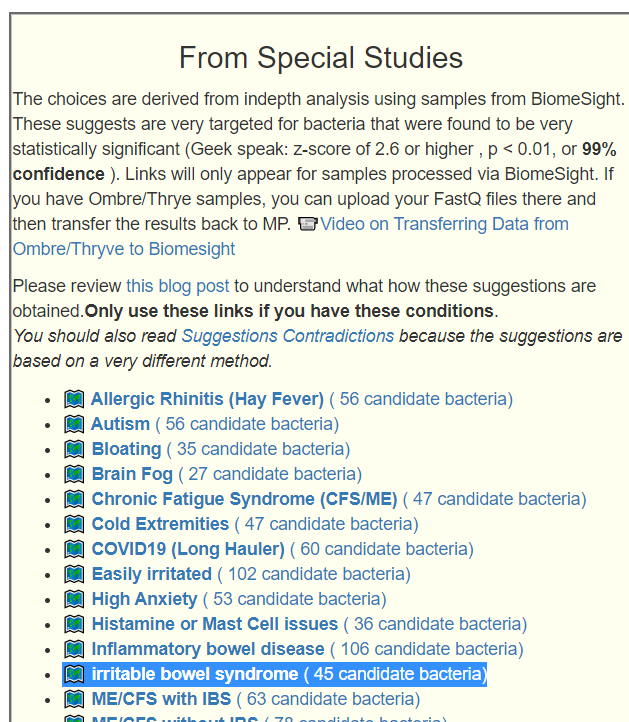
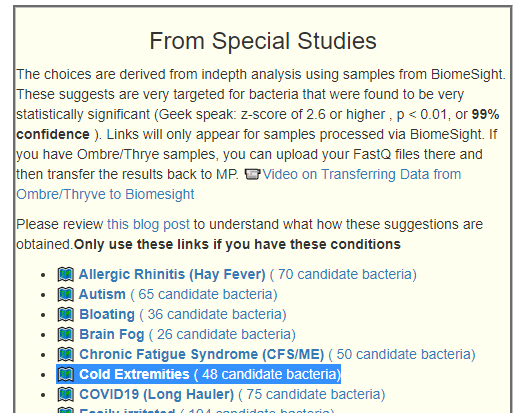
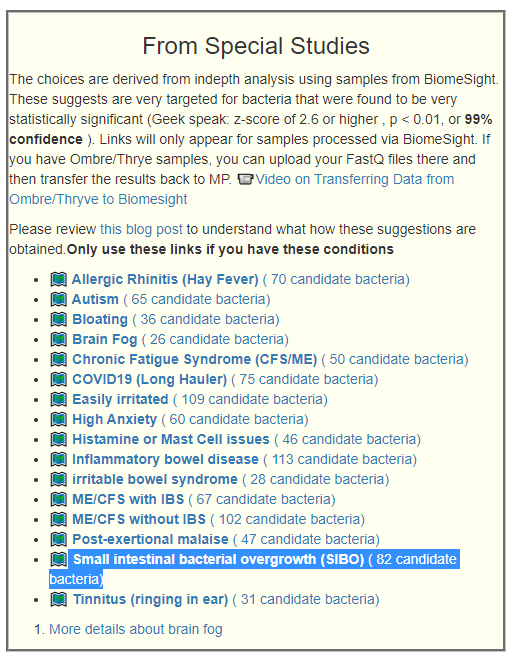
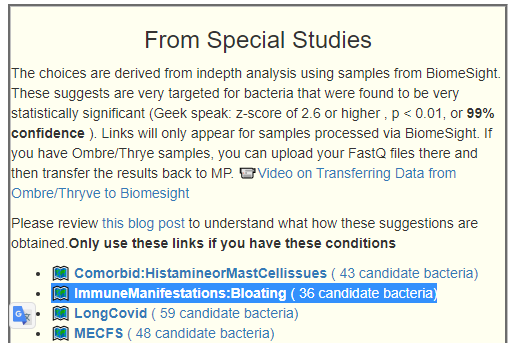
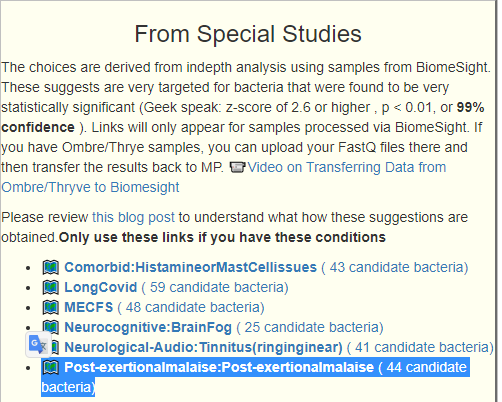
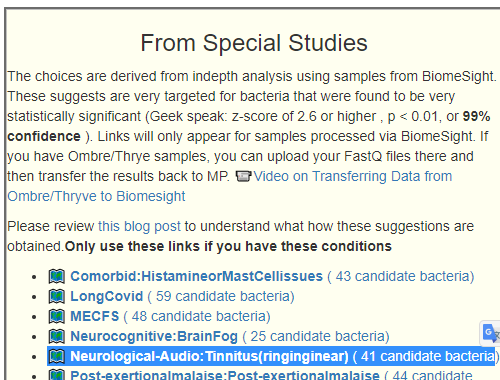
We have IBS annotated in three different ways:
- Autonomic Manifestations: irritable bowel syndrome
- Official Diagnosis: Irritable Bowel Syndrome
- Condition: ME/CFS with IBS
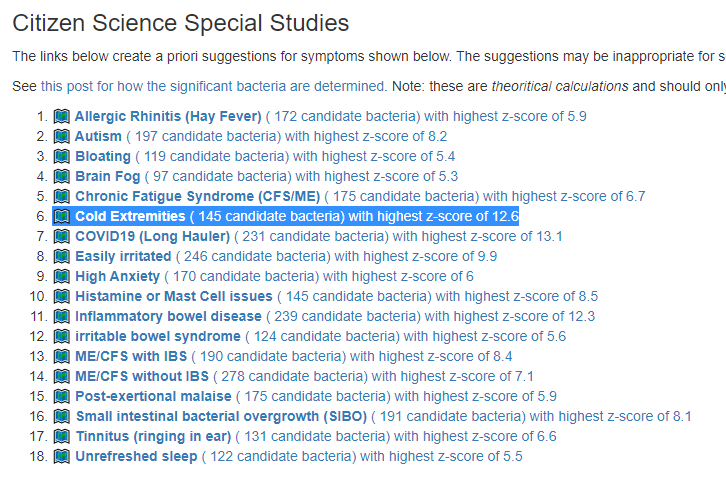
I ran each possible combination of the above and Official Diagnosis: Irritable Bowel Syndrome gave the strongest results and this will be reported here. When other things are combined, it is common for associations to become diffused/weaker. This is part of A new specialized selection of suggestions links.
Study Populations:
| Symptom | Reference | Study |
| Official Diagnosis: Irritable Bowel Syndrome | 1122 | 56 |
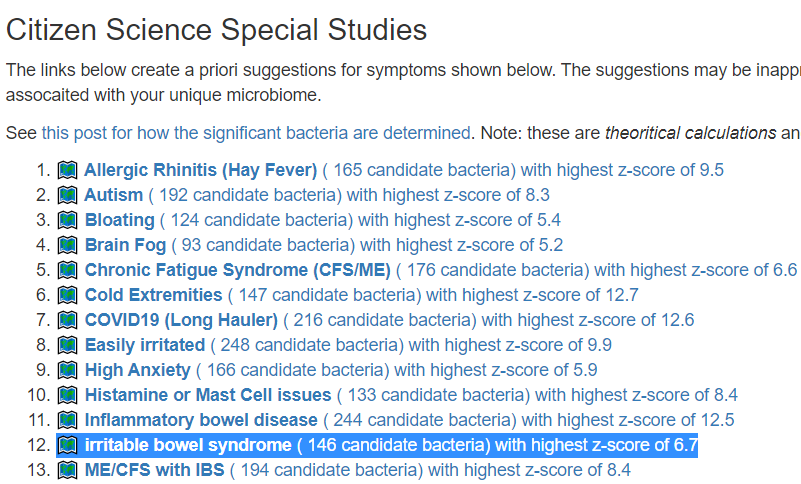
- Bacteria Detected with z-score > 2.6: found 148 items, highest value was 6.7
- Enzymes Detected with z-score > 2.6: found 218 items, highest value was 6.1
- Compound Detected with z-score > 2.6: found No items
Interesting Significant Bacteria
The results are very striking — low bifidobacterium across the board at the top! Almost all of the bacteria associated are low.
| Bacteria | Reference Mean | Study | Z-Score |
| Bifidobacterium gallicum (species) | 3741 | 587 | 6.7 |
| Bifidobacterium kashiwanohense PV20-2 (strain) | 325 | 62 | 6.6 |
| Bifidobacterium catenulatum subsp. kashiwanohense (subspecies) | 315 | 62 | 6.6 |
| Thermosediminibacterales (order) | 49 | 16 | 6.3 |
| Lactiplantibacillus pentosus (species) | 123 | 28 | 5 |
| Escherichia (genus) | 5983 | 1397 | 4.9 |
| Bifidobacterium cuniculi (species) | 81 | 30 | 4.7 |
| Bifidobacterium angulatum (species) | 184 | 32 | 4.7 |
Interesting Enzymes
As is often seen with various symptoms/conditions, the associations are due to insufficiency and not surplus.
| Enzyme | Reference Mean | Study Mean | Z-Score |
| substrate,NADPH—hemoprotein reductase:oxygen oxidoreductase (RH-hydroxylating or -epoxidizing) (1.14.14.1) | 51 | 19 | 6.1 |
| NADPH:hemoprotein oxidoreductase (1.6.2.4) | 51 | 19 | 6.1 |
| propanoyl-CoA:oxaloacetate C-propanoyltransferase (thioester-hydrolysing, 1-carboxyethyl-forming) (2.3.3.5) | 1480 | 381 | 6.1 |
| (2S)-3-(4-hydroxyphenyl)-2-isocyanopropanoate,2-oxoglutarate:oxygen oxidoreductase (decarboxylating) (1.14.20.10) | 131 | 26 | 6 |
| (2S)-3-(4-hydroxyphenyl)-2-isocyanopropanoate,2-oxoglutarate:oxygen oxidoreductase (1.14.20.9) | 131 | 26 | 6 |
| (2S,3R)-3-hydroxybutane-1,2,3-tricarboxylate pyruvate-lyase (succinate-forming) (4.1.3.30) | 1432 | 375 | 5.9 |
| ATP:amicoumacin A 2-phosphotransferase (2.7.1.230) | 41 | 18 | 5.7 |
| (E)-4-(trimethylammonio)but-2-enoyl-CoA:L-carnitine CoA-transferase (2.8.3.21) | 1354 | 388 | 5.7 |
| gamma-butyrobetainyl-CoA:electron-transfer flavoprotein 2,3-oxidoreductase (1.3.8.13) | 1365 | 390 | 5.7 |
| L-carnitine:CoA ligase (AMP-forming) (6.2.1.48) | 1339 | 443 | 5.4 |
| hydrogen-sulfide:ferredoxin oxidoreductase (1.8.7.1) | 9912 | 4683 | 5.3 |
| NADPH:acceptor oxidoreductase (1.6.99.1) | 5684 | 2284 | 5.3 |
| (2S,3S)-2-hydroxybutane-1,2,3-tricarboxylate hydro-lyase [(Z)-but-2-ene-1,2,3-tricarboxylate-forming] (4.2.1.79) | 1284 | 407 | 5.2 |
| S-methyl-5′-thioadenosine:phosphate S-methyl-5-thio-alpha-D-ribosyl-transferase (2.4.2.28) | 3638 | 1668 | 5.1 |
| acyl-CoA,ferrocytochrome b5:oxygen oxidoreductase (6,7 cis-dehydrogenating) (1.14.19.3) | 1062 | 284 | 5 |
| butanoyl-CoA:acetoacetate CoA-transferase (2.8.3.9) | 3892 | 2229 | 5 |
| L-carnitinyl-CoA hydro-lyase [(E)-4-(trimethylammonio)but-2-enoyl-CoA-forming] (4.2.1.149) | 1422 | 362 | 5 |
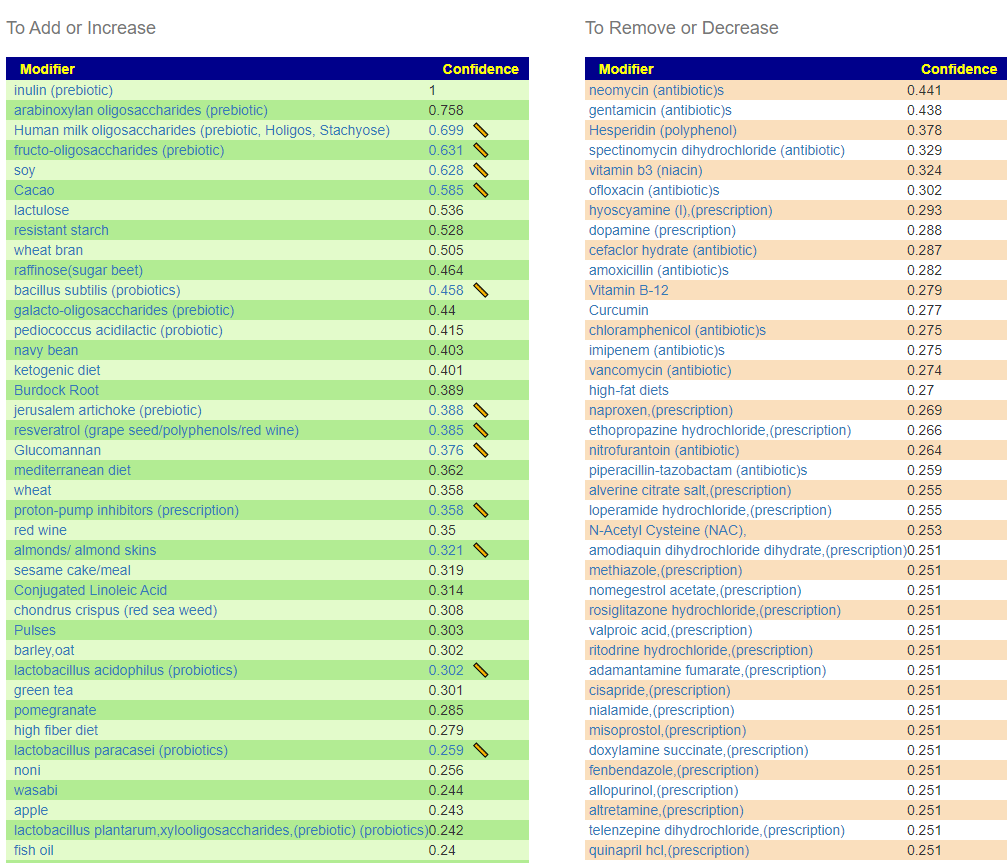
Bottom Line
Looking at the bacteria, the probiotic solution would be:
- Bifidobacterium (a wide variety)
- E. Coli Probiotic (Mutaflor or Symbioflor-2)
Lactobacillus are HOSTILE to E.Coli, so Lactobacillus probiotics should likely be avoided.
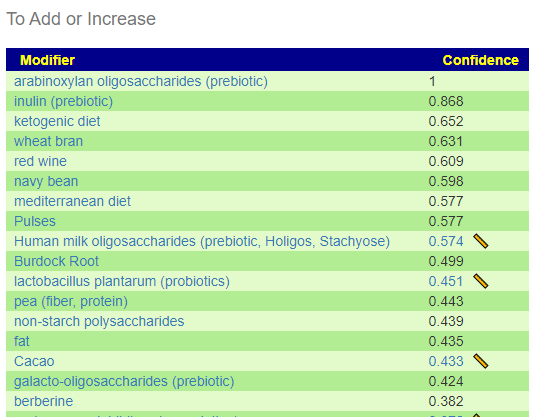
Looking at some of the recommendations, we see Human milk oligosaccharides (prebiotic, Holigos, Stachyose) which are known to greatly encourage bifidobacterium. We also see saccharomyces boulardii which is also known to increase Bifidobacterium [2020].
As always, using your own 16s samples would produce the best suggestions.

Recent Comments