This young man seem to have been thru every situation that results in Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), including Gulf War, Lyme, food poisoning etc…
Back Story
I have been pretty sick for a long time, and have a complex history of symptoms primarily consistent with classic Chronic Fatigue Syndrome/Gulf War Illness.
- 1972 born, probable over use of antibiotics in youth, family history of severe arthritis/rheumatism on fathers side.
- 1990, severe case of Herpes simplex one, caught while on high school wrestling team, immune system was depleted from cutting weight, no eating.
- 1991, military service in Army, in Iraq during Desert Shield/Storm, possible exposure to low doses of chemical/biological weapons
- 1992, tick bite in military in North Carolina, tick on body for several days before found
- 1994, first notice waking up with unusual mild joint pain/stiffness, mild fatigue (only 22 years old at the time)
- 1995, bad case of food poisoning, around this time begin having episodes of bad fatigue, also paresthesia
- 1995, severe chainsaw accident, around this time several episodes of severe full body paresthesia, lasting up to a week
- 1996, after a likely viral illness, for the first time develop severe, constant fatigue. Did 30 days of doxycycline, and slowly recovered over course of about 6 months
- 1996-2001- was very active during this time, extremely athletic, running and lifting weights to extreme levels. Did not eat well, drank quite a bit of alcohol. Began having periods of fatigue, joint pain, flu-like feeling) especially after exercise, also periods of irritability, and brain fog began around time had a mercury filling put in.
- 2001-had bad upper respiratory infection, was very sick, extreme coughing uncontrollably. Dropped out of graduate school.
- Doctor gave me antibiotics for what he thought was “bronchitis”. This triggered a huge reaction where I developed extreme fatigue, pain, paresthesia, anxiety, etc.…all symptoms manifested to the highest level I had ever experienced and remained constant. This was the period I would say I developed full on Chronic Fatigue Syndrome.
- 2002-doctor put me on 2 antibiotics, thought I could have Lyme disease. I improved significantly. But then had a bad accident and nearly cut off my finger. This caused a major relapse of all symptoms.
- 2004-Saw doctor and was put back on doxycycline long term again. Had some initial improvements, but plateaued, and relapsed fully after exercising too much one day.
- 2004-2009-symptoms continue to progress, and get worse after moving from Arizona to cooler, wet climate of western Washington state.
- 2009-new doctor put me on multiple antibiotics for over a year, again for possible Lyme disease. Does nothing, if anything makes me worse. New symptom now of facial acne.
- 2010-present, symptoms persist, and have some new ones. Test various supplements on my own, work with various alternative practitioners, with minimal benefit.
Basic Analysis
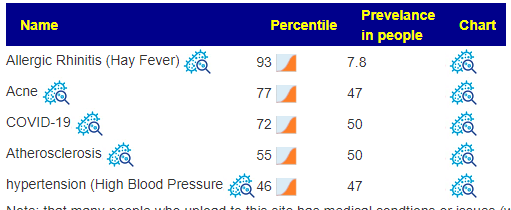
The list of potential medical conditions is relatively short:
- The “Bacteria Deemed Unhealthy” list was short with just one sticking out at 97%ile: Parabacteroides merdae.
- Dr. Jason Hawrelak Recommendations placed him at the 89%ile
This seems to be a milder version of another recent review (Severe gut dysbiosis, candida, SIBO): namely “normal appearing using classic criteria” but with a big spike in rare bacteria.
Using DNA (aka Kyoto Encyclopedia of Genes and Genomes )
When dealing with a lot of rare bacteria, you will usually encounter a void of literature on how to modify them. Using KEGG does not always come up with suggestions. I have seen a few samples where there was nothing suggested.
- RETAIL Probiotics is very similar to the (Severe gut dysbiosis, candida, SIBO) review cited above. I actually show
it’s value strikethroughfor comparison.- miyarisan (jp) / miyarisan –
907903 (clostridium butyricum) - enviromedica terraflora sbo probiotic –
812, 813 (bacillus clausii,bacillus coagulans, bacillus megaterium, bacillus pumilus, bacillus subtilis)
- miyarisan (jp) / miyarisan –
- Supplements – this is similar but much shorter list. The list lacks Magnesium, Molybdenum, Amylase, L-Lysine, L-Proline, L-Threonine.
- beta-alanine – Percentile:
1.51.5 - L-Cysteine – Percentile:
10.42 - L-glutamine – Percentile:
5.94.6 - L-Histidine – Percentile: NEW 6.8
- NADH – Percentile:
2.82.8
- beta-alanine – Percentile:
On to Suggestions
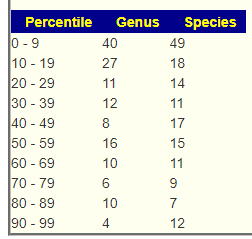
I am doing the same process as cited in (Severe gut dysbiosis, candida, SIBO) review The number of bacteria picked for each is shown below:
- Use JasonH (15 Criteria) – 8
- Use Medivere (54 Criteria) – 8
- Use Metagenomics (59 Criteria) – 8
- Use Nirvana/CosmosId (36 Criteria) – 8
- Use XenoGene (22 Criteria) – 8
- Standard Lab Ranges (+/- 2 Std Dev) – 6
- Box Plot Whisker – 20
- Kaltoft-Moltrup Normal Ranges – 86
- Percentile in top or bottom 10% – 160
These numbers seem to reflect “normal appearing using classic criteria” cited above.
Consensus Report
I just revised the consensus page this morning to make it easier to use. Added a page specific video. With all suggestions, it is important to remember that none guarantees improvement, rather each items increases the odds of improvement. You can pick and choose from the list as you wish — just keep to things with positive values. Things that you are taking now with a negative value, you should try to reduce or stop (factoring in medical needs). From the list, I picked the following items as likely easy to implement , available and reasonable costs.
- probiotics (note: these were also suggested from DNA)
- fruit/legume fibre
- walnuts, almonds/ almond skins
- Supplements:
- Glucomannan (a dietary fiber usually made from the root of the konjac plant – available as a supplement)
- Conjugated Linoleic Acid
- magnesium
- Herbs/Spices
- Turmeric
- Holy Basil (Neem)
- pomegranate, rhubarb (apple and rhubarb pie over the summer?)
- blueberry
- Cacao (i.e. 85% for higher chocolate)
In short: start each day with porridge made with barley or oats, serve with walnuts or blueberries. Meat, high-protein diet is a to be avoided, Mediterranean diet comes high.
Suggestions using Symptoms
This person entered symptoms so we can use that to generate one or more sets of suggestions. There are many ways of slicing/dicing the symptoms and there is nothing wrong with doing a lot of them and then using the consensus to get what is in common.
My first past used:
- Neuroendocrine Manifestations: intolerance of extremes of heat and cold
- Immune: Sensitivity to smell/food/medication/chemicals
| Rank | Name | Your value | Percentile |
|---|---|---|---|
| class | Fusobacteriia | 10 | 2.4 |
| family | Bifidobacteriaceae | 70 | 3 |
| family | Fusobacteriaceae | 10 | 2.2 |
| family | Proteinivoraceae | 30 | 19.4 |
| genus | Bifidobacterium | 60 | 3.5 |
| genus | Ethanoligenens 💥 | 350 | 84.2 |
| genus | Fusobacterium | 10 | 2.1 |
| genus | Sphingobacterium | 50 | 17.3 |
| order | Fusobacteriales | 10 | 2.5 |
| phylum | Fusobacteria | 10 | 2.3 |
I clicked on Ethanoligenens to see what decreases it, and compiled this list,
A second pass using just Condition: ME/CFS without IBS, resulted in an short ‘expected’ list – all of them were low
| Rank | Name | Your value | Percentile |
|---|---|---|---|
| family | Moraxellaceae | 20 | 19.5 |
| genus | Bifidobacterium | 60 | 3.5 |
| genus | Sarcina 💥 | 100 | 19.6 |
| order | Moraxellales Liao et al. 2020 | 20 | 19.5 |
| phylum | Actinobacteria | 170 | 0.4 |
| species | Adlercreutzia equolifaciens | 100 | 26.7 |
This approach can help you filter out the suggestions to ones that may help the symptoms that you are most concerned about. You need to be careful not to try fix all issues at one time — you want short course corrections.
Recent Comments