This post was triggered by the email below. They included a Biomesight microbiome test, Mosaic Organic Acid Test and a Gastric Tissue report. My expertise is solely the microbiome as a statistican so I will ignore all except the microbiome test.
Key Question: Is “vaccine injury” is a permanent condition?
- Answer: No, the most probable cause of vaccine injury is a vaccine response triggering or worsening a microbiome dysbiosis. See the literature below.
- A microbiome dysbiosis may self-resolve for some people (i.e. people feel off for a few days or weeks after the shot) or become stable — requiring sophisticated intervention.
- There can be other speculated mechanism (autoimmunity induced, molecular mimicry or bystander activation) but they lack clear evidence, and are often based on ideological beliefs. I keep to Osler Principle and the simplest explanation supported by evidence.
- Followup from reader: H1N1 Influenza Pandemrix vaccine which caused narcolepsy (autoimmune disease) due molecular mimicry, which is my worst fear..
- Correct: Narcolepsy Associated with Pandemrix Vaccine [2018]. This is one specific vaccine, not for all vaccines (my scope). The researchers who found this in the data would have reported all vaccines with similar side effects if there was data supporting it. [Studies] It seems to be associated to H1N1 vaccines.
I wanted to give you a rundown of what’s been going on with me. On January 6, 2023, I got the third dose of the nonavalent HPV vaccine, Gardasil 9. Immediately after the shot, I felt wiped out and weird, but my symptoms subsided only to come back with vengeance two weeks later.
A reader on CFS Remission
The symptoms I experienced were all the classic ME/CFS ones, specifically POTS, tachycardia, panic attacks, brain fog, blurred vision, shortness of breath, trouble finding words, fatigue, PEM, fasciculations, neuropathy, pins and needles, Raynaud’s phenomenon, joint pain and joint cracking, food intolerances and food malabsorption, yellow mushy stools, and some more alarming sensations: like feeling that my body was heavy, like it was made of concrete, a sensation of electric shocks in my arms, and tingling in my feet that moved to my hands a couple of times.
Since then, some symptoms have disappeared, but others remain and new ones pop up. Right now, the symptoms I still have are joint pain and joint cracking, fasciculations, malabsorption and yellow stools, what I think is Raynaud’s phenomenon (my hands are red most of the time), and, at the moment I’m writing this message, heavy drowsiness and a general feeling of malaise, which is discouraging, since I felt better earlier this month and thought I was finally getting out of this nightmare.
Overview
This is a two-sided discussion exploring the interaction between vaccinations and the microbiome from both perspectives:
- How vaccinations may alter the microbiome
- How the existing state of the microbiome may influence the effectiveness of a vaccination
To be transparent, I want to share that I personally experienced an adverse side effect following a series of vaccinations. The side effect involved severe gingival (gum) recession, causing the roots of my teeth to become fully exposed. Unfortunately, the condition progressed to the point where dentures became necessary due to the extent of gum loss.
At a high level, interactions in both directions are not only possible but expected. Vaccinations stimulate the immune system, similar to a natural infection — and any shift in immune function can, in turn, affect the microbiome. Conversely, the microbiome plays a key role in shaping immune responses, meaning it can directly influence how the body responds to vaccines.
It’s important to remember that the primary goal of any vaccination is to safely prompt the immune system to build protection against a specific infection. However, because the microbiome and immune system are deeply interconnected, this process can be more complex than it first appears.
Vaccination to Microbiome
A few studies of interest:
Growing evidence shows that the composition of the intestinal microbiota, which is known to play an important role in the development and regulation of immune responses7, influences responses to vaccination8,9,10. Studies which have investigated this have shown that a higher relative abundance of the phylum Actinobacteria is consistently associated with higher vaccine responses and a higher relative abundance of Bacteroides with lower responses, while the association between the relative abundance of the phyla Firmicutes and Proteobacteria and vaccine responses varies for different genera and species11,12,13,14,15,16,17,18.
The immunological interplay between vaccination and the intestinal microbiota [2023]
A recent study using metagenomic sequencing, reported that the intramuscular administration of an inactivated and an mRNA SARS-CoV-2 vaccine was associated with lower bacterial diversity, an increase in the relative abundance of Bacteroides caccae and a decrease in the relative abundance of Clostridiales (Coprococcus comes, Dorea longicatena and Ruminococcus obeum) in the intestinal microbiota one month after vaccination
… a total of 15 bacterial species in the baseline gut microbiome were identified, of which Bifidobacterium adolescentis was enriched in high-responders while Bacteroides vulgatus, Bacteroides thetaiotaomicron and Ruminococcus gnavus were more abundant in low-respondersGut microbiota composition is associated with SARS-CoV-2 vaccine immunogenicity and adverse events [2021]
Microbiome to Vaccination Effectiveness
Not only do pathogens exert immunomodulatory effects, but the microbes that populate a healthy human host, known as the microbiome, can also influence the immune response.4,11
Influence of the microbiome on response to vaccination [2015]
When facing respiratory syncytial virus (RSV), mice supplemented with Lactobacillus showed an enhanced immune response
One of these factors seems to be the microbiome differences among individuals (101, 102). A growing number of studies suggest that the microbiome can modulate immune responses induced by vaccines (103, 104). Huda et al. (105) studied infants’ microbiomes to evaluate how their microbiome composition influenced the response to oral PV and hepatitis B virus vaccines. They found that Actinobacteria species prevalence may increase the vaccine response, while Enterobacteriales, Pseudomonadales, and Clostridiales were associated with lower response to the aforementioned vaccines. Hagan et al. (106) showed that differences in the microbiome can alter the responses of humans vaccinated against IAV.
The Interplay between the Host Microbiome and Pathogenic Viral Infections [2021]
Gut microbiota composition is associated with SARS-CoV-2 vaccine immunogenicity and adverse events
Analysis
My model is that ME/CFS is a microbiome dysbiosis. A vaccination is a microbiome disruptor — for most people, they recover. If you start with dysbiosis, then recovery may be a bit less likely.
Urban Legend in some ME/CFS groups is that people with ME/CFS do not catch things. There may some truth to it — virus friendly to the typical microbiome may find the dysbiosis of the ME/CFS patient very unfriendly. Secondly, (with a little tongue in check humor) how can they tell!!!
It turns out that virii often requires specific species to infect a person.
certain microbiome can be essential for a virus to infect its host. Jones et al. (82) showed that human norovirus needs Enterobacteria spp. to successfully infect B cells, as this bacterium aids in the attachment of the virus to the host cell. Norovirus infection in mice requires the microbiota to be persistent (83): mice with a depleted microbiome prevented persistent norovirus infection.
The Interplay between the Host Microbiome and Pathogenic Viral Infections
Going Forward
The phrase of “Vaccine Injury” is very misleading and implies that the body is somehow injured in potentially a permanent way. I believe that “Vaccine Dysbiosis” is a better and more accurate term.
We find a mountain of literature associating a vast array of different virii to ME/CFS. A few examples are:
- Epstein-Barr Virus (EBV)
EBV, which causes infectious mononucleosis, is one of the most frequently implicated viruses in ME/CFS. Studies show that 8–15% of people who develop infectious mononucleosis go on to meet ME/CFS criteria, and a subgroup of ME/CFS patients show evidence of EBV reactivation or immune response abnormalities related to EBV5 7. - Human Herpesvirus 6 (HHV-6)
Reactivation of HHV-6, another common herpesvirus, has been hypothesized to contribute to ME/CFS symptoms, particularly in combination with EBV reactivation7. - Enteroviruses
Historical and contemporary evidence links enteroviruses (a group that includes polioviruses, coxsackieviruses, and echoviruses) to ME/CFS. Outbreaks of ME/CFS have coincided with enteroviral epidemics, and some researchers consider enteroviruses a likely culprit, especially in cluster cases1. - Influenza Viruses
Influenza infection has been associated with a more than two-fold increased risk of developing ME/CFS in the years following infection17. - SARS-CoV-2 (COVID-19)
Many individuals with long COVID meet criteria for ME/CFS, and SARS-CoV-2 is recognized as a trigger for ME/CFS in some cases67. - Other Herpesviruses
Varicella zoster virus (which causes chickenpox and shingles) and other herpesviruses have also been reported as potential triggers7. - Ross River Virus
This mosquito-borne virus has been linked to ME/CFS onset, likely through immune system dysregulation3. - Retroviruses (e.g., XMRV)
Early studies suggested an association between the retrovirus XMRV and ME/CFS, but this link has been discredited by subsequent research and retraction of the original findings2.
The goal of vaccines is to trigger enough of a response to set up the body to fight the target infection. Unfortunately, it also has a risk of triggering ME/CFS in some cases. If the person has ME/CFS, it may trigger cascades like reported above.
Going Forward
Forget about trying to “repair the injury”, the ‘injury’ is dysbiosis. You want to correct the dysbiosis. He did not have a prior to vaccination test to use for reference 🙁 .
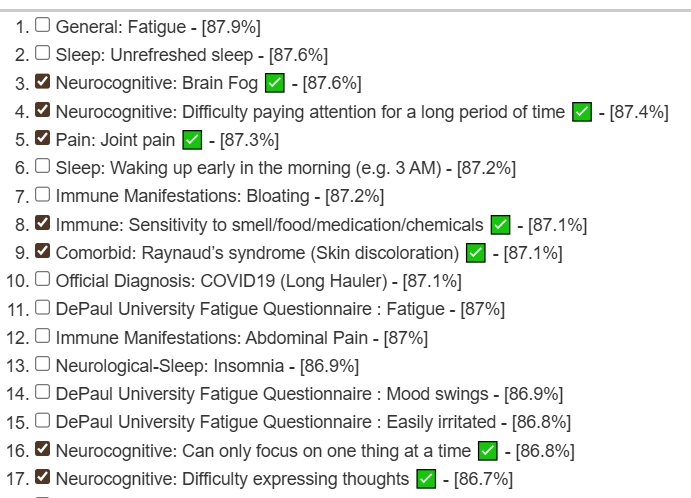
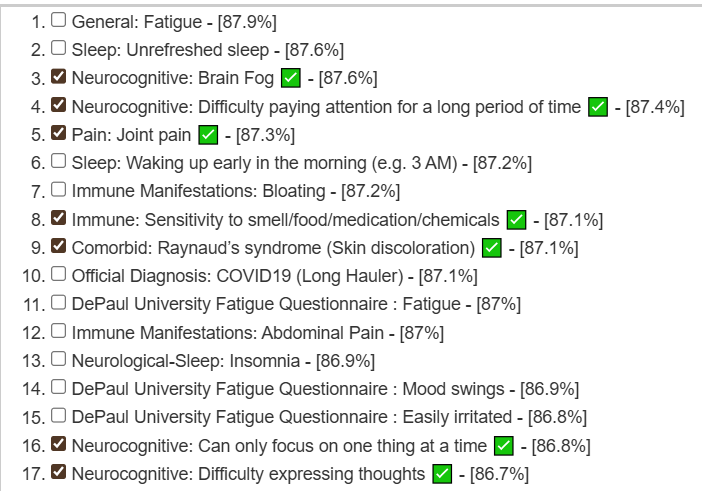
Looking at the forecasted symptoms and the symptoms he marked we see a lot of matches at a high level (> 85%)
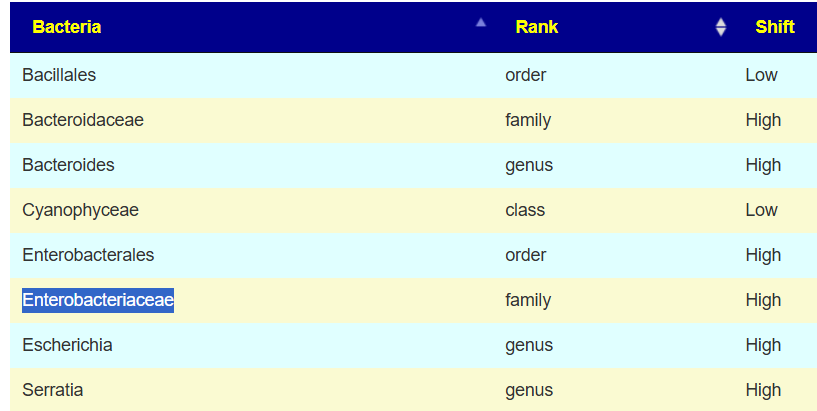
Looking at the bacteria that the above picked, we have one that is in the literature is associated with norovirus above.
Looking at the shifts reported for COVID, we see 64 matches to reported bacteria shifts from the literature.
| Adlercreutzia – genus : Low 21 Adlercreutzia equolifaciens – species : Low 14 Aeromonadaceae – family : Low 2 Akkermansia – genus : Low 12 15 16 22 24 Akkermansia muciniphila – species : Low 10 13 Anaerococcus – genus : Low 13 Bacillota – phylum : Low 14 Bacteroides – genus : High 1 4 11 13 14 24 25 Bacteroides stercoris – species : High 13 14 Bacteroides uniformis – species : Low 13 14 Bacteroidia – class : High 9 Bacteroidota – phylum : High 9 14 Blautia – genus : Low 5 6 12 13 16 Blautia obeum – species : Low 8 13 Clostridia – class : Low 23 Clostridiaceae – family : Low 14 Collinsella aerofaciens – species : High 7 14 Coprococcus – genus : Low 12 13 14 Coprococcus catus – species : Low 14a | Dorea formicigenerans – species : Low 8 13 Enterobacterales – order : High 18 Enterobacteriaceae – family : High 2 13 14 16 17 19 20 Escherichia – genus : High 3 14 17 Escherichia coli – species : High 14 Eubacterium – genus : Low 11 13 21 Faecalibacterium – genus : High 1 4 12 Finegoldia – genus : Low 13 Flavobacteriaceae – family : High 14 Gammaproteobacteria – class : High 14 Haemophilus – genus : High 16 Lachnospiraceae – family : Low 3 11 14 21 Moraxellaceae – family : Low 2 Oscillospira – genus : Low 24 Ruminococcus – genus : Low 6 12 13 16 24 Ruminococcus bromii – species : Low 13 Spirochaetia – class : Low 14 Spirochaetota – phylum : Low 14 Verrucomicrobiota – phylum : Low 22 |
The top results are very typical for ME/CFS: specific antibiotics used with the Jadin Protocol for ME/CFS. I know that both getting specific antibiotics off-label and often human reluctance to do them(valid from many horror stories of them being arbitrarily selected by MDs and making people worse) — makes that a path rarely travelled.
Looking at the R2 model for making probiotics do the work, the top ones (that are commercially available)
- In Research — not for sale
- Anaerobutyricum hallii – rank: 998
- Christensenella minuta – rank: 888
- Roseburia intestinalis – rank: 882
- Blautia wexlerae – rank: 823
- Blautia hansenii – rank: 748
- Faecalibacterium prausnitzii – rank: 697
- Top Recommendations
- Enterococcus faecium – rank: 687
- Lactococcus cremoris – rank: 558
- Akkermansia muciniphila – rank: 547
- Lactococcus lactis – rank: 331
- Leuconostoc mesenteroides – rank: 282
- Levilactobacillus brevis – rank: 236
- Fall backs – very small impact.
- Segatella copri – rank: 189
- Bacteroides uniformis – rank: 137
- Parabacteroides goldsteinii – rank: 136
- Ligilactobacillus salivarius – rank: 127
- Latilactobacillus sakei – rank: 111
- Bacteroides thetaiotaomicron – rank: 106
- Streptococcus thermophilus – rank: 89
- Lactiplantibacillus plantarum – rank: 88
- Bifidobacterium adolescentis – rank: 67
All of the items listed in 2 above are available from one or more of my usual sources except for Akkermansia which does have several providers today:
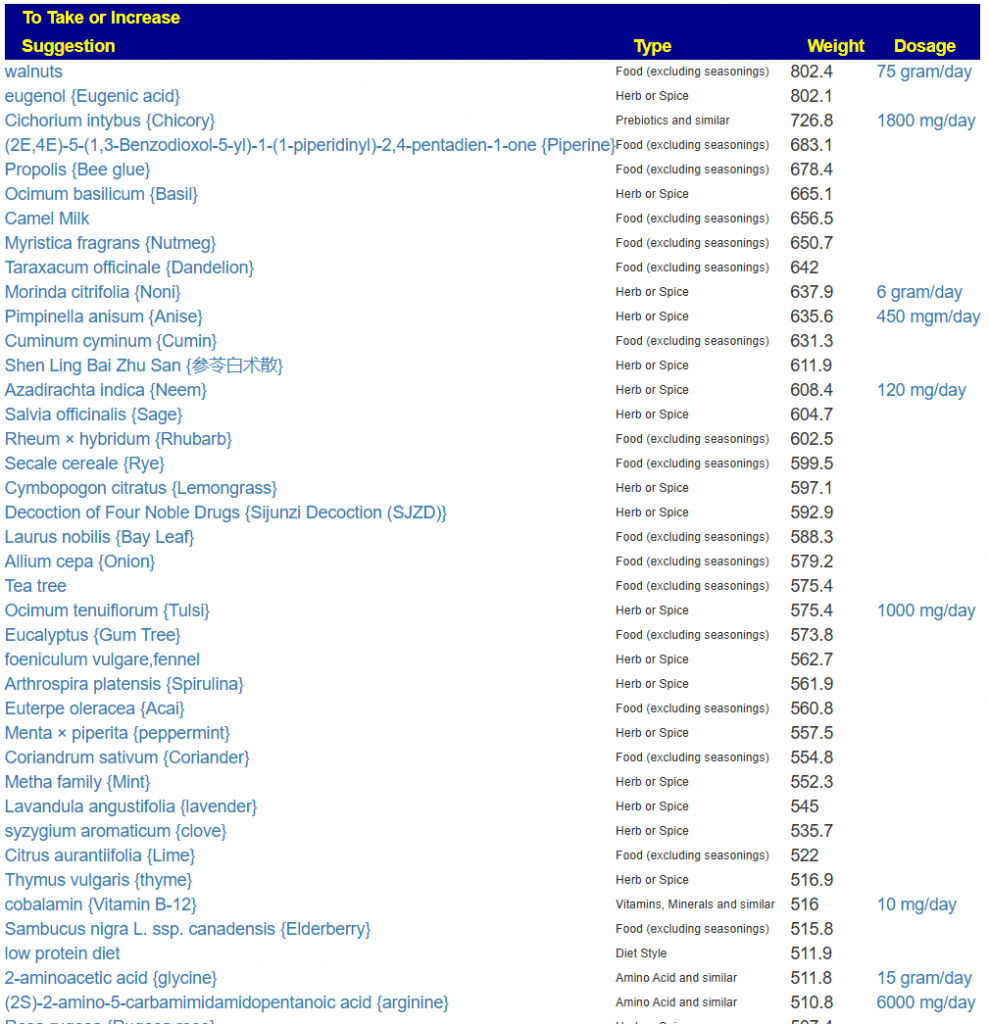
The next item are other suggestions which are listed below and high in herbs. As a FYI, Enterococcus faecium is actually the top probiotic using PubMed literature (and not R2 infererence) – I do like that type of convergence of different paths.
Suggested Methodology
- Get the probiotics in 2 above.
- Start the first and keep taking for 4 weeks (then 2 week break)
- Every week, add in one more probiotic for 4 weeks followed by 2 week break
- Do a lot of teas with different ones of the above herbs — if it is liquid, it should be a tea!
- Wheat bread are all avoids, so do 100% Rye bread which is on the above list (not wheat-rye mixtures)
Go through the consensus list for more information. Do a retest about 2-3 months after starting the above. The retest will show the next course correction (often there are many).
Questions and Answers
- The vaccine I got (HPV vaccine) is documented to cause ME/CFS and is one of the vaccines with higher number of reported adverse reactions compared to others. Why would you say is this?
- I tried to find this “documentation” and found this summary with studies
- Extensive research, including large register-based studies from Norway and Denmark, has found no evidence of a causal link between HPV vaccination and an increased risk of developing ME/CFS. (9 studies)
- Incidence rates of ME/CFS have not differed significantly between vaccinated and unvaccinated groups.
- Follow up from Reader: provided links to some studies
- to chronic epipharyngitis induced by adjuvants, not ME/CFS. adjuvants
- Possible Vaccine-Triggered Escalation of Undiagnosed Pre-Existing Mast Cell Disease – again not ME/CFS, and “possible” indicates speculation that is not supported by data.
- Postural Orthostatic Tachycardia With Chronic Fatigue After HPV Vaccination as Part of the “Autoimmune/Auto-inflammatory Syndrome Induced by Adjuvants” Single person case report is not evidence. Also note that the suspect cause was not the vaccine but Adjuvants.
- Postural tachycardia syndrome following human papillomavirus vaccination again not ME/CFS, but a condition shared by a few people with ME/CFS.
- Note these (and other links provided) found no statistically significant link — Adjuvants appears the most likely cause of side effects. Studies based on casual US studies (versus studies based on whole population medical data – for example Iceland) tend to be low quality.
- I tried to find this “documentation” and found this summary with studies
- I see you highlight the family Enterobacteriacea but ignore others like Bacteroides
- I picked Enterobacteriacea for purpose of illustration of one virus-microbiome interaction, there is not sufficient literature on HPV vaccine. We have extremely sparse data in this area.
- Microbiome Prescription also told me that I probably had lactic acid acidemia and biofilms but I didn’t understand it very well. Can you explain which implications have this and what bacteria may be causing it?
- Lactic Acid Acidosis means too much lactic acid. It is very common with ME/CFS and typically associated to brain fog. This is also associated with the following symptoms:
- Nausea and vomiting.
- Exhaustion and fatigue.
- Fast, deep breathing (respiratory compensation).
- Muscle cramps and body aches.
- Increasing weakness and drowsiness.
- Delirium and confusion.
- Ataxia.
- Oliguria (low urine output).
- Low body temperature.
- Low blood pressure.
- Fever.
- Jaundice (a yellow tint to the skin and whites of the eyes).
- Biofilms include dental plaque and often acts as “bullet proof vests” to bacteria that we want to change. See Wikipedia for more.
- Lactic Acid Acidosis means too much lactic acid. It is very common with ME/CFS and typically associated to brain fog. This is also associated with the following symptoms:
- Regarding the antibiotics, I was terrorized when I saw Ciprofloxacin at the top of the recommendations as it’s infamous for injuring people and causing a ME/CFS like condition, even being sold with a black label warning in the US. It seemed ironic to me and I am frankly hesitant to try it.
- The system does not consider these risks — that is for your medical professional to evaluate.
- I strongly favor Cecile Jadin’s approach. One course (7-10 days) of one antibiotic, 3 weeks off, rotate to another appropriate one. the ones marked with [CFS] have been use with some success for ME/CFS. I believe the issue cited was for continuous use of this antibiotic for more than one course. See this video for her experience. She has never seen in 20+ years of using it, adverse interactions. This also details her process (to be reviewed by your medical professional).
- The top two suggested probiotics, I haven’t heard of them in my life and haven’t seen them sold anywhere. Will they even still work?
- Enterococcus faecium – rank: 687 and Lactococcus cremoris – rank: 558 are likely not available at your local health food store. Enterococcus faecium Source, Lactococcus cremoris source
- They are computed to work — and my experience using the above sources for other probiotics is they work for me. One factor may be the freshness or the probiotics.
- Followup: I see Lactobacillus reuteri at the top of my probiotics suggestions list and don’t see Lactococcus cremoris at all. Are we look at the same screen?
- We are — there are several places that probiotics are predicted based on different data sources. See this video: https://www.youtube.com/watch?v=KvxJLYEGrwU
- I am coming out of a 14-day Rifaxamin cycle which I think caused my current neuropathy and I wonder if it altered my microbiome enough so the results of the Biomesight are no longer accurate. Is my suspicion of the neuropathy being caused by Rifaxamin accurate? It started on the very last days of the cycle and I also have neurological symptoms again after a long time without having them.
- Rifaximin are your current sample is listed as an avoid. Your neuropathy may have been contributed by it.
- I suspect that the suggestions will not be dramatically altered, so I would suggest implementing the top suggestions that you are comfortable with. Also, eliminate as many of the AVOIDS as is practical.
- I am also still taking Saccharomyces Boulardii, Lactobacillus Plantarum, Lactobacillus Gasseri and will be adding Colostridium Butyricum, Bacillus Coagulans and the mix of Bifidobacterias “Seeking Health ProBiota Bifidobacterium.” All of them suggested by ChatGPT o3 model after feeding it my Biomesight, OAT, and a wide array of conventional medical tests.
- ChatGPT can be best described as a hearsay model with hallucinations being well known.
- Most of the probiotics are fine — reservations on the Bifidobacterium mixture:
bifidobacterium adolescentis and bifidobacterium bifidum are to be avoided - I advocate probiotic rotations and not continuous. Many probiotics produce natural antibiotics. Continuously taking them promote “antibiotic resistance”.
- Also be aware of minimum effective dosages, Seeking Health ProBiota Bifidobacterium is 12 BCFU/capsule, it is not unusual to need at least 50 BCFU (of fresh probiotic) to have effect. See Probiotics — what is advertised may not be what you get for background.
- Most of the probiotics are fine — reservations on the Bifidobacterium mixture:
- ChatGPT can be best described as a hearsay model with hallucinations being well known.
- I find some of the recommendations given by Microbiome Prescription weird, like whole milk and camel milk. Didn’t Biomesight said that my lactose processing was low? Or walnuts. What kind of walnuts they need to be? Can they be pecans or indian walnuts?
- Microbiome Prescription will differ from Biomesight see Why sites suggestions disagree on the same data. In short, MP uses over 7,431,437 facts to compute decisions as of today. I do not know the number BS uses, I suspect very few. All suggestions can be traced back to studies. The names of suggestions are based on the terms used in studies.
- I do not know how many studies they based “lactose processing was low”, I see lactose as a significant positive value in your results (400).
- Also most of them are herbs like you said or non foods like spices and other odd things. Is this common for other microbiomes?
- I view every microbiome as different. The suggestions that I see are similar to others with ME/CFS, see other analysis here.
Followup: As I am not doing well economically and looking for ways to save, I feed ChatGPT o3 model the Microbiome Prescription suggestions table and told it to look for probiotic mixtures with the most amount of recommended strains and the least of strains to be avoided, Seeking Health ProBiota Bifidobacterium was the result.
I was aware of the wrong strains on the mixture and asked ChatGPT about the impact they would had. It told me that even then, it was still worth the risk as the strains to avoid had relatively low impact (Bifidobacterium bifidum -132.8) compared to the recommended strains on the mix (Bifidobacterium Longum 540.3).
You see this as an accurate analysis from ChatGPT or you would still recommend to avoid them?
In case that you say yes… Can I take all the probiotics I previously told at once or they antagonize each other? Is doing this risky?
ChatGPT and other Large Language Model are sophisticated Hearsay-Engines. The lack the expertise of a fuzzy logic expert system. If I was a judge, I would strike hearsay evidence from consideration. The issue of risk is a question for your medical professional. All that I can say is that it was decreased odds of helping and may have some risk of hurting.
5.- “I see lactose as a significant positive value in your results (400).”
A = I am talking about the lactose degrader shown as LOW (0.11%) under the food intolerances section on the Biomesight report.
There are some other findings here that disturb me, like butyrate producers LOW, colibactin producers HIGH, D-Lactate producers HIGH, gram negative bacteria HIGH and gram positive bacteria LOW.
Would you say that I fit on the classic ME/CFS profile? Anything else that stands out about my microbiome?
Thank you and I hope this format is easy to understand but if not, please let me know.
I avoid comment on any provider individual reports, i.e. Biomesight report, beyond what the US National Institute of Standards and Technology has stated. I will comment on methodologies, the usual comment is they “went cheap” and do not use sufficient data — MP consider 7,431,520 facts in computing suggestions.
Your sample have strong statistical associations to may symptoms of ME/CFS and Long COVID. “Fitting a profile” is question more suitable for a medical professional. I am a statistican.
Postscript – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I cannot tell people what they should take or not take. I can inform people items that have better odds of improving their microbiome as a results on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting.
Also, I note that many people will make inferences (often based on influencers opinions) that are not supported by the evidence. Often people want absolute certainty and will deem things proven if they find a single case study supporting a hypothesis; this is not how science and statistics work… it is all odds.
The answers above describe my logic and thinking and is not intended to give advice to this person or any one. Always review with your knowledgeable medical professional.
Recent Comments