Those shifts have faded over the last 3 months with a different pattern appearing indicating a different dialect of gut dysfunction.
Multi-Vector Comparison
The main numbers are below. The take away, less bacteria that are in the high percentile range (at 95%ile, 10 -> 28 -> 23 -> 8). The numbers bounce around with the middle two being similar and the other two also similar. There are no really clear shift in these measures.
| Criteria | 11/18/2021 | 5/20/2022 | 6/22/2023 | 9/4/2023 |
| Lab Read Quality | 8.1 | 5.5 | 4.7 | 7.2 |
| Outside Range from JasonH | 6 | 6 | 9 | 9 |
| Outside Range from Medivere | 16 | 16 | 15 | 15 |
| Outside Range from Metagenomics | 8 | 8 | 7 | 7 |
| Outside Range from MyBioma | 5 | 5 | 6 | 6 |
| Outside Range from Nirvana/CosmosId | 20 | 20 | 23 | 23 |
| Outside Range from XenoGene | 29 | 29 | 35 | 35 |
| Outside Lab Range (+/- 1.96SD) | 7 | 6 | 17 | 3 |
| Outside Box-Plot-Whiskers | 36 | 69 | 54 | 38 |
| Outside Kaltoft-Møldrup | 93 | 48 | 47 | 88 |
| Bacteria Reported By Lab | 652 | 508 | 542 | 558 |
| Bacteria Over 99%ile | 7 | 4 | 6 | 2 |
| Bacteria Over 95%ile | 10 | 28 | 23 | 8 |
| Bacteria Over 90%ile | 29 | 42 | 36 | 22 |
| Bacteria Under 10%ile | 208 | 41 | 50 | 175 |
| Bacteria Under 5%ile | 180 | 19 | 8 | 157 |
| Shannon Diversity Index | 1.853 | 1.826 | 1.272 | 1.556 |
| Simpson Diversity Index | 0.056 | 0.038 | 0.087 | 0.09 |
| Rarely Seen 1% | 2 | 2 | 7 | 1 |
| Rarely Seen 5% | 14 | 5 | 21 | 8 |
| Pathogens | 41 | 24 | 29 | 36 |
From Special Studies
The top match was the same on all of the samples, with an increase when there was actually COVID.
| Criteria | 11/18/2021 | 5/20/2022 | 6/22/2023 | 9/4/2023 |
| COVID19 (Long Hauler) | 28%ile | 33%ile | 41%ile | 28%ile |
| Next one: | 15%ile | 26%ile | 20%ile | 13%ile |
Health Analysis
Using Dr. Jason Hawrelak Recommendations, there are many items on the edge of being in range with some items of interest (I strike out those that are unlikely to be of great concern):
- Faecalibacterium prausnitzii at 27% of the microbiome or 96%ile
Akkermansia — 0.009 % of the microbiome or 35%ileBifidobacterium 0.016 % of the microbiome or 16%ileBacteroides – 27% of microbiome, or 64%ile
Additionally, two indicate increased risk of Candida (new feature just added)
- Phocaeicola dorei at 10% of the microbiome or 91%ile
- Faecalibacterium prausnitzii at 27% of the microbiome or 96%ile
I would suggest a test for candida to be safe. The data suggests a risk. If confirmed, candida would contribute significantly to gut dysbiosis [The interplay between gut bacteria and the yeast Candida albicans[2021]). I did a “back-flip” check of the top prescription items, and all of them reduces Candida (studies cited below).
Addendum – Predicted Symptoms
This was just added to the site today as a further refactor based on New Special Studies on Symptoms data. These are from [My Profile Tab]
| Criteria | 11/18/2021 | 5/20/2022 | 6/22/2023 | 9/4/2023 |
| Forecast Major Symptoms | Neurological: Cognitive/Sensory Overload 40 % match on 25 taxa DePaul University Fatigue Questionnaire : Racing heart 38 % match on 13 taxa DePaul University Fatigue Questionnaire : Difficulty falling asleep 37 % match on 27 taxa DePaul University Fatigue Questionnaire : Difficulty finding the right word 35 % match on 20 taxa | Autonomic Manifestations: urinary frequency dysfunction 66 % match on 6 taxa Immune Manifestations: Bloating 37 % match on 45 taxa Neurological-Audio: hypersensitivity to noise 35 % match on 28 taxa | None | Neurological-Sleep: Chaotic diurnal sleep rhythms (Erratic Sleep) 50 % match on 18 taxa Neurological: Spatial instability and disorientation 37 % match on 16 taxa |
This can be helpful for judging possible severity (and potential improvement of some symptoms), for example: Neurological: Cognitive/Sensory Overload. See [Special Studies] tab.
- 2021 – 40% matches
- 2022- 24% matches
- 6/22/23 – 16% matches
- 9/4/2023 – 4% matches
Going Forward
COVID has had quite an impact on this microbiome. I am going to just go with the “Just Give Me Suggestions” option with the addition of what matched his diagnosis:
- Irritable Bowel Syndrome (68 %ile) 7 of 68
To explain a bit more. First I click the button below
And then click I could click the consensus report to see what the top items are:

Which are shown below.
In this case, I want to add Irritable Bowel Syndrome suggestions (on the Changing Microbiome Tab)
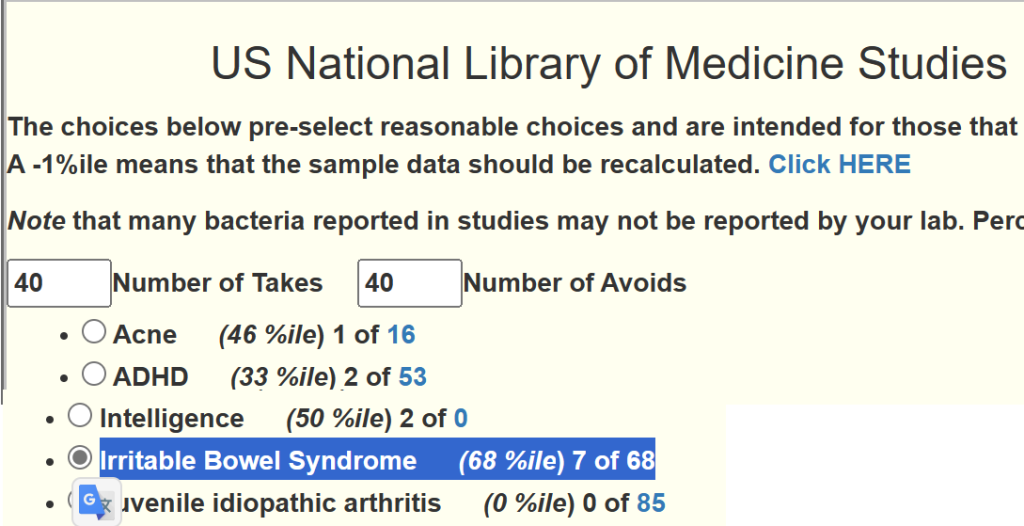
Instead of the usual 4 packages of suggestions, we have 5
When we look at the consensus report we see the same items there, but the values have increased.
The intent is put a little bias on the numbers towards specific conditions of greatest concern.
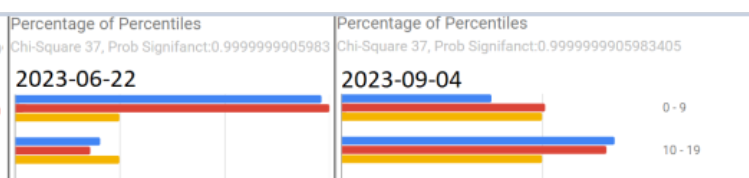
PDF Suggestions
I tend to favor the PDF suggestions because it simplifies things for many readers. Also the PDF gives a good list of citations (never complete) used to make the citations to persuade MDs to see that the suggestions are based on studies — a lot of studies.
The PDF suggestions are below (using the consensus view is another option for those more technically orientated). I clip from the PDF to keep the blog simpler for the typical reader.
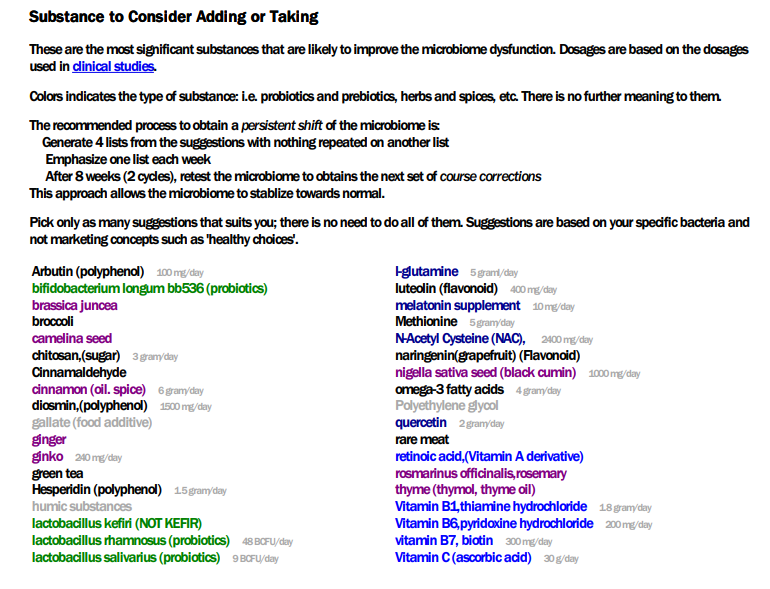
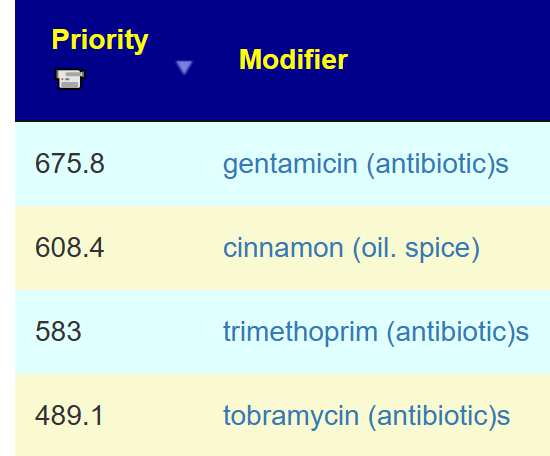
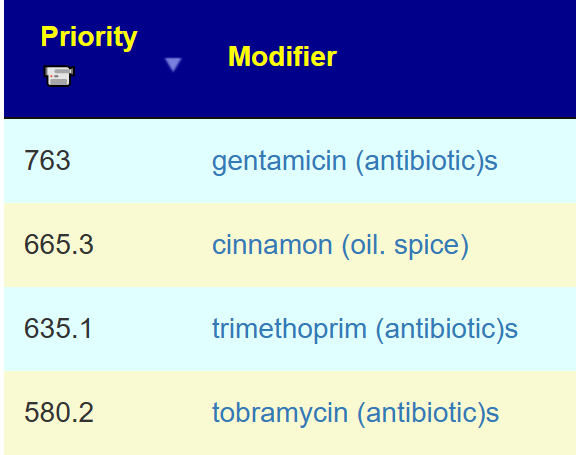
This is a little longer list than usual, so I went to the consensus report to get priority data. Top value was 618, so 309 is the 50% threshold.
- Top Items:
- cinnamon (oil. spice): 571
- green tea: 435
- Hesperidin (polyphenol): 428
- omega-3 fatty acids: 395
- rosmarinus officinalis,rosemary: 395
- N-Acetyl Cysteine (NAC): 354
- Vitamins:
- Probiotics.
- lactobacillus salivarius (probiotics): 402
lactobacillus rhamnosus (probiotics): 339- lactobacillus rhamnosus gg (probiotics): -352, thus there is a risk and I would avoid.
- lactobacillus kefiri (NOT KEFIR): 292 –Note: For sale in Italy
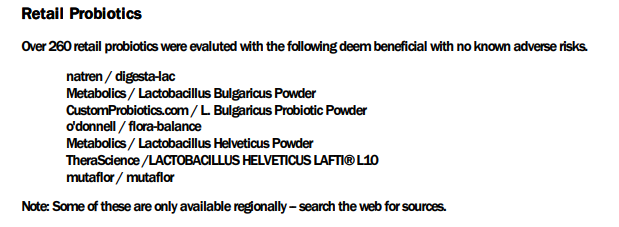
These appear to be of low influence with the exception of l.bulgaricus:
- mutaflor escherichia coli nissle 1917 (probiotics): 1.41 (only in 1 of the 5 suggestions sets)
- lactobacillus bulgaricus (probiotics): 221 (on 4 of the 5 suggestions sets)
- lactobacillus helveticus: 99 (on 2 of 5 suggestions sets)
Minor note: quercetin with resveratrol is an avoid, quercetin is a take. resveratrol by itself is a negative (-113). At times, you need to look at the technical details/consensus to clarify things; the data we are using is incomplete and sparse…. If clearly contradictory suggestions appear, then don’t do them (thing an abundance of caution).
Because he has an antibiotic friendly MD, the following are the TOP antibiotics with notes:
- gentamicin (antibiotic)s: 618, an Aminoglycoside
- “Since gentamicin has minimal gastrointestinal absorption,…it has applications in several clinical scenarios, such as bacterial septicemia, meningitis, urinary tract infections, gastrointestinal tract (including peritonitis), and soft tissue infection,” NIH StatPearls
- Antifungal Activity of Gentamicin B1 against Systemic Plant Mycoses [2020], i.e. candida
- trimethoprim (antibiotic)s: 552
- “The FDA-Approved indications include acute infective exacerbation of chronic bronchitis, otitis media in pediatrics only, travelers diarrhea for treatment and prophylaxis, urinary tract infections, shigellosis, pneumocystis jirovecii, pneumonia/pneumocystis carinii pneumonia (PJP/PCP), and toxoplasmosis, both as prophylaxis and treatment. ” NIH StatPearlls
- atorvastatin (prescription): 459
- medications decrease cholesterol production in the liver. NIH StatPearls
- Antifungal effect of Atorvastatin against Candida species in comparison to Fluconazole and Nystatin [2019]
- ofloxacin (antibiotic)s : 386, sparfloxacin (antibiotic): 381 – these are Quinolones (i.e. fluoroquinolone) many people have issues with using these, see this post for discussion: Update #4 on ME/CFS Person
CFS Antibiotics are also above the threshold. Since the prior sample had a strong Long COVID or ME/CFS Profile, I would be inclined to include one of those below in the antibiotic rotation. The microbiome cannot make a diagnosis of most things, with most ME/CFS microbiomes there is a particular pattern which you had in your last sample but which has disappeared from your current sample which looks more like your first sample. I read this as recovering from ME/CFS…. in likely a fragile state since relapse is very common with ME/CFS.
- azithromycin,(antibiotic)s[CFS]: 349
- amoxicillin (antibiotic)s[CFS]: 327
- Of those below, I would favor: minocycline (antibiotic)s[CFS]: 293
My own experience is that it is better to overcure ME/CFS and when there are signs of recovery…. no backflips of joy or running marathons; keep doing slow walks that becomes a bit further each week for 6-12 months. Your microbiome is fragile and can quickly slip back.
I prefer to use the strategy of going for prescription items that are both suggested from the microbiome and been shown to help with one or more of the diagnosis conditions. This usually encounter low resistance from physicians — they are clueless for the microbiome, but very accepting of published studies. An antibiotic that is used as a prophylaxis usually encounter little resistance.
KEGG Suggestions
This is done by using information from the bacteria found with some fudge factors. I am in discussion with some Ph.D. candidates to build this concept directly from the FASTQ files and will hopefully have this as an added feature next year.
The KEGG probiotics is the usual pattern for ME/CFS and Long COVID with the top one being the usual, with the top reasonably available ones for other families shown below. I usually like to compare the values with those from consensus to minimum risk (i.e. two thumbs up, we do; mixed, we skipped)
- 170.6 Escherichia coli:
- 50 Bifidobacterium bifidum (and the rest lower)
- -240 bifidobacterium bifidum (probiotics) 🙁
- Other bifido are positive on both, especially bifidobacterium longum bb536
- 56 Lactobacillus plantarum subsp. plantarum
- -132 lactobacillus plantarum (probiotics)
- Other Lacto are positive, especially lactobacillus salivarius (probiotics)
- 49 Akkermansia muciniphila – not in consensus
- 37 Lactococcus lactis – not in consensus
KEGG Supplements
From the list, we will look only at those with a z-score (statistical significance) over 2. After each we put the consensus value (if it is listed)
- Phenylalanine
- Tryptophan -50
- Cysteine: + 459, N-Acetyl Cysteine (NAC),
- Aspartic acid
- Biotin (Vitamin H): + 392 Vitamin B7, biotin
- Serine
- Tyrosine
Only two items are with high confidence.
How to Proceed Suggestions
The suggestions should be thought as influencers. The human population is often a good analogy or parable for the microbiome population. Each influencer shifts the population in the desired direction. Based on Cecile Jadin’s work and several studies, I am a firm believer in short duration (1-2 weeks) of each influencers. Just as with human influencers, people stop listening if the same person just keeps droning on and on. If a different person starts speaking, you get persuaded more. If a mob start to shout, yet a different human behavior will occur. In terms of the microbiome, “stop listening” means mutations that are resistant to the item will start to increase. Items line vitamins and minerals can be taken continuously; items that are likely to have bacteria resistance developed should be taken for a week and then another item replace it.
The items to rotate:
- Antibiotics listed above
- Probiotics: lactobacillus salivarius and lactobacillus bulgaricus
- Herbs and spices: cinnamon, ginger, black cumin, thyme, rosemary, quercetin (suggests just before each antibiotic with a few days of overlap because it has potential synergistic activity with antibiotics [2020], [2016],[2018] )
Remember our goal is to destabilize a stable microbiome dysfunction.
Questions and Answers
While there has not been significant changes in many of the vectors between this sample and the prior sample from a few months earlier, there has been two significant objective changes:
- Significant improvement of Anti inflammatory Bacteria Score (higher) and Histamine Producers (Lower).
- The lost of the ME/CFS – Long COVID spike in the 0-9%ile
Q: Do you/should I use the colored list now instead of the consensus list?
- Either are fine, the color list (from PDF) is what I tend to use in post because it is easier for new readers to understand (and automatically sent on new uploads). The consensus page is more complex but allows people to apply their own logic and priorities.
Q: “Quercetin (suggests just before each antibiotic with a few days of overlap because it has potential synergistic activity with antibiotics”
- Yes, there are several studies similar to this one. Potential synergistic activity of quercetin with antibiotics against multidrug-resistant clinical strains of Pseudomonas aeruginosa,[2020]
Q: I just did Mutaflor for 8 days and felt really tired all the time (but in the end I also got a flu/cold, so maybe that was the reason and not mutaflor). Nevertheless, if it was a herx reaction, I wonder if I should have taken it for longer until the reaction disappeared? (I stopped it 4 days ago.) Not sure if this question even makes sense.
- My personal choice would be to keep taking it for at least a week (perhaps 2). Remember that the traditional pattern for a herx is feeling bad for X hours and then things get better. The duration of the feeling bad usually decrease from day to day. Catching a cold makes interpretation challenging.
Postscript – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I can compute items to take, those computations do not provide information on rotations etc.
I cannot tell people what they should take or not take. I can inform people items that have better odds of improving their microbiome as a results on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting.
The answers above describe my logic and thinking and is not intended to give advice to this person or any one. Always review with your knowledgeable medical professional.
Interesting that the Kegg Supplements include phenylalanine, tryptophan and tyrosine. These are essential amino acids that only a microbiome can produce via the shikimate biochemical pathway. This pathway is suppressed by glyphosate that is widely found in food due to it’s widespread use in the Western food production system. More usual in processed and conventionally-produced food. Biodynamic, regenerative and organic food choices are a way to avoid glyphosate.