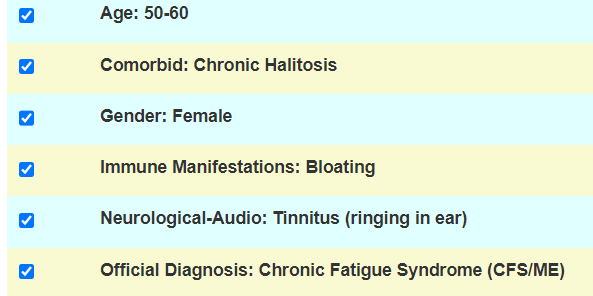
This is the son of a person with issues: Bad Diet and Antibiotics? ME/CFS like symptoms. As I have often cautioned, young people’s and children’s microbiomes are different than adults and we do not have appropriate reference ranges. We will do best efforts.
- Tired all the time
- Cannot gain weight (very skinny)
- Diagnosed with Marfan syndrome (a genetic disease he has since birth)
[editor] About 1 in 5,000 people have Marfan syndrome - Stomach pain
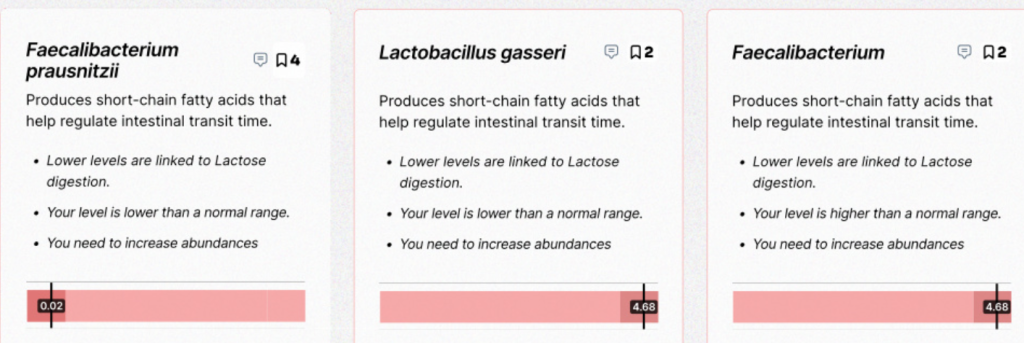
- Disgestion issues (yellow stool and fat in stool)
- Joint and Muscle pain
- Dark circles around the eyes
Analysis
There is no available literature on microbiome shifts with Marfan syndrome. Marfan syndrome (MFS) results from heterozygous mutations in the fibrillin-1 gene (FBN1; OMIM #134797), located on chromosome 15 at band q21. 1 (15q21. 1), which encodes for the glycoprotein fibrillin. [MedScape]. Coagulation plays a major role in Marfan syndrome. Both procoagulation and bleeding disorders participate in the disease. Platelet function abnormalities, compatible with von Willebrand syndrome or congenital thrombocytopathies, have been identified in 29% of patients. [2014].
FBN1 is the causative gene for Marfan syndrome, an inherited disorder of connective tissue whose major features include tall stature and arachnodactyly, ectopia lentis, and thoracic aortic aneurysm and dissection. More than one thousand individual mutations in FBN1 are associated with Marfan syndrome, making genotype-phenotype correlations difficult. [2016]
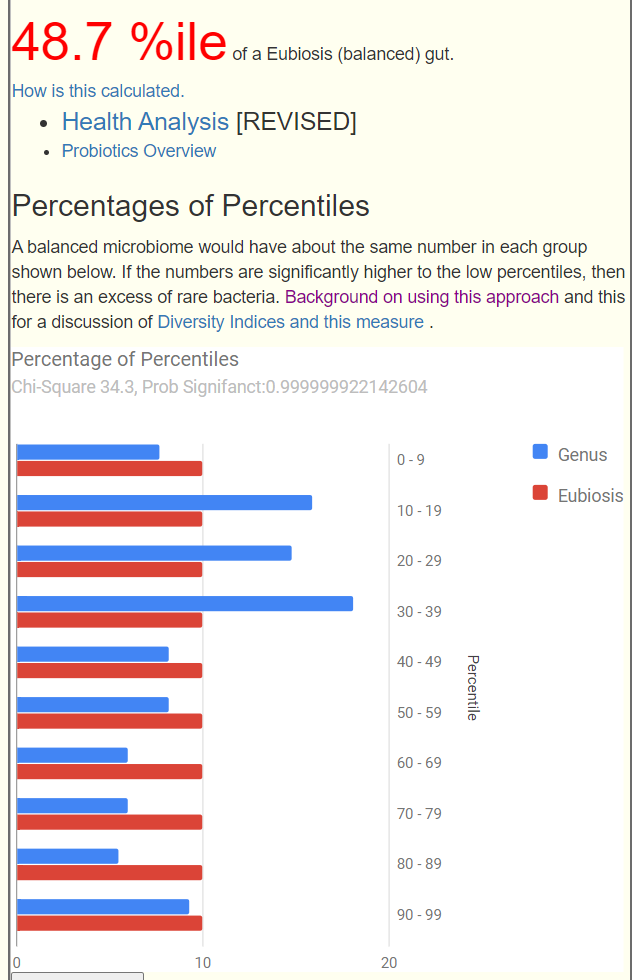
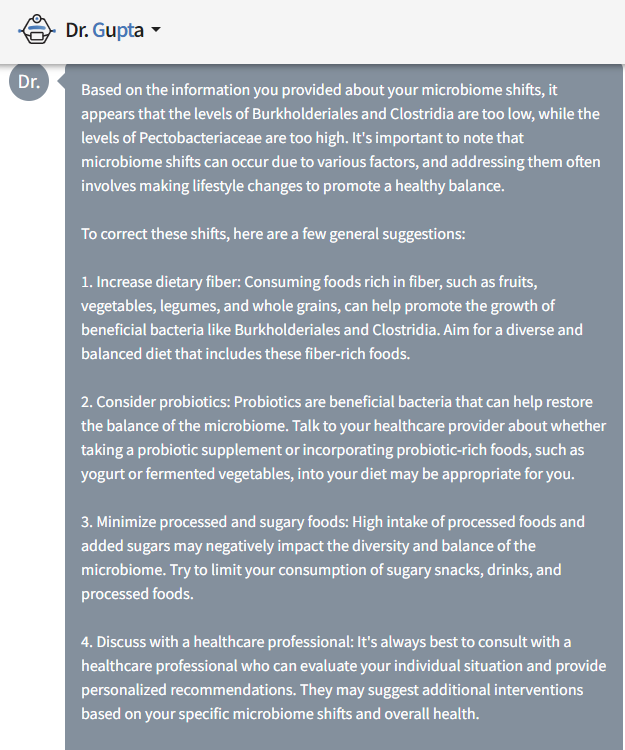
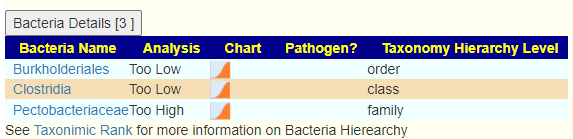
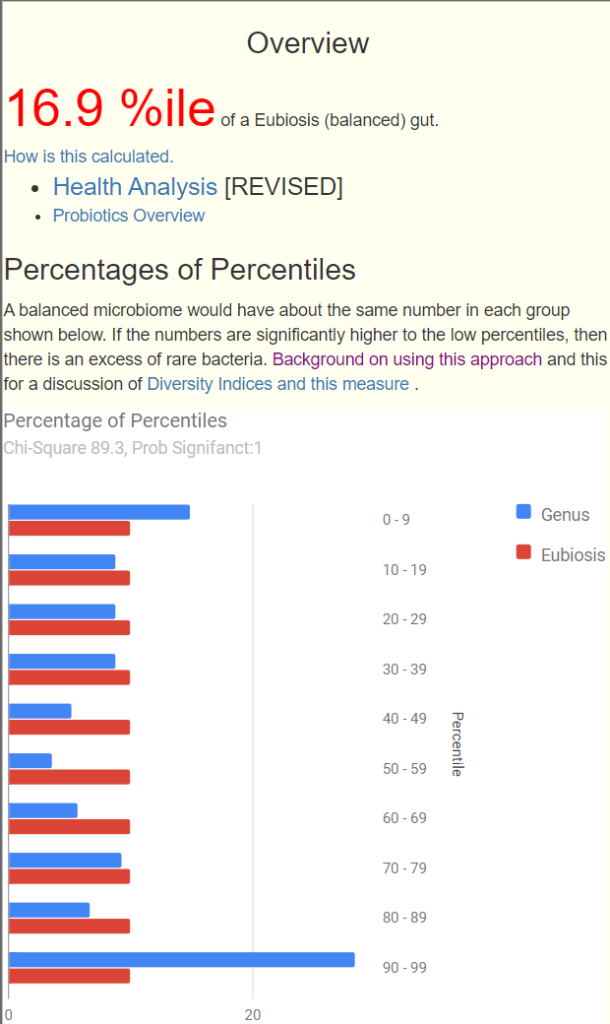
At a high level we see potential issues. [NOTE: The Eubiosis value changed for many people after a defect was detected in how percentile was computed for some bacteria – often 100% dropped, which how agrees with people symptoms ].
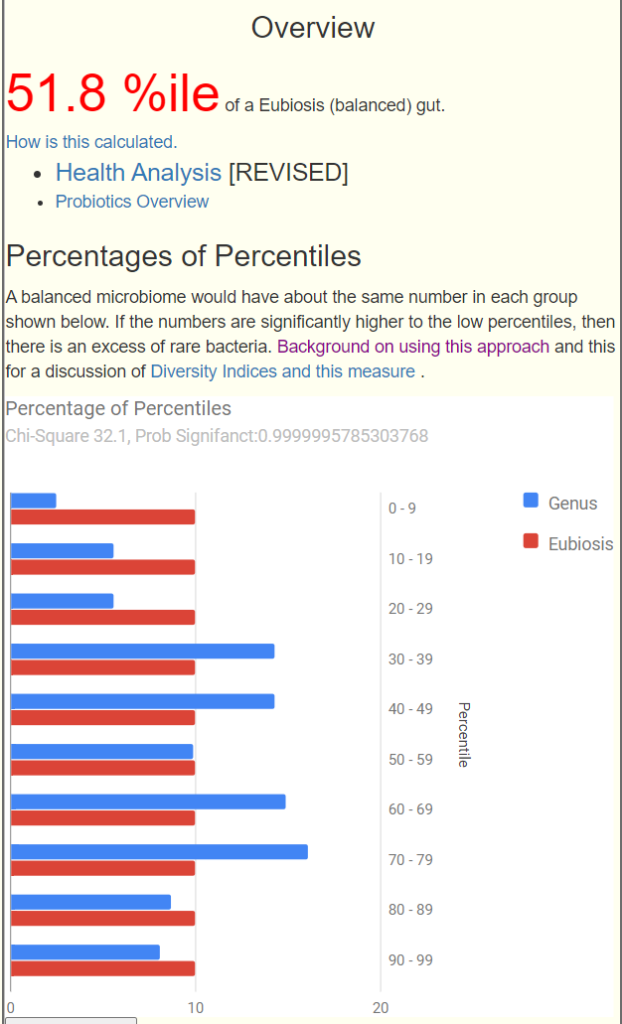
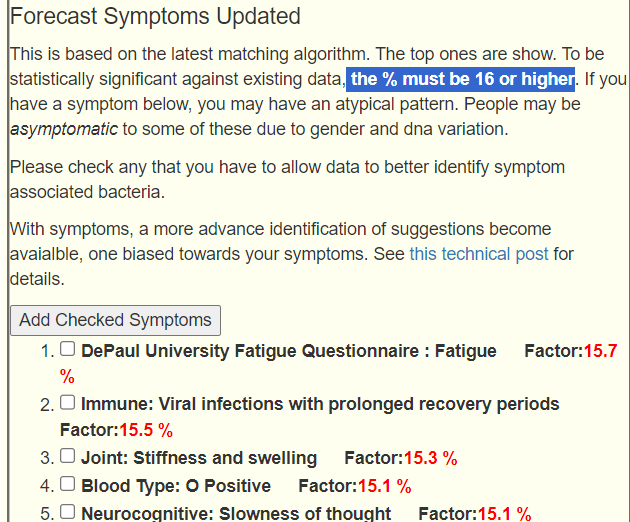
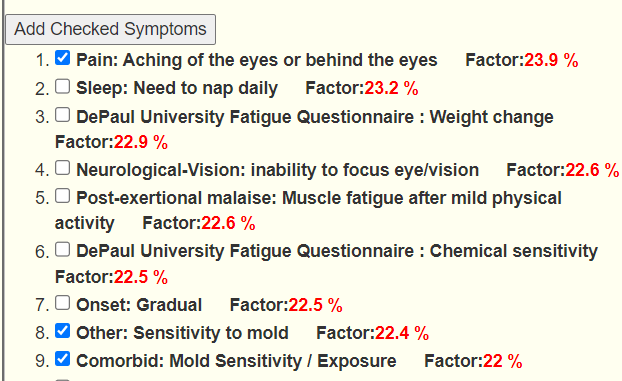
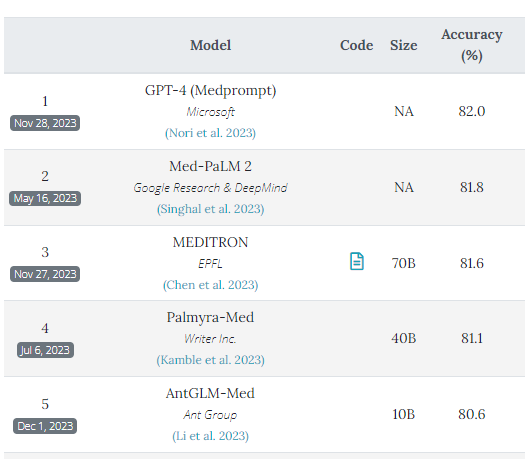
However, there were no statistically significant matches (this page was just updated to use the latest algorithm). This algorithm is similar to the Eubiosis algorithm. We compute the expected number of matches to bacteria shifts associated with the symptoms. The expected number by randomness is 16%. A higher number indicate increased odds, a lower number decreased odds. This is based on the existing annotated samples uploaded data. It is not definitive and often there can be multiple subsets of bacteria associated with a symptom. The match is on too much or too few of a collection of bacteria associated to symptoms.
We will still check the matching symptoms. The top one is a match for symptoms but not a match for the typical bacteria seen for this symptom. We have to hope that there is sufficient matches to be worth while.
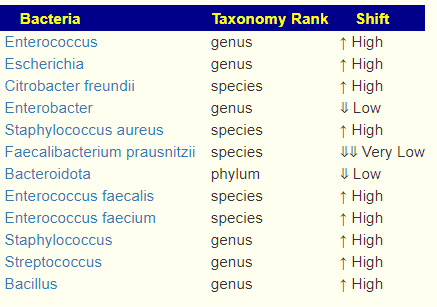
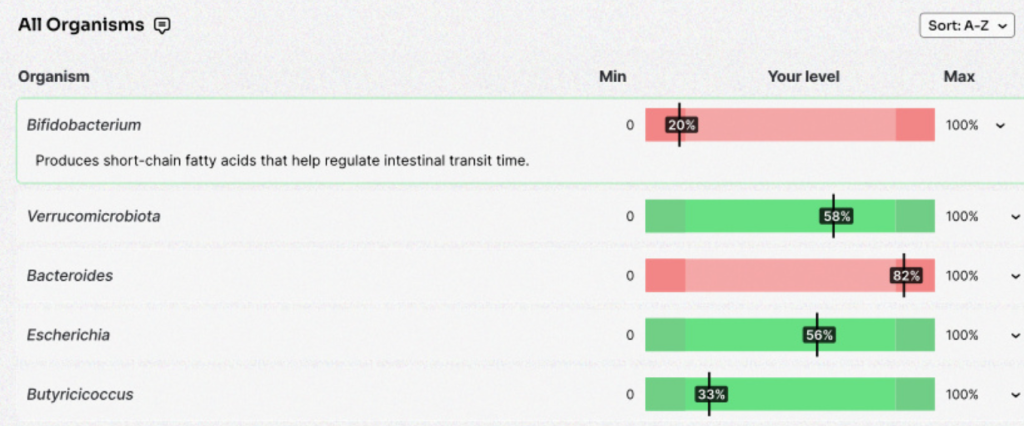
First, looking at all of the common, popular measuring sticks –
- General Health Predictors has a low number (just 8) with only one of possible concern: Veillonella atypica
- All of the usual ratios are between 20%ile and 80%ile
- Anti inflammatory Bacteria Score is at 89%ile — very good
- No Potential Medical Conditions Detected detected
- Histamine issues are a potential health issue
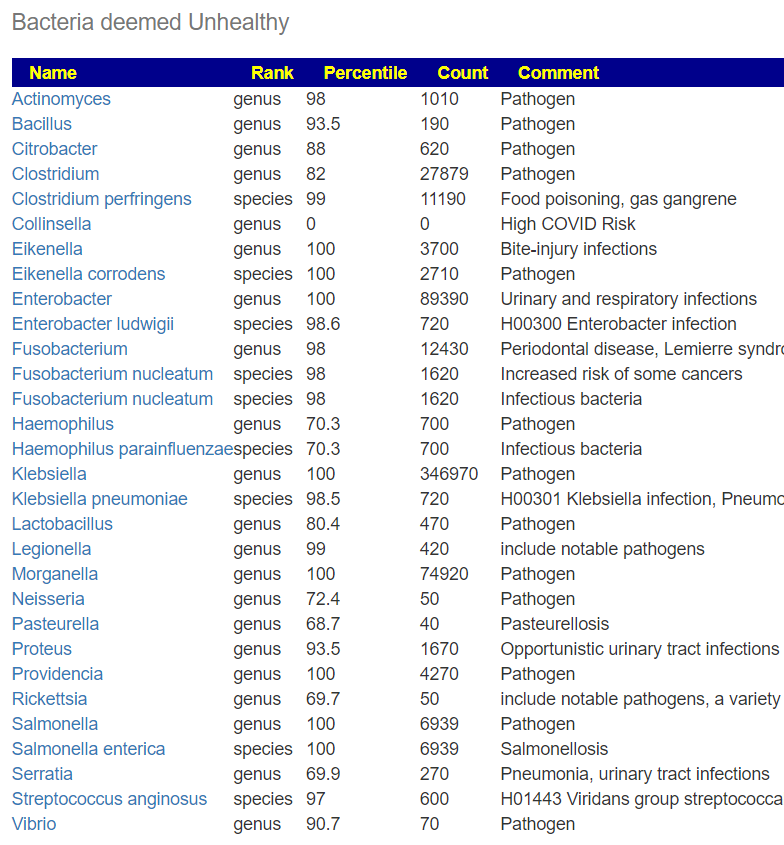
- Bacteria deemed Unhealthy: Bacteroides fragilis and Parabacteroides merdae are the only one, both are potentially infectious bacteria.
- Dr. Jason Hawrelak Recommended Levels came in at 94%ile
So, everything looks like a reasonably healthy person.
Going Forward
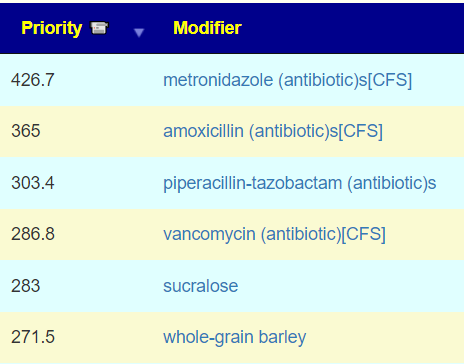
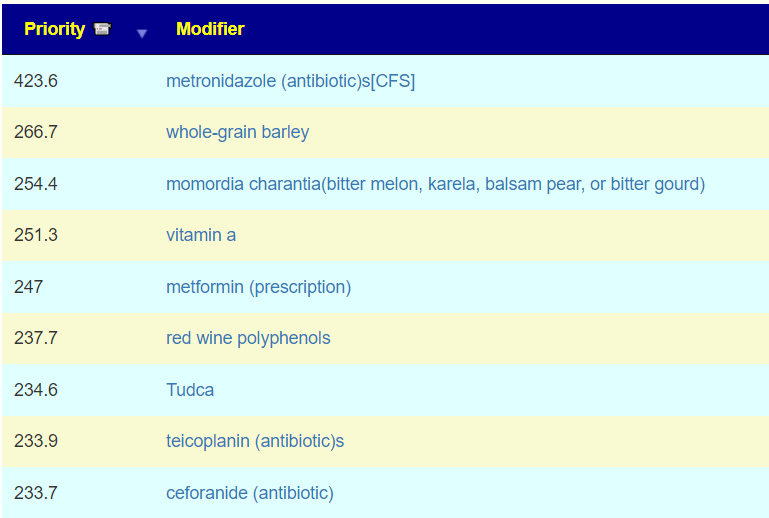
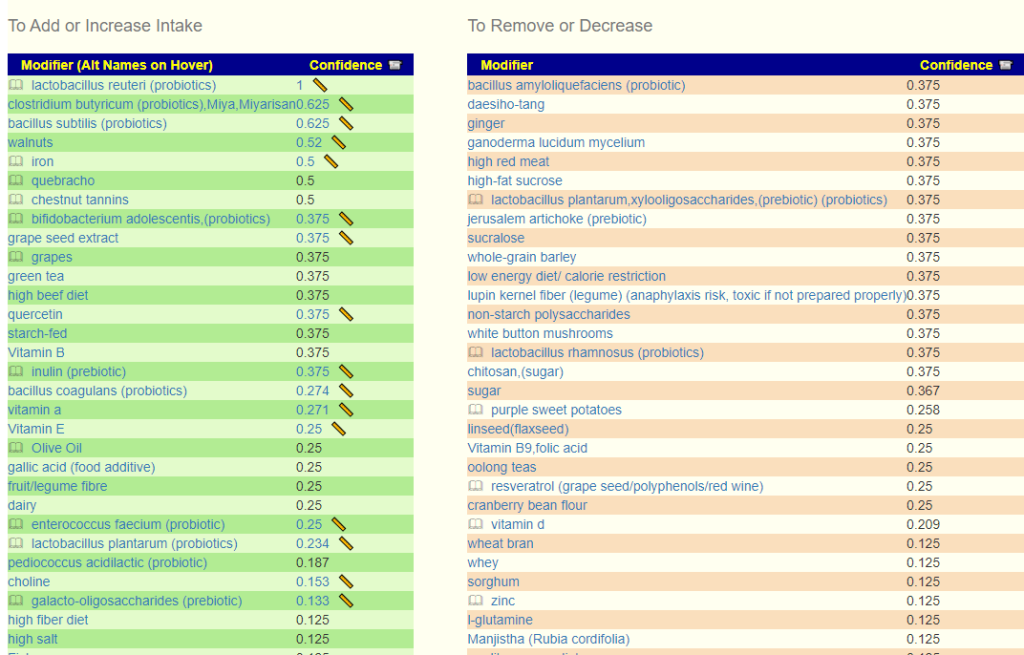
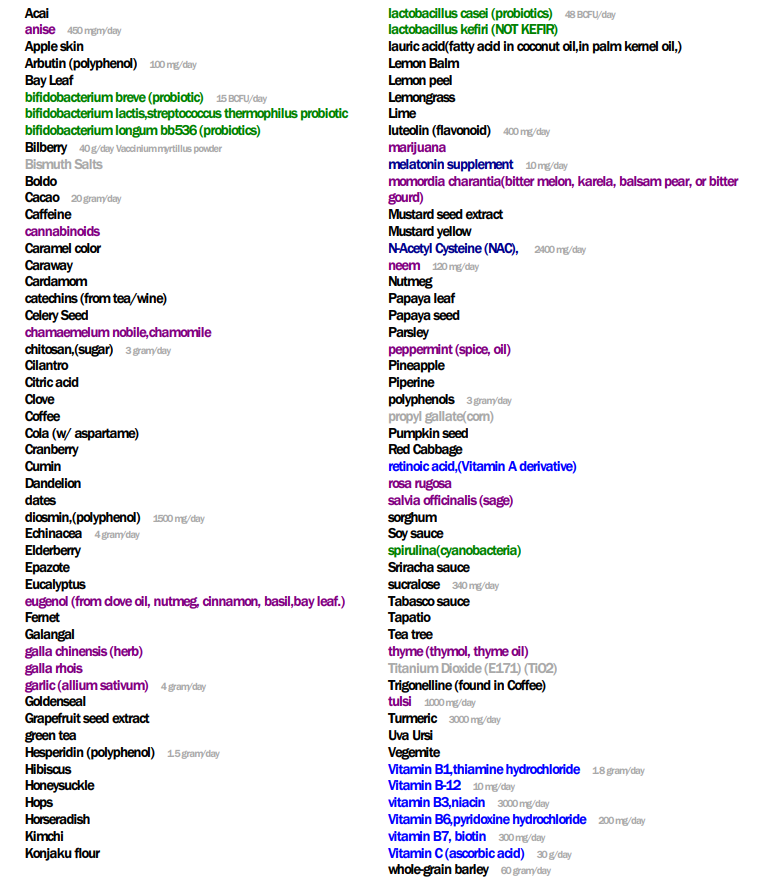
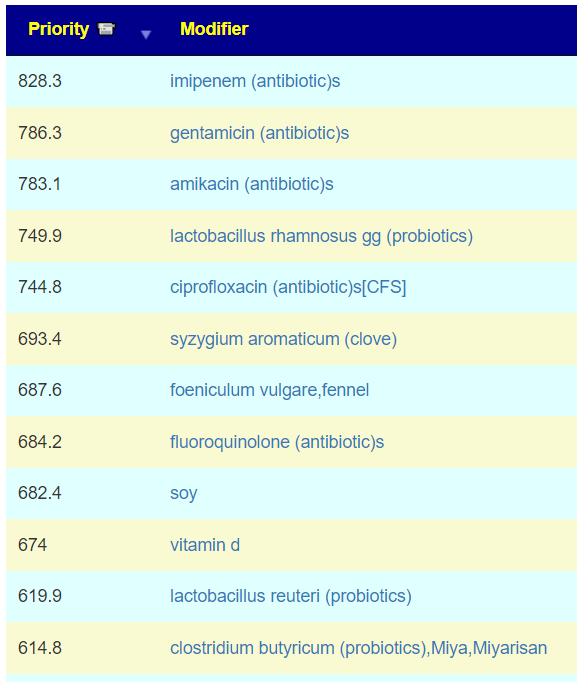
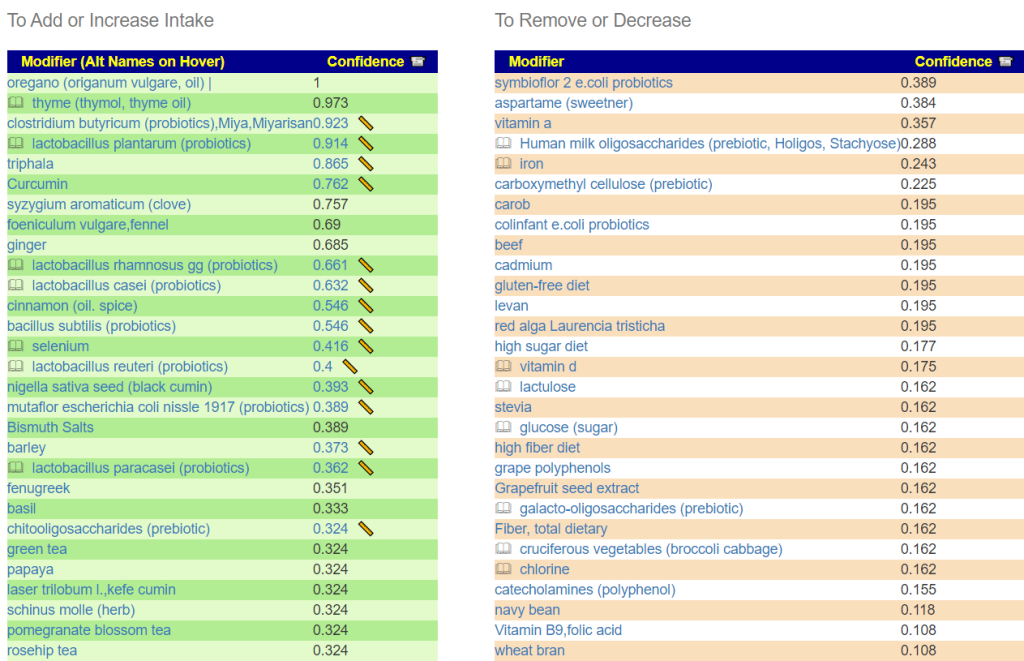
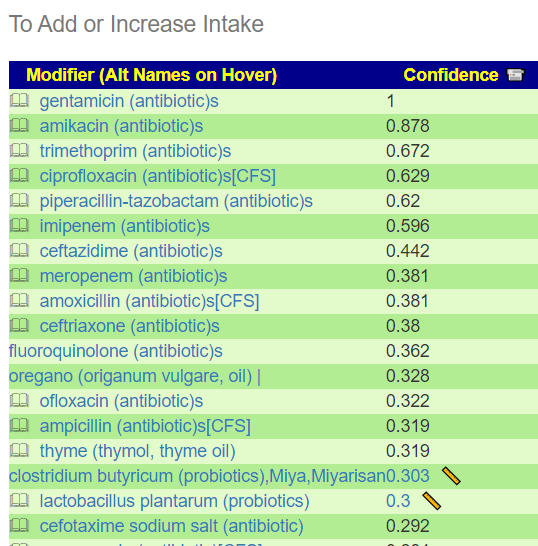
With no clear issue associations, we are going to do two runs: One with symptoms and one without.. Using the standard ‘Just give me Suggestions’ The list below are for the items at a priority of 50% or more of the highest priority [506] [Symptoms: 440]. This limit has no rationale apart from reducing the volume of suggestions.
Suggestions
- polyphenols:
- Hesperidin (polyphenol)
- Arbutin (polyphenol)
- diosmin,(polyphenol)
- luteolin (flavonoid)
- Guaiacol (polyphenol)
- mannooligosaccharide (prebiotic) — Coffee is rich in them! as are chickpeas, lentils, and peas
- Herb and Spices – Nothing in range, highest was ginger
- Diet Style — last time nothing made it above the cut, that is no longer the case, two made it above the line
- Amino Acid – nothing last time
- l-glutamine made it above the cut
- Foods –
- Caffeine (Coffee, Tea etc)
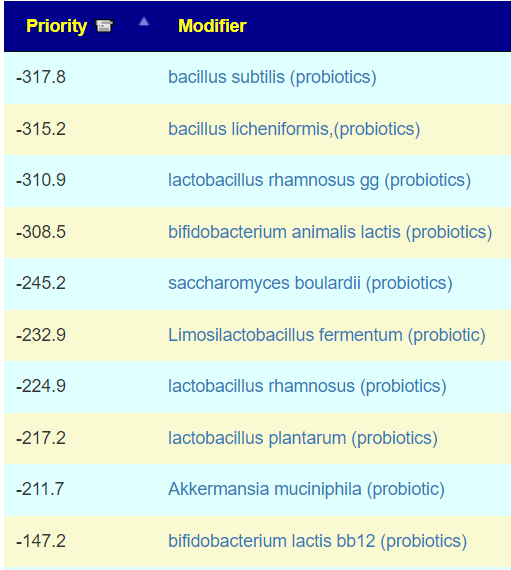
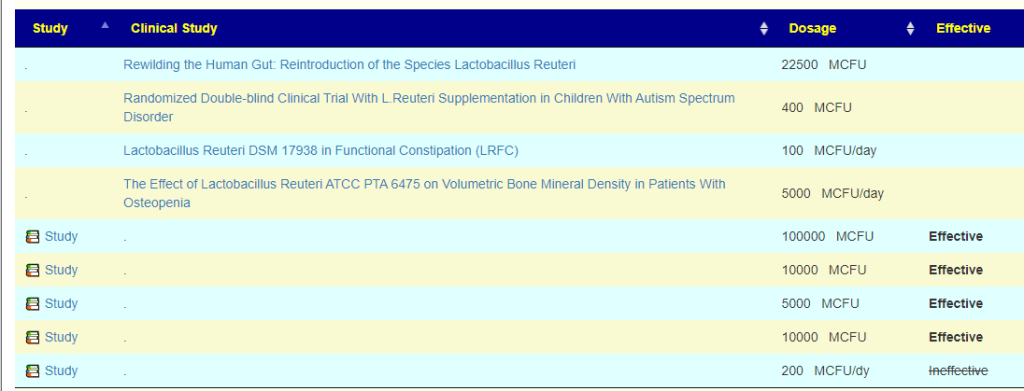
- Probiotics Nothing over 250
- Sugars – nothing in range, sucralose was highest
- Vitamins
- The usual B vitamins B1,B3,B6,B7,B9,B12
- WARNING: Make sure you are doing therapeutic dosages of these, See Supplement Dosages.
- Vitamin B Mitigates Thoracic Aortic Dilation in Marfan Syndrome Mice by Restoring the Canonical TGF-β Pathway [2021]
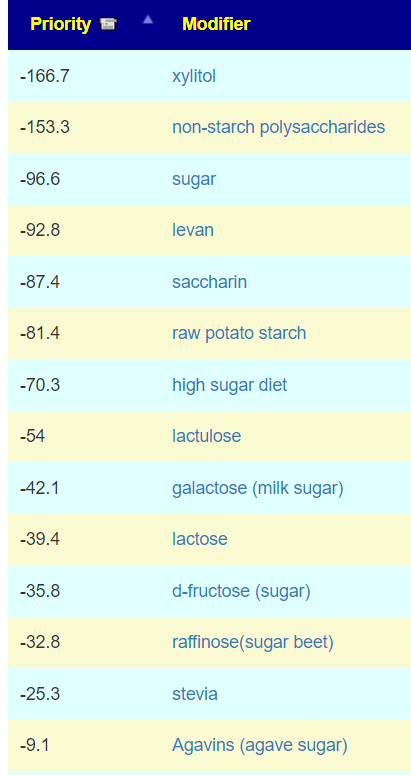
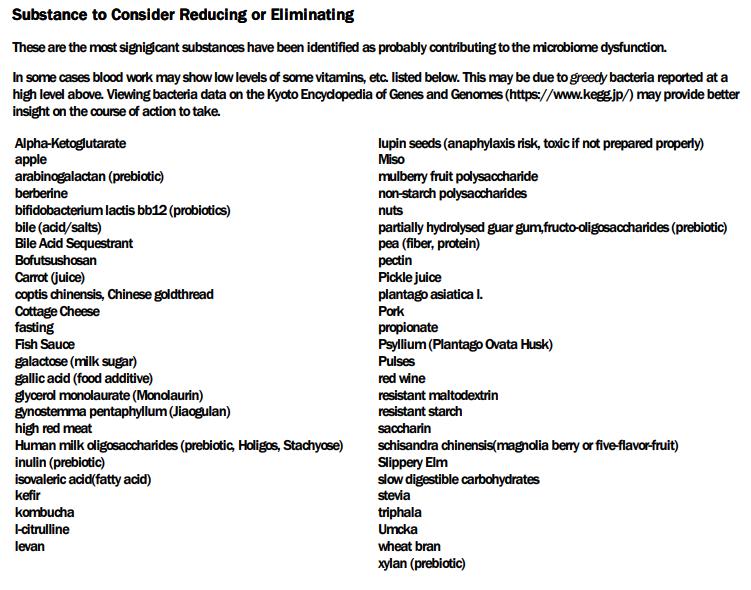
Let us look at AVOIDS, given the general healthy state, just try reducing if taking,
- inulin (prebiotic), arabinogalactan (prebiotic), fructo-oligosaccharides (prebiotic), Human milk oligosaccharides (prebiotic, Holigos, Stachyose)
- fasting, ketogenic diet, fibre-rich macrobiotic ma-pi 2 diet (which agrees with item above and below)
- wheat bran and grains containing gluten, barley, whole grain,bran
- Pulses
- black raspberries, pomegranate, almonds/ almond skins
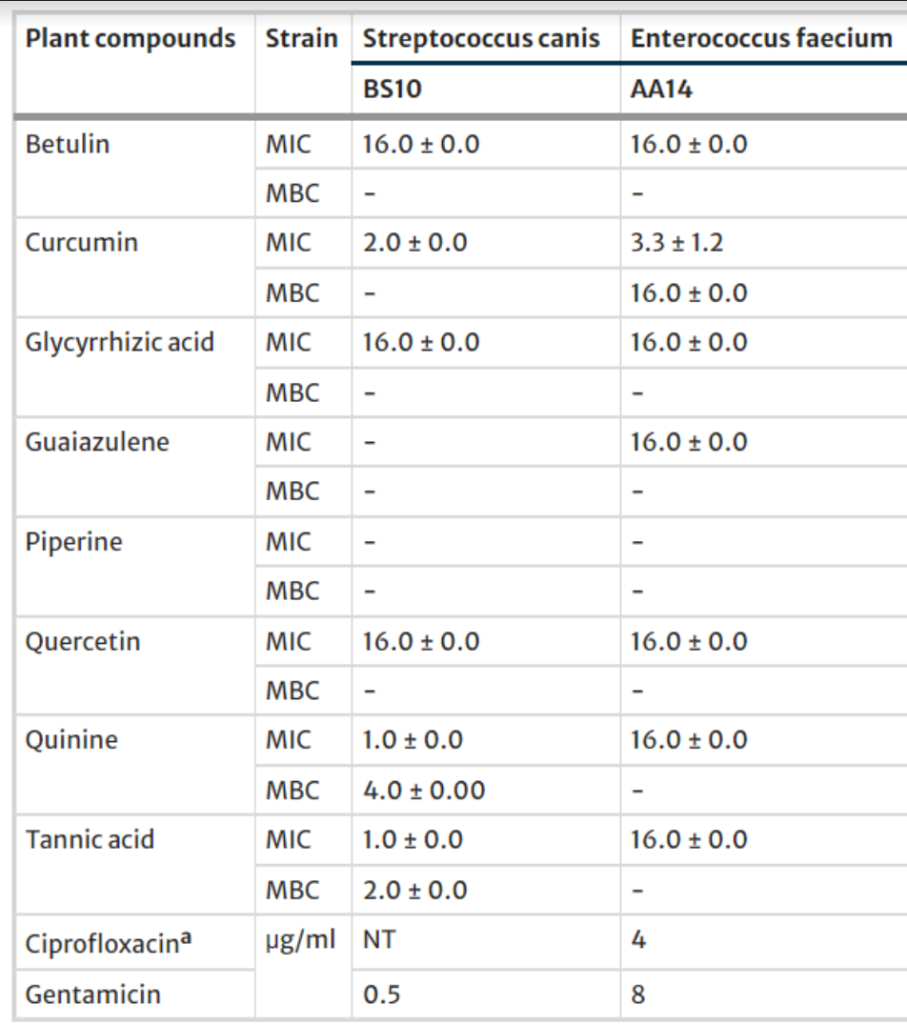
- Moringa Oleifera, Slippery Elm, berberine
- Pork
- Olive Oil — use Safflower Oil instead
- Conjugated Linoleic Acid (CLA)
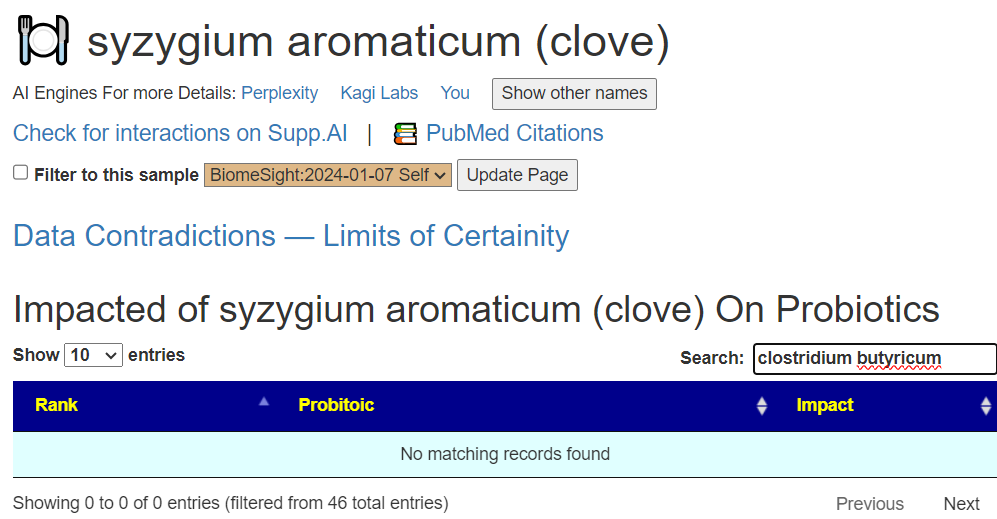
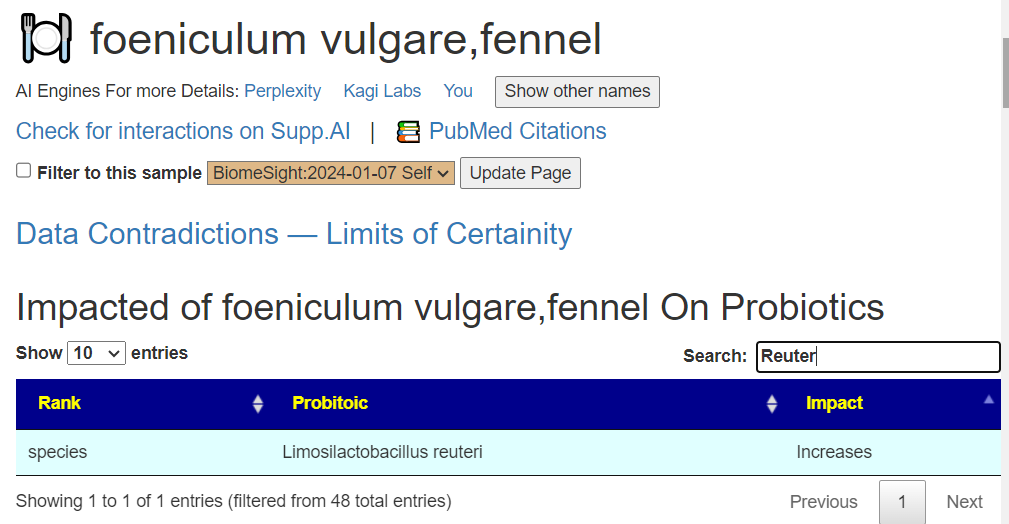
- Most probiotics! See below!!
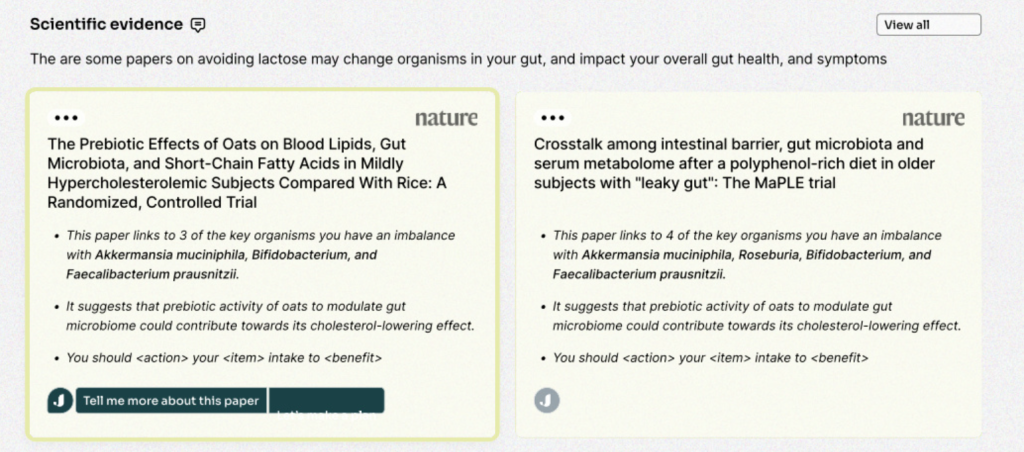
At this point, I attempted to do cross validation: Are there any literature of items suggested (or avoid) on improving Marfan syndrome. This is done to test the suggestions – for other conditions with lots of literature, we have usually seen 90-95% agreement. For ME/CFS, I know the literature well — for this condition, not. I found only symptom treatment (Mayo, NHS). Since this is a DNA condition and I know DNA can influence the microbiome (and the reverse), then trying to improve towards typical this youth’s microbiome is a reasonable (and low risk) approach.
Because of the platelet function abnormalities that could be present, as well as thick blood (procoagulation) — both areas that I am familiar with from ME/CFS. I checked suggestions for possible items that could be related to coagulation:
- Vitamin K — Nothing
- resveratrol (grape seed/polyphenols/red wine), grape polyphenols, grape seed extract, grapes — both negative
- Conjugated Linoleic Acid – negative
Questions and Answers
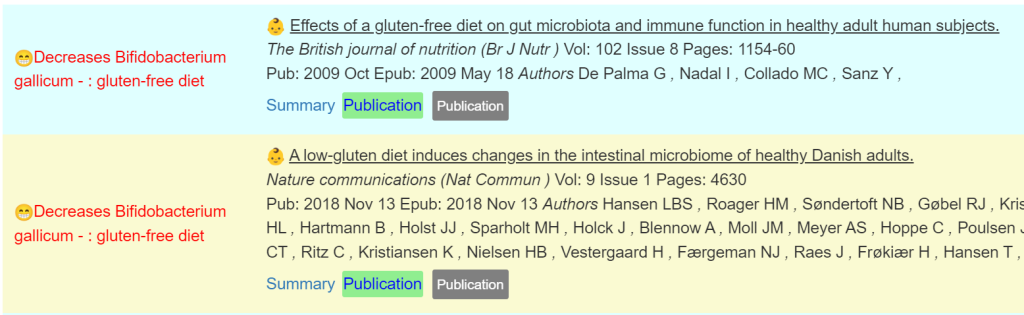
Q: Do you know why it suggest gluten Free diet? Could he have gluten intolerence/celiac maybe?
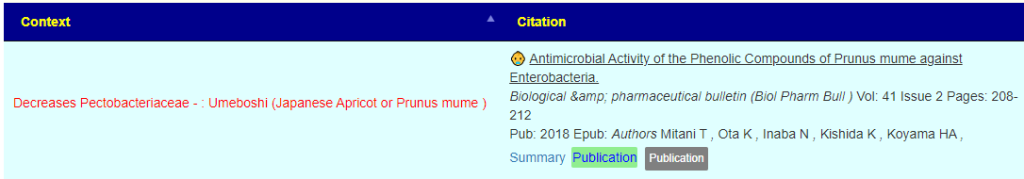
- The why is because of that type of diet impacts on bacteria that are off balance. We cannot detect gluten intolerance/celiac. Only the impact of that type of diet on different bacteria. Some source papers to illustrate:
Bottom Line
The thing that strikes me most about the suggestions, the items to avoid are prebiotics and probiotics; the opposite of common advice for anyone with health issue, especially digestive issues. There are no studies on PubMed for probiotics and this condition which infers to me (given the popularity of trying probiotics) that there were studies with no effect or negative effect. In the sparse literature, we did have one of the take suggestions computing matching the literature.
If this was my own child, I would likely follow the items in suggestions above. There is low risk in following them and one suggestion does cross-validate with the available literature (which has almost nothing published in this area).
I work off the axiom that a disease or conditions modifies the microbiome to be favorable to the condition. Undoing those shifts have a reasonable change of slowing, and in some cases, reversing the condition. I have had antidotal reports of this approach speeding cancer treatment.
Postscript – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I cannot tell people what they should take or not take. I can inform people items that have better odds of improving their microbiome as a result on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting.
The answers above describe my logic and thinking and is not intended to give advice to this person or anyone. Always review with your knowledgeable medical professional.








Recent Comments